- Department of Neurosurgery, Kurashiki Central Hospital, Kurashiki, Japan.
Correspondence Address:
Hiroyuki Ikeda, Department of Neurosurgery, Kurashiki Central Hospital, Kurashiki, Japan.
DOI:10.25259/SNI_948_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mai Tanimura, Hiroyuki Ikeda, Toshio Fujiwara, Minami Uezato, Takuya Osuki, Masanori Kinosada, Yoshitaka Kurosaki, Masaki Chin. Basilar artery occlusion due to vertebral artery injury treated with thrombectomy and distal vertebral artery embolization through the unaffected side. 12-Jan-2024;15:12
How to cite this URL: Mai Tanimura, Hiroyuki Ikeda, Toshio Fujiwara, Minami Uezato, Takuya Osuki, Masanori Kinosada, Yoshitaka Kurosaki, Masaki Chin. Basilar artery occlusion due to vertebral artery injury treated with thrombectomy and distal vertebral artery embolization through the unaffected side. 12-Jan-2024;15:12. Available from: https://surgicalneurologyint.com/surgicalint-articles/12702/
Abstract
Background: There is no established opinion regarding embolization of asymptomatic traumatic vertebral artery injuries that do not require cervical spine repair and fixation.
Case Description: A 78-year-old man fell backward from a height of about 1 m and was rushed to his previous hospital. He had a fracture of the left transverse process of the 6th cervical vertebra. Six hours after the trauma, he became unconscious; magnetic resonance angiography showed occlusion of the left vertebral and basilar arteries, and he was transferred to our hospital. The basilar artery was completely recanalized 430 min after the onset of unconsciousness. Due to the presence of thrombi in the distal vertebral artery at the level of the 6th cervical vertebra and collateral blood flow from the deep cervical artery, the distal vertebral artery was occluded to prevent embolism. Postoperative diffusion-weighted imaging showed extensive infarction in the posterior circulation, and the patient died two days after surgery.
Conclusion: In the case of vertebral artery injury, preparation for early occlusion of the basilar artery is necessary. If a thrombus and collateral blood flow are present distal to the vertebral artery injury, distal vertebral artery embolization may be necessary to prevent embolism.
Keywords: Basilar artery occlusion, Parent artery embolization, Thrombectomy, Vertebral artery injury
INTRODUCTION
Vertebral artery injuries associated with blunt cervical spine trauma are relatively common, ranging from 19% to 39%.[
There is a potential risk of fatal cerebral embolism due to recanalization of the vertebral artery after cervical spine realignment and fixation surgery in patients with traumatic vertebral artery occlusion.[
Here, we present a case of mechanical thrombectomy through the unaffected vertebral artery and simultaneous distal vertebral artery embolization for basilar artery occlusion that occurred during follow-up of vertebral artery injury caused by a blunt cervical spine fracture.
CASE REPORT
History and examination
A 78-year-old man fell backward from a height of about 1 m at his workplace, injuring the back of his head, neck, and back, and was rushed to the previous hospital. At the time of initial examination, he was conscious with no neurological abnormalities but had neck pain. He had diabetes, hypertension, hyperlipidemia, and a history of laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. Still, no significant family history and was not taking any antithrombotic agents. Cervical spine computed tomography (CT) showed vertebral body fractures at the 6th and 7th cervical vertebrae, a fracture of the left transverse process of the 6th cervical vertebra, and ossification of the posterior longitudinal ligament at the 4th–7th cervical spine levels [
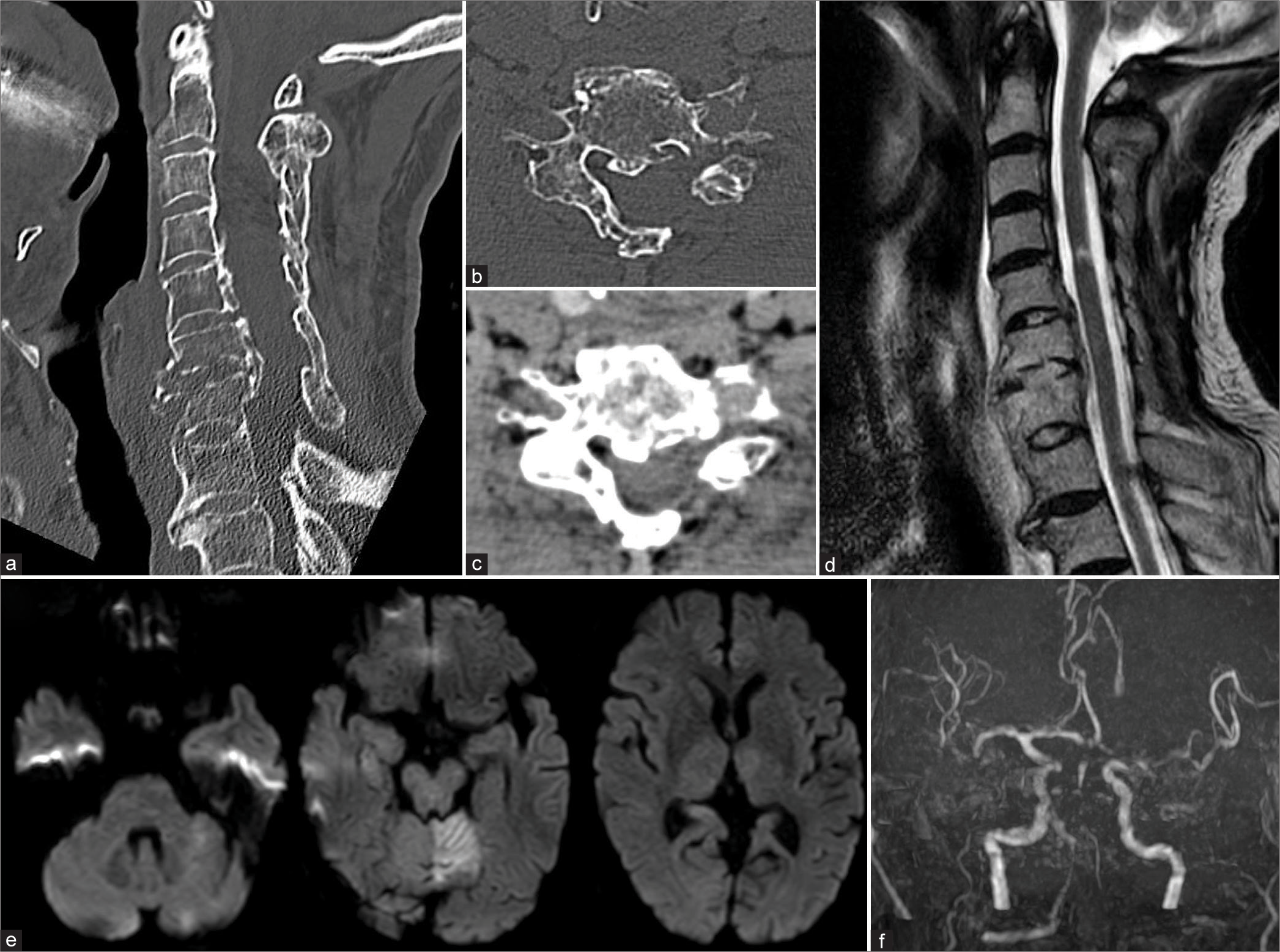
Figure 1:
Images taken at the previous hospital: (a) the sagittal section of cervical computed tomography (CT) shows vertebral fractures of the 6th and 7th cervical vertebrae and ossification of the posterior longitudinal ligament at the level of the 4th–7th cervical vertebrae. (b and c) The axial section of cervical CT at the level of the 6th cervical vertebra shows a fracture of the left transverse process and a slightly high-density area within the left transverse foramen. (d) Cervical spine T2-weighted magnetic resonance imaging shows no signs of compression of the spinal cord and a hyperintense area at the level of the 4th/5th cervical vertebrae. (e) Diffusion-weighted imaging at the time of loss of consciousness shows a slightly high-intensity area in the left cerebellum (posterior circulation acute stroke prognosis early CT score 9 points). (f) Magnetic resonance angiography at the time of loss of consciousness shows occlusion of the left vertebral and basilar arteries.
On arrival at our hospital, the Glasgow coma scale score was E1V1M4, and there was paralysis of the right upper and lower limbs. The National Institutes of Health Stroke Scale score was 32. At 310 min after the onset of altered consciousness, a head CT showed a hyperdense sign at the tip of the basilar artery and low-density areas in the left cerebellum and midbrain (pc-ASPECTS 7 points) [
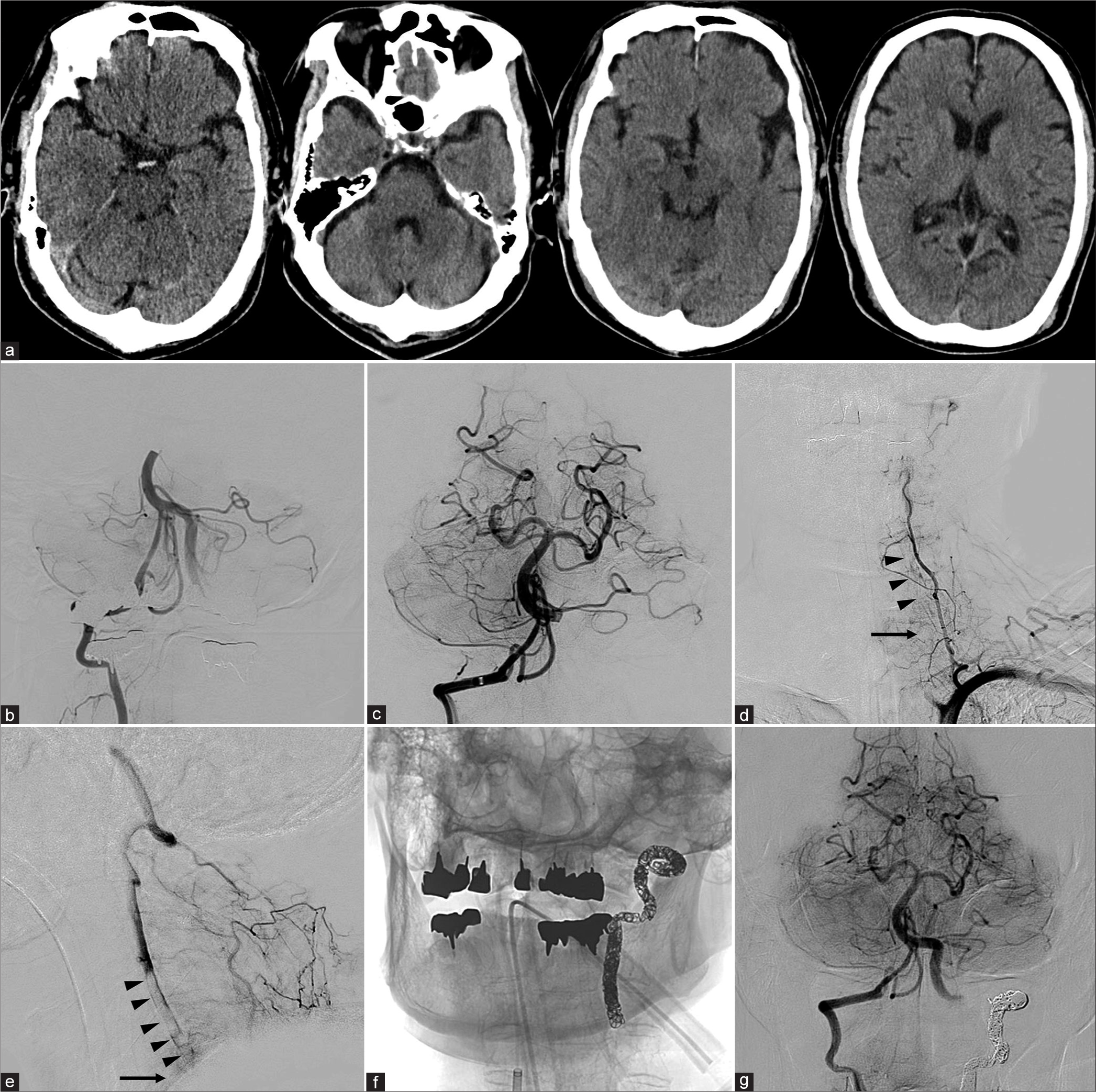
Figure 2:
Preoperative and intraoperative images at our hospital: (a) preoperative head computed tomography (CT) shows a hyperdense sign at the tip of the basilar artery and hypodense areas in the left cerebellum and midbrain (posterior circulation acute stroke prognosis early CT score 7 points). (b) Before thrombectomy, right vertebral artery angiography shows occlusion at the tip of the basilar artery. (c) After thrombectomy, right vertebral artery angiography shows complete recanalization of the tip of the basilar artery. (d and e) Left subclavian artery angiography shows occlusion at the origin of the left vertebral artery. Collateral blood flow from the left deep cervical artery to the left vertebral artery is observed, with anterograde flow beyond the level of the 6th cervical vertebra (arrow). Thrombi (arrowheads) are seen within the left vertebral artery at the level of the 4th–6th cervical vertebrae. (f) Coil embolization was performed in the distal part of the left vertebral artery from the level of the 3rd/4th cervical vertebra to the V3 segment. (g) After coil embolization, right vertebral artery angiography shows retrograde blood flow of the left posterior inferior cerebellar artery through the left vertebral artery.
Endovascular surgery
Under general anesthesia, a 6-Fr Fubuki dilator kit (Asahi Intecc, Seto, Japan) was inserted through the right femoral artery, and systemic heparinization was performed. To restore basilar artery blood flow as quickly as possible, the 6-Fr Fubuki dilator kit was guided into the open and unaffected right vertebral artery. Right vertebral artery angiography showed occlusion at the tip of the basilar artery [
The retrieved thrombus was macroscopically a red thrombus with a partial mixture of white thrombus [
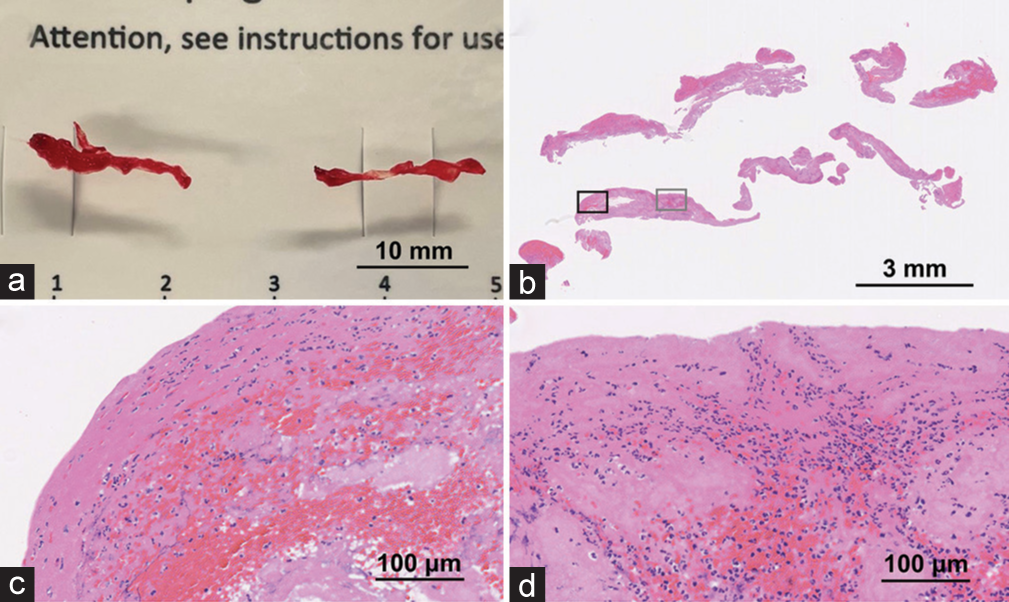
Figure 3:
Photograph and histopathological findings with hematoxylin-eosin staining of the retrieved thrombi: (a) the photograph shows a predominantly red thrombus with interspersed white thrombus. (b-d) b shows the entire thrombus under hematoxylin-eosin staining. c is a magnified view of the black rectangle in b, while d is a magnified view of the gray rectangle in b. The thrombus surface is dominated by platelets and fibrin, with neutrophils interspersed. Red blood cells are mixed in the thrombus.
Postoperative course
No improvement in neurological symptoms was observed after the surgery. Diffusion-weighted imaging performed 13 h after the onset of altered consciousness showed infarction in the midbrain, pons, both occipital lobes, both cerebellar hemispheres, and the left thalamus [
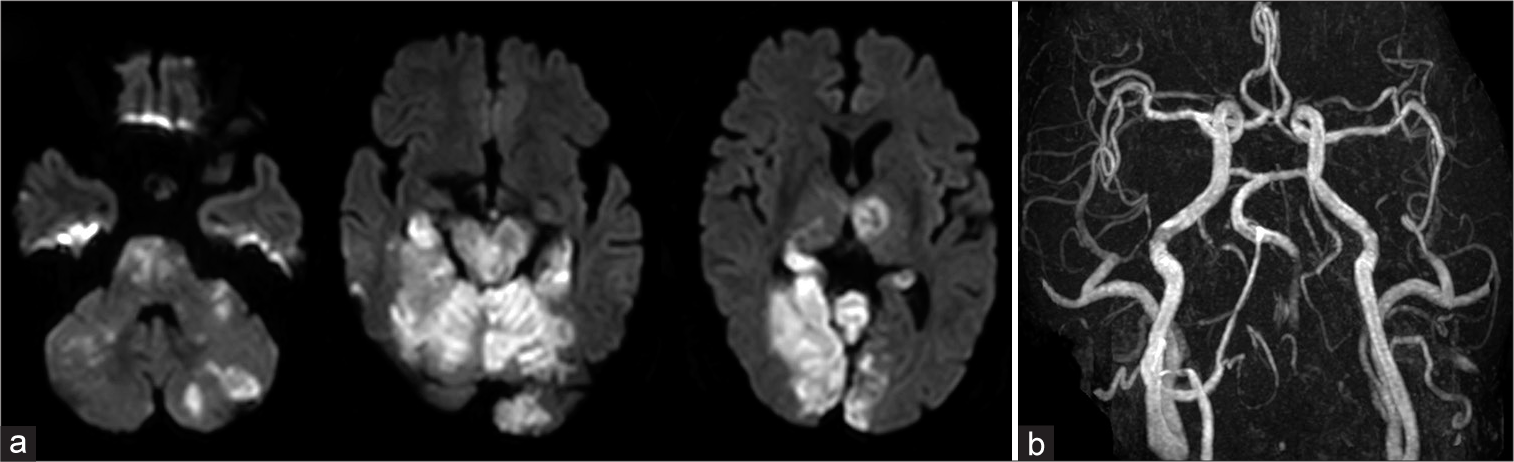
Figure 4:
Magnetic resonance imaging findings 13 h after the onset of altered consciousness disturbance: (a) diffusion-weighted imaging shows hyperintense areas in the midbrain, pons, bilateral cerebellum, bilateral occipital lobes, and left thalamus. (b) Magnetic resonance angiography shows patency of the right vertebral and basilar arteries and occlusion of the left vertebral artery.
DISCUSSION
In this case, vertebral artery injury was suspected due to a transverse foramen fracture of the 6th cervical vertebra following blunt force trauma. However, because cervical spine repair and fixation were not required, the vertebral artery was not evaluated at the initial visit. During follow-up, a basilar artery occlusion occurred relatively early (6 h after the trauma), and mechanical thrombectomy and embolization of the injured vertebral artery at the source of the embolism failed to save the patient’s life. To the best of our knowledge, this is the first report of a case in which thrombus retrieval from the unaffected vertebral artery and embolization of the distal vertebral artery were performed simultaneously for basilar artery occlusion caused by vertebral artery injury after blunt cervical spine trauma.
In this case, the transverse process fracture of the left 6th cervical vertebra and the high-density area in the foramen transversarium on cervical spine CT suggested that the left vertebral artery had been occluded at the level of the 6th cervical vertebra before the basilar artery occlusion occurred. Because left subclavian angiography did not show the left vertebral artery distal to the origin, the left vertebral artery was considered to be occluded at the level of the 6th cervical vertebra. There was a thrombus in the vertebral artery distal to the occluded area, and the left vertebral artery had antegrade blood flow distal to the level of the 6th cervical vertebra due to abundant collateral blood flow. Therefore, we speculated that the thrombus formation associated with the occlusion and the presence of collateral blood flow led to the basilar artery occlusion, although the vertebral artery was occluded at the site of the transverse process fracture.
To prevent embolism in traumatic vertebral artery occlusion, embolization of the proximal vertebral artery is usually the treatment of choice.[
In thrombectomy for basilar artery occlusion with vertebral artery lesions, there are reports of approaches from both the affected vertebral artery and the opposite unaffected vertebral artery.[
Among cervical spine injuries, dislocations with intervertebral joint injury, transverse foramen fractures, and fractures of the 1st–3rd cervical vertebrae have been reported to carry a high risk of vertebral artery injury.[
In recent years, randomized controlled trials have reported that thrombectomy for basilar artery occlusion yields better outcomes than medical treatment alone.[
CONCLUSION
In cases of vertebral artery injury, there is a possibility of early onset of basilar artery occlusion, necessitating preparation for early recanalization. Even in traumatic vertebral artery occlusion, there is a possibility of embolism due to a thrombus and collateral blood flow on the distal side of the occlusion. Thrombectomy from the unaffected side of the vertebral artery for basilar artery occlusion associated with vertebral artery injury may reduce the time to recanalization. It is believed that distal vertebral artery embolization is necessary to prevent embolism associated with traumatic vertebral artery occlusion in which a thrombus and collateral blood flow exist on the occluded distal side.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Becker KJ, Monsein LH, Ulatowski J, Mirski M, Williams M, Hanley DF. Intraarterial thrombolysis in vertebrobasilar occlusion. AJNR Am J Neuroradiol. 1996. 17: 255-62
2. Berne JD, Norwood SH. Blunt vertebral artery injuries in the era of computed tomographic angiographic screening: Incidence and outcomes from 8,292 patients. J Trauma. 2009. 67: 1333-8
3. Biffl WL, Moore EE, Elliott JP, Ray C, Offner PJ, Franciose RJ. The devastating potential of blunt vertebral arterial injuries. Ann Surg. 2000. 231: 672-81
4. Cohen JE, Leker RR, Gomori JM, Eichel R, Rajz G, Moscovici S. Emergent revascularization of acute tandem vertebrobasilar occlusions: Endovascular approaches and technical considerations-Confirming the role of vertebral artery ostium stenosis as a cause of vertebrobasilar stroke. J Clin Neurosci. 2016. 34: 70-6
5. Cothren CC, Moore EE, Biffl WL, Ciesla DJ, Ray CE, Johnson JL. Cervical spine fracture patterns predictive of blunt vertebral artery injury. J Trauma. 2003. 55: 811-3
6. Desouza RM, Crocker MJ, Haliasos N, Rennie A, Saxena A. Blunt traumatic vertebral artery injury: A clinical review. Eur Spine J. 2011. 20: 1405-16
7. Even J, McCullough K, Braly B, Hohl J, Song Y, Lee J. Clinical indications for arterial imaging in cervical trauma. Spine (Phila Pa 1976). 2012. 37: 286-91
8. Grandhi R, Weiner GM, Agarwal N, Panczykowski DM, Ares WJ, Rodriguez JS. Limitations of multidetector computed tomography angiography for the diagnosis of blunt cerebrovascular injury. J Neurosurg. 2018. 128: 1642-7
9. Indo M, Oya S, Shojima M, Inokuchi K, Yahata T, Sugiyama S. Prevention of thromboembolic infarction after surgery for traumatic cervical fracture with vertebral artery occlusion by preoperative endovascular coil embolization. World Neurosurg. 2019. 129: e838-44
10. Jovin TG, Li C, Wu L, Wu C, Chen J, Jiang C. Trial of thrombectomy 6 to 24 hours after stroke due to basilar-artery occlusion. N Engl J Med. 2022. 387: 1373-84
11. Lebl DR, Bono CM, Velmahos G, Metkar U, Nguyen J, Harris MB. Vertebral artery injury associated with blunt cervical spine trauma: A multivariate regression analysis. Spine (Phila Pa 1976). 2013. 38: 1352-61
12. Miller PR, Fabian TC, Croce MA, Cagiannos C, Williams JS, Vang M. Prospective screening for blunt cerebrovascular injuries: Analysis of diagnostic modalities and outcomes. Ann Surg. 2002. 236: 386-93
13. Morton RP, Hanak BW, Levitt MR, Fink KR, Peterson EC, Vilela MD. Blunt traumatic occlusion of the internal carotid and vertebral arteries. J Neurosurg. 2014. 120: 1446-50
14. Senda J, Nishikawa T, Iizuka H, Kato N, Ito H, Ohshima R. Thrombectomy using trevo provue stent retriever devices after recombinant tissue plasminogen activator thrombolysis for acute basilar artery occlusion during vertebral artery dissection. Intern Med. 2016. 55: 985-9
15. Shinohara T, Yamashita R, Koyama K, Fukuyama R, Kubota J, Mukaihara S. A case of mechanical thrombectomy for basilar artery occlusion across the vertebral artery dissection. No Kekkannai Chiryo. 2019. 4: 131-5
16. Tanaka T, Ogata A, Iwashita H, Liu X, Shojima H, Momozaki N. A case of mechanical thrombectomy for cerebral infarction due to vertebral artery dissection with cervical fracture. Neurotraumatology. 2020. 43: 28-32
17. Tao C, Nogueira RG, Zhu Y, Sun J, Han H, Yuan G. Trial of endovascular treatment of acute basilar-artery occlusion. N Engl J Med. 2022. 387: 1361-72
18. Tumialán LM, Theodore N. Basilar artery thrombosis after reduction of cervical spondyloptosis: A cautionary report. J Neurosurg Spine. 2012. 16: 492-6
19. Yonezawa A, Neki H, Mizuhashi S, Otsuka T, Tsukagoshi E, Yamane F. Case of a patient who developed basilar artery occlusion after treatment of traumatic vertebral artery dissection with proximal coil occlusion. J Neuroendovasc Ther. 2019. 13: 430-4