- Department of Neurosurgery, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, State University of New York, Buffalo, New York, USA
- Department of Neurosurgery, Roswell Park Cancer Institute, Buffalo, New York, USA
Correspondence Address:
Andrew J. Fabiano
Department of Neurosurgery, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, State University of New York, Buffalo, New York, USA
Department of Neurosurgery, Roswell Park Cancer Institute, Buffalo, New York, USA
DOI:10.4103/2152-7806.187531
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Fanous AA, Fabiano AJ. Bevacizumab for the treatment of post-stereotactic radiosurgery adverse radiation effect. Surg Neurol Int 02-Aug-2016;7:
How to cite this URL: Fanous AA, Fabiano AJ. Bevacizumab for the treatment of post-stereotactic radiosurgery adverse radiation effect. Surg Neurol Int 02-Aug-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/bevacizumab-treatment-post%e2%80%91stereotactic-radiosurgery-adverse-radiation-effect/
Abstract
Background:Adverse radiation effect (ARE) is one of the complications of stereotactic radiosurgery. Its treatment with conventional medications, such as corticosteroids, vitamin E, and pentoxifylline carries a high risk of failure, with up to 20% of lesions refractory to such medications. In addition, deep lesions and those occurring in patients with significant medical comorbidities may not be suitable for surgical resection. Bevacizumab is an antiangiogenic monoclonal antibody against vascular endothelial growth factor, a known mediator of cerebral edema. It can be used to successfully treat ARE.
Case Description:An 85-year-old man with a history of small-cell lung cancer presented with metastatic disease to the brain. He underwent stereotactic radiosurgery to a brain metastasis involving the right external capsule. Three months later, the lesion had increased in size, with significant surrounding edema. The patient developed an adverse reaction to steroid treatment and had a poor response to treatment with pentoxifylline and vitamin E. He was deemed a poor surgical candidate because of his medical comorbidities. He was eventually treated with 3 doses of bevacizumab, and the treatment resulted in significant clinical improvement. Magnetic resonance imaging showed some decrease in the size of the lesion and significant decrease in the surrounding edema.
Conclusions:Bevacizumab can be successfully used to treat ARE induced by stereotactic radiosurgery in patients with cerebral metastases. It is of particular benefit in patients considered unsuitable for surgical decompression. It is also beneficial in patients with poor tolerance to corticosteroids and in patients who do not respond to other medications.
Keywords: Adverse radiation effect, bevacizumab, cerebral metastases, complication, stereotactic radiosurgery
INRODUCTION
Adverse radiation effect (ARE) is one of the complications of stereotactic radiosurgery.[
Medical management of ARE includes corticosteroids, vitamin E, and pentoxifylline.[
Bevacizumab is an antiangiogenic monoclonal antibody against vascular endothelial growth factor, a known mediator of cerebral edema. Bevacizumab was shown to be effective in the treatment of radiation-induced necrosis in patients with brain tumors.[
CASE REPORT
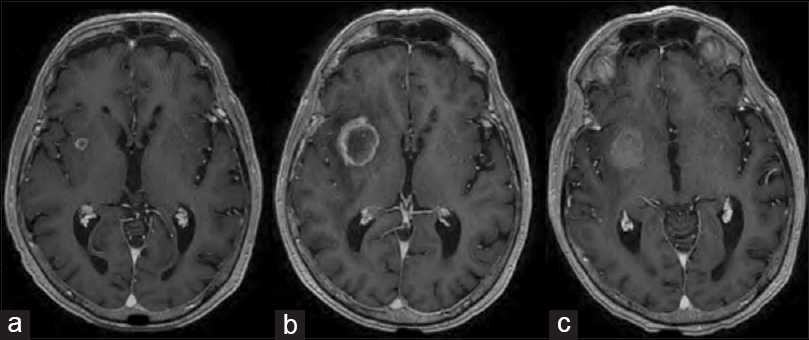
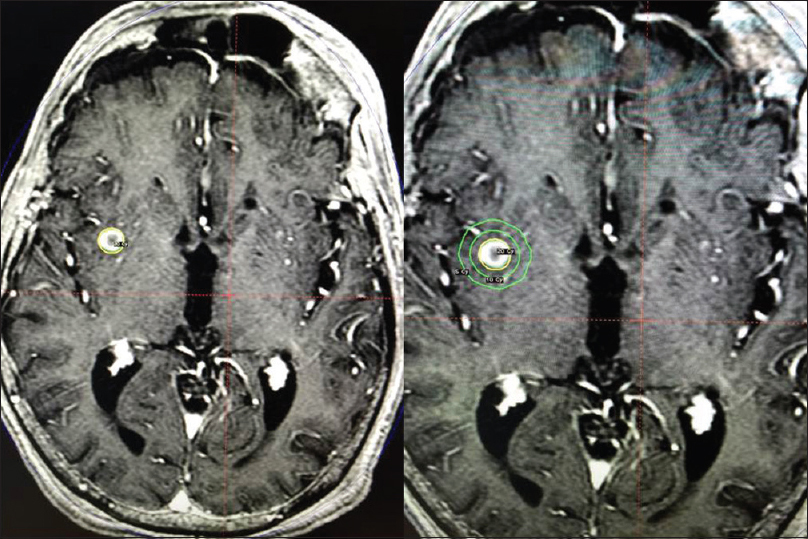
An 85-year old man with a history of small-cell lung cancer presented with metastatic disease to the brain. The patient underwent stereotactic radiosurgery (Gamma Knife Perfexion, Elekta Inc., Stockholm, Sweden) to a 7.0 × 8.0 × 8.0 mm brain metastasis involving the right external capsule [
Three months later, the patient developed new-onset imbalance. Magnetic resonance imaging (MRI) showed that the lesion had increased to 23.0 × 28.0 × 25.0 mm, with significant surrounding edema [
DISCUSSION
This case describes a significant size increase in a brain metastasis following stereotactic radiosurgery. There is no noninvasive diagnostic study to differentiate tumor recurrence from ARE in post-stereotactic radiosurgery brain metastases.[
Symptomatic post-stereotactic radiosurgery brain metastases should be treated.[
CONCLUSION
Bevacizumab can successfully be used to treat ARE induced by stereotactic radiosurgery in patients with cerebral metastases. It is of particular benefit in patients unsuitable for surgical decompression. Rather than a prolonged course of corticosteroids, patients with post-stereotactic radiosurgery ARE should be evaluated for bevacizumab therapy.
Authors’ contributions
Conception and design: both authors; Acquisition of data: both authors; Analysis and interpretation of data: both authors; Drafting of the manuscript: Fanous; Critical revision of the manuscript for important intellectual content: both authors; Final approval of the manuscript: both authors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank Paul H. Dressel BFA for preparation of the illustrations and Debra J. Zimmer for editorial assistance.
References
1. Clark AJ, Butowski NA, Chang SM, Prados MD, Clarke J, Polley MY. Impact of bevacizumab chemotherapy on craniotomy wound healing. J Neurosurg. 2011. 114: 1609-16
2. Dashti SR, Spalding A, Kadner RJ, Yao T, Kumar A, Sun DA. Targeted intraarterial anti-VEGF therapy for medically refractory radiation necrosis in the brain. J Neurosurg Pediatr. 2015. 15: 20-5
3. Fabiano AJ, Alberico RA. Laser-interstitial thermal therapy for refractory cerebral edema from post-radiosurgery metastasis. World Neurosurg. 2014. 81: 652 e1-4
4. Fabiano AJ, McBride P, Prasad D, Plunkett RJ, Fenstermaker RA, Qiu J. Post-stereotactic radiosurgery radiation necrosis: The three-month peak. Presented at the American Association of Neurological Surgeons 83rd Annual Meeting, Washington DC, May 2-6, 2015. p.
5. Fabiano AJ, Qiu J. Delayed failure of laser-induced interstitial thermotherapy for postradiosurgery brain metastases. World Neurosurg. 2014. 82: e559-63
6. Fabiano AJ, Qiu J. Post-stereotactic radiosurgery brain metastases: A review. J Neurosurg Sci. 2015. 59: 157-67
7. Kano H, Kondziolka D, Lobato-Polo J, Zorro O, Flickinger JC, Lunsford LD. T1/T2 matching to differentiate tumor growth from radiation effects after stereotactic radiosurgery. Neurosurgery. 2010. 66: 486-91
8. Levin VA, Bidaut L, Hou P, Kumar AJ, Wefel JS, Bekele BN. Randomized double-blind placebo-controlled trial of bevacizumab therapy for radiation necrosis of the central nervous system. Int J Radiat Oncol Biol Phys. 2011. 79: 1487-95
9. Rao MS, Hargreaves EL, Khan AJ, Haffty BG, Danish SF. Magnetic resonance-guided laser ablation improves local control for postradiosurgery recurrence and/or radiation necrosis. Neurosurgery. 2014. 74: 658-67
10. Taugourdeau-Raymond S, Rouby F, Default A, Jean-Pastor MJ. Bevacizumab-induced serious side-effects: A review of the French pharmacovigilance database. Eur J Clin Pharmacol. 2012. 68: 1103-7
11. Torcuator R, Zuniga R, Mohan YS, Rock J, Doyle T, Anderson J. Initial experience with bevacizumab treatment for biopsy confirmed cerebral radiation necrosis. J Neurooncol. 2009. 94: 63-8