- Department of Neurosurgery, Tohoku University Graduate School of Medicine, Tohoku University, Japan.
- Department of Neurosurgical Engineering and Translational Neuroscience, Graduate School of Biomedical Engineering, Tohoku University, Japan.
- Department of Neurosurgical Engineering and Translational Neuroscience, Tohoku University Graduate School of Medicine, Japan.
- Department of Diagnostic Radiology, Tohoku University Graduate School of Medicine, Sendai, Miyagi, Japan.
Correspondence Address:
Kuniyasu Niizuma
Department of Neurosurgery, Tohoku University Graduate School of Medicine, Tohoku University, Japan.
DOI:10.25259/SNI_735_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yoshimichi Sato1, Kuniyasu Niizuma1,2,3, Hideki Ota4, Hidenori Endo1, Teiji Tominaga1. Basilar artery dissection with rupture 6 years after accidental detection: A case report. 05-Jan-2021;12:4
How to cite this URL: Yoshimichi Sato1, Kuniyasu Niizuma1,2,3, Hideki Ota4, Hidenori Endo1, Teiji Tominaga1. Basilar artery dissection with rupture 6 years after accidental detection: A case report. 05-Jan-2021;12:4. Available from: https://surgicalneurologyint.com/surgicalint-articles/10511/
Abstract
Background: Chronic basilar artery dissection (BAD) is a rare pathology, and only a few reports have been mentioned in the literature. The imaging features of chronic BAD, especially those that develop into a subarachnoid hemorrhage (SAH), are unknown.
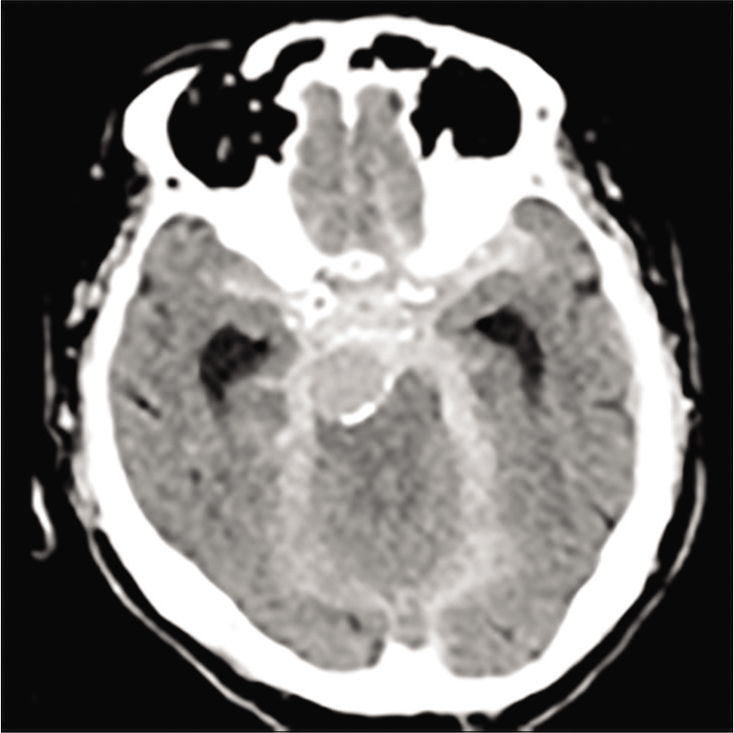
Case Description: We report a unique case of a chronic BAD with a split intimal flap that developed into an SAH. A 74-year-old man was diagnosed with BAD. After considering all treatment options, conservative treatment was selected for the patient. We continued imaging follow-up of the patient in our outpatient clinic once a year. The BA gradually dilated and the internal flap split. The patient and his family refused surgical treatment; therefore, conservative treatment was continued. Six years and 2 months from the first diagnosis, he developed a massive SAH and died.
Conclusion: In the case of this patient, the weakened condition of the internal elastic lamina may have caused dissection of the intimal flap between the intima and media. Furthermore, the dissection may have developed and connected the true lumen to the pseudolumen and induced BA rupture. Thereby, split of the internal flap could be a risk factor for rupture in chronic BAD.
Keywords: Basilar artery, Dissection, Intimal flap
INTRODUCTION
Basilar artery dissection (BAD) is a rare, but significant disorder. Ruecker et al. reported that BAD accounted for 1% of all cases of subarachnoid hemorrhage (SAH), and no <10.5% and 4.5% of posterior circulation and overall cranial vessel dissections, respectively.[
The clinical presentations of BAD are various. Large dissections may narrow the artery and can cause intra-arterial clots. Potentially, the intra-arterial clots and arterial stenosis caused by BAD can interrupt blood flow and cause ischemic stroke.[
Furthermore, the enlargement of the arterial diameter due to dissection can cause brainstem compression.[
Patients presenting with ruptured BAD have high mortality.[
Here, we report a unique case of a chronic BAD with a split intimal flap that developed into a massive SAH and discuss the risk factors for rupture in chronic BAD cases.
CASE DESCRIPTION
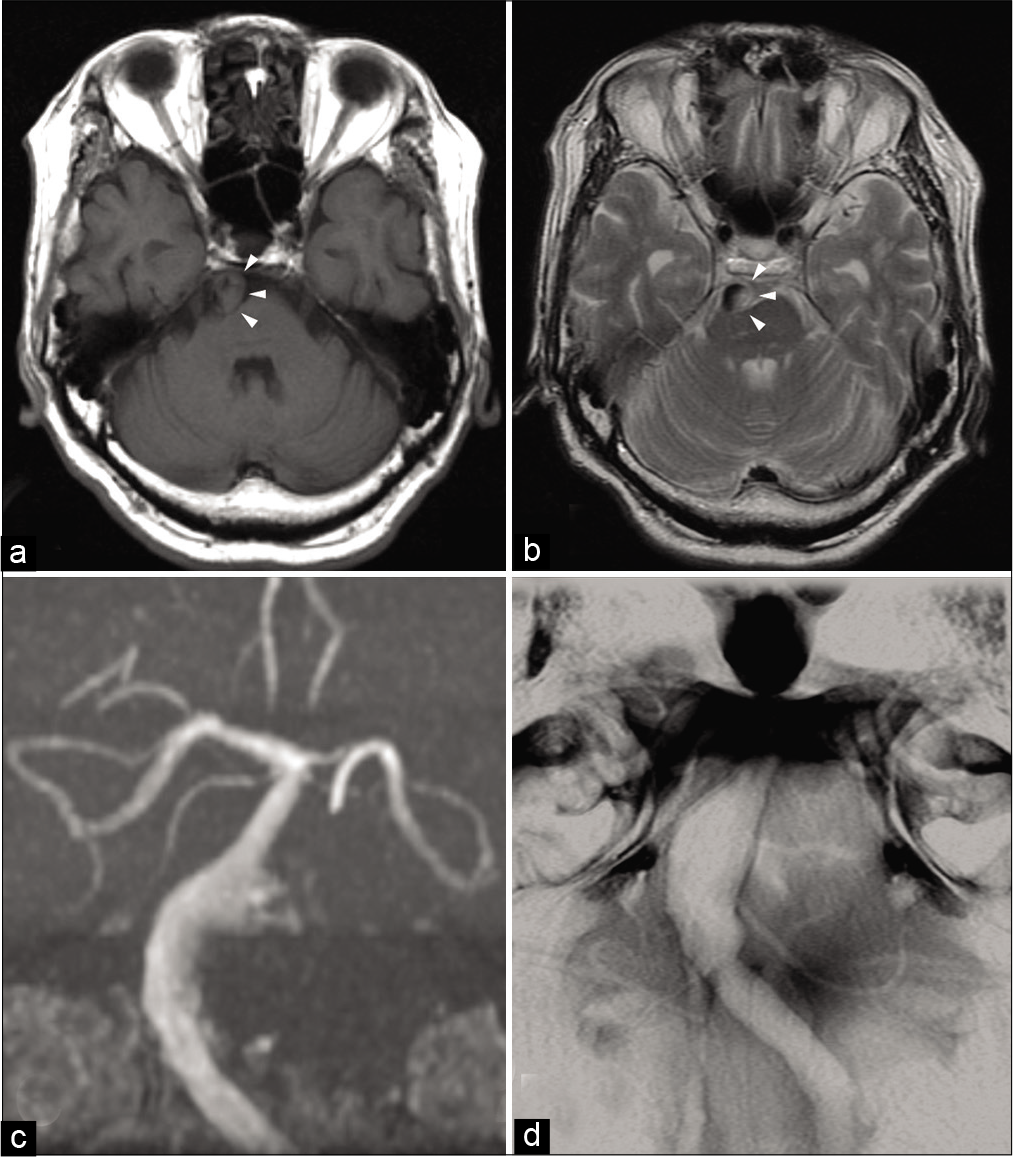
A 74-year-old man complaining of mild right hemiparesis was referred to our hospital. He had a history of atrial fibrillation, multiple neuromas, and an infarction in the right corona radiate due to severe stenosis of the right middle cerebral artery and had left hemiparesis since then. Neither computed tomography nor magnetic resonance imaging (MRI) demonstrated any ischemic or hemorrhagic lesions in the brainstem. However, MRI demonstrated thickened vessel wall of the BA with isointense appearance on T1-weighted and hyperintense appearance on T2-weighted images, indicating intramural hematoma [
Figure 1:
Magnetic resonance imaging (MRI) findings obtained on admission. Axial T1-weighted (a) and T2-weighted (b) MRI showing a narrowed eccentric flow void surrounded with intramural hematoma (arrowhead) that expands the basilar artery diameter. MR angiography (c) and basi-parallel anatomical scanning (d) showing focal dilatation of the basilar artery.
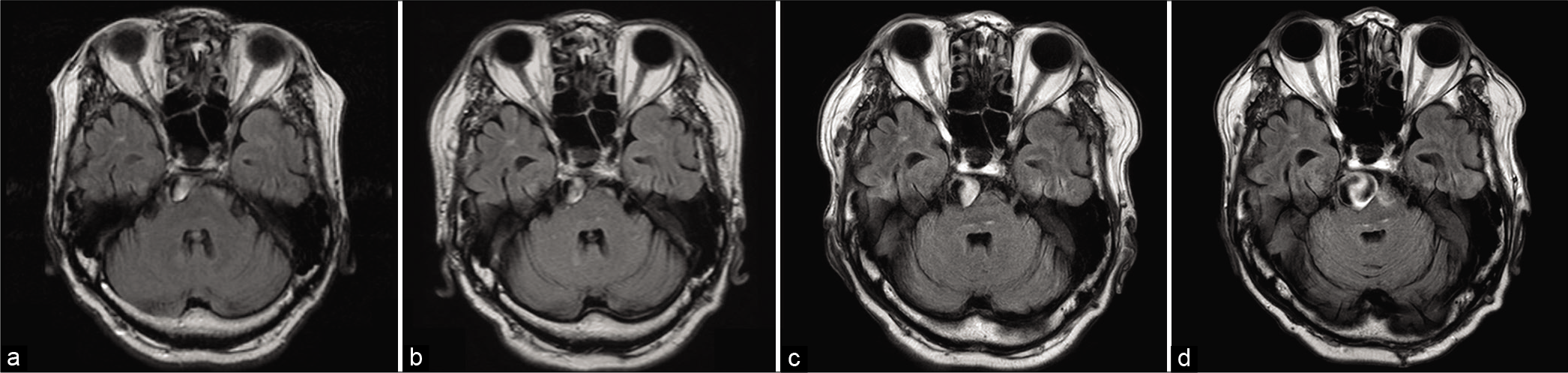
Yearly follow-up MR examinations demonstrated gradual aneurysmal enlargement of the BA [
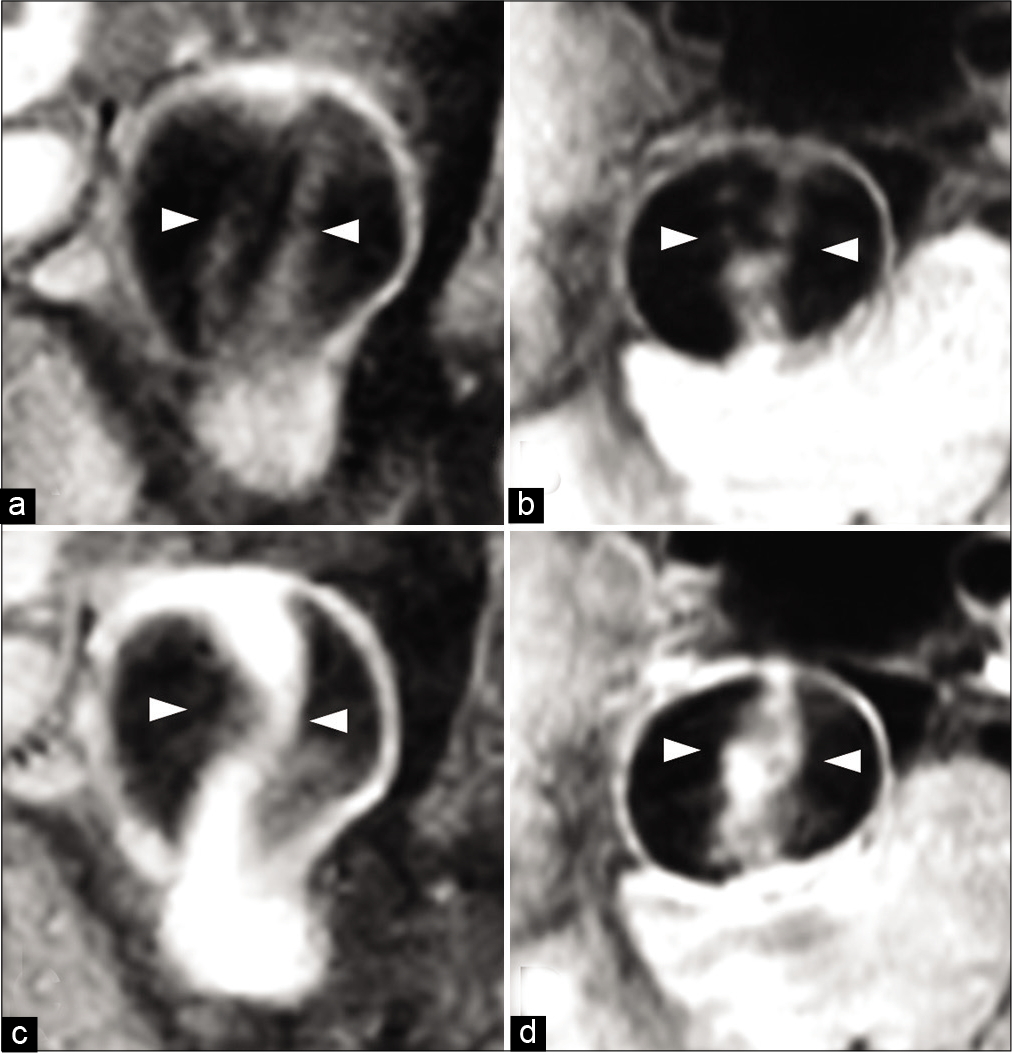
Figure 3:
Magnetic resonance imaging (MRI) findings 6 years from the first diagnosis. Coronal (a) and axial (b) noncontrast volumetric isotropic turbo spin echo acquisition (VISTA) MRI and coronal (c) and axial (d) contrast VISTA MRI showing blood flow in the pseudolumen and changes in image findings of the intimal flap with enhancement. The intimal flap looks like it split into two (arrowhead).
DISCUSSION
In the present case, the patient was stable in the acute phase and was symptomatically stable; however, he developed SAH in the chronic phase and died. The imaging features of chronic BAD that develops into SAH are not well-known. In our case, gradually dilating BA, enhancement in the BA wall, and intimal flap appearance of a split were observed. These imaging features may be considered as risk factors for rupture in chronic BAD.
Mizutani described the tortuous dilating basilar artery as a risk factor for poor prognosis.[
Several studies indicated that aneurysm wall enhancement could identify unstable aneurysms.[
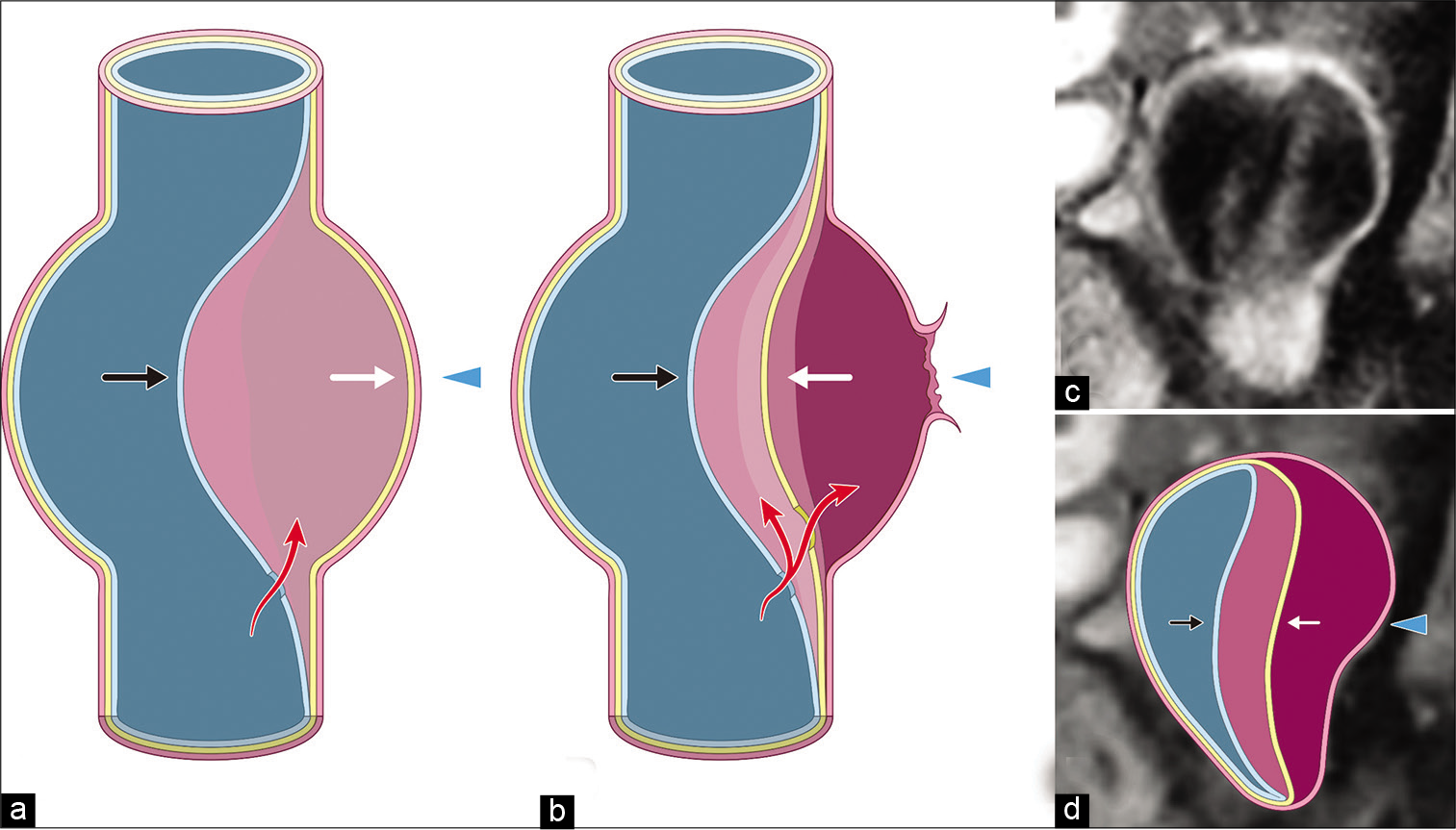
On the other hand, splitting of the intimal flap has never been reported as a risk factor. In our case, the initial intimal flap may have been formed within the intima. The reason why the intimal flap split is unknown. However, the weakened condition of the media may have caused dissection between the media and adventitia [
Figure 5:
Illustration of the hypothesis of the split intimal flap (a and b). First, the blood flow into the space between the adventitia (arrowhead), media (white arrow), and intima (black arrow). Next, the weakened condition of the media may cause dissection between the media and adventitia and induce rupture. Coronal noncontrast volumetric isotropic turbo spin echo acquisition magnetic resonance imaging (c) with the illustration of the hypothesis in this case (d) image of the adventitia (white arrowhead), media (white arrow), and intima (black arrow).
Surgical clipping and wrapping, endovascular treatment, and conservative treatment have been used for the management of BAD.[
CONCLUSION
We found a split of the intimal flap in a case of chronic BAD followed by lethal SAH. This imaging feature may be a new risk factor for rupture in chronic BAD. Further studies are needed to reveal the significance of this imaging feature of chronic BAD.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ali MJ, Bendok BR, Tella MN, Chandler JP, Getch CC, Batjer HH. Arterial reconstruction by direct surgical clipping of a basilar artery dissecting aneurysm after failed vertebral artery occlusion: Technical case report and literature review. Neurosurgery. 2003. 52: 1475-80
2. Chalouhi N, Hoh BL, Hasan D. Review of cerebral aneurysm formation, growth, and rupture. Stroke. 2013. 44: 3613-22
3. Cohen JE, Moscovici S, Rajz G, Vargas A, Itshayek E. Chronic basilar artery dissection with an associated symptomatic aneurysm presenting with massive subarachnoid hemorrhage. J Clin Neurosci. 2016. 30: 146-8
4. Edjlali M, Guédon A, Hassen WB, Boulouis G, Benzakoun J, Rodriguez-Régent C. Circumferential thick enhancement at vessel wall mri has high specificity for intracranial aneurysm instability. Radiology. 2018. 289: 181-7
5. Kim BM, Suh SH, Park SI, Shin YS, Chung EC, Lee MH. Management and clinical outcome of acute basilar artery dissection. AJNR Am J Neuroradiol. 2008. 29: 1937-41
6. Masson C, Krespy Y, Masson M, Colombani JM. Magnetic resonance imaging in basilar artery dissection. Stroke. 1993. 24: 1264-6
7. Mizutani T. A fatal, chronically growing basilar artery: A new type of dissecting aneurysm. J Neurosurg. 1996. 84: 962-71
8. Nakahara T, Satoh H, Mizoue T, Kawamoto H, Kohmo Y, Kurisu K. Dissecting aneurysm of basilar artery presenting with recurrent subarachnoid hemorrhage. Neurosurg Rev. 1999. 22: 155-8
9. Nakajima H, Ishiguro T, Komiyama M. Basilar artery dissection presenting with subarachnoid hemorrhage: Report of two cases. NMC Case Rep J. 2015. 2: 97-100
10. Nakatomi H, Nagata K, Kawamoto S, Furusho JI. Basilar artery occlusion due to spontaneous basilar artery dissection in a child. Acta Neurochir (Wien). 1999. 141: 99-104
11. Omodaka S, Endo H, Niizuma K, Fujimura M, Inoue T, Endo T. Circumferential wall enhancement in evolving intracranial aneurysms on magnetic resonance vessel wall imaging. J Neurosurg. 2019. 131: 1262-8
12. Pozzati E, Andreoli A, Padovani R, Nuzzo G. Dissecting aneurysms of the basilar artery. Neurosurgery. 1995. 36: 254-8
13. Raychaudhuri R, Yu W, Hatanpaa K, Cavuoti D, Pride GL, White J. Basilar artery dissection treated by neuroform stenting: Fungal stent infection. Surg Neurol. 2009. 71: 477-80
14. Ruecker M, Furtner M, Knoflach M, Werner P, Gotwald T, Chemelli A. Basilar artery dissection: Series of 12 consecutive cases and review of the literature. Cerebrovasc Dis. 2010. 30: 267-76
15. Sonobe S, Yoshida M, Niizuma K, Tominaga T. Ruptured basilar artery dissection diagnosed using magnetic resonance vessel wall imaging and treated with coil embolization with overlapping LVIS stents: A case report. NMC Case Rep J. 2020. 7: 75-9
16. Wang GX, Gong MF, Zhang D, Lei S, Yin JB, Gong ZL. Wall enhancement ratio determined by vessel wall MRI associated with symptomatic intracranial aneurysms. Eur J Radiol. 2019. 112: 88-92
17. Yoshimoto Y, Hoya K, Tanaka Y, Uchida T. Basilar artery dissection. J Neurosurg. 2005. 102: 476-81