- Department of Neurosurgery, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia,
- Department of Adult Neurosurgery, National National Neuroscience Institute, King Fahad Medical City, Riyadh, Saudi Arabia,
- Department of Neurosurgery, University of Miami, Miami, Florida, United States,
- Department of Radiation Oncology, Comprehensive Cancer Center, King Fahad Medical City, Riyadh, Saudi Arabia.
Correspondence Address:
Abdulrahman Y. Alturki
Department of Adult Neurosurgery, National National Neuroscience Institute, King Fahad Medical City, Riyadh, Saudi Arabia,
DOI:10.25259/SNI_760_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ali Alkhabiry1, Othman T. Almutairi2, Turki Elarjani3, Mohammed Bafaquh2, Hossam Alassaf4, Abdulrahman Y. Alturki2. Bibliometric analysis of the top-100 most cited articles on the radiosurgical management of cerebral arteriovenous malformation. 29-Dec-2020;11:477
How to cite this URL: Ali Alkhabiry1, Othman T. Almutairi2, Turki Elarjani3, Mohammed Bafaquh2, Hossam Alassaf4, Abdulrahman Y. Alturki2. Bibliometric analysis of the top-100 most cited articles on the radiosurgical management of cerebral arteriovenous malformation. 29-Dec-2020;11:477. Available from: https://surgicalneurologyint.com/surgicalint-articles/10491/
Abstract
Background: Radiosurgery is an effective, alternative treatment modality in managing patients with cerebral arteriovenous malformations (AVMs). The present study aims to highlight the scholarly impact of the top-100 most cited articles on the radiosurgical management of AVMs.
Methods: A title-specific search using the keyword “arteriovenous malformation” was conducted in the Scopus database. The outcome of the search was rearranged based on the citations count. Articles were categorized into four entities; clinical, gamma knife radiosurgery, linear accelerator (LINAC) radiosurgery, and proton beam radiosurgery. The exclusion criteria were applied to spinal or non-intracranial AVM, conference papers, non-English articles predominantly discussing the endovascular or microsurgical management.
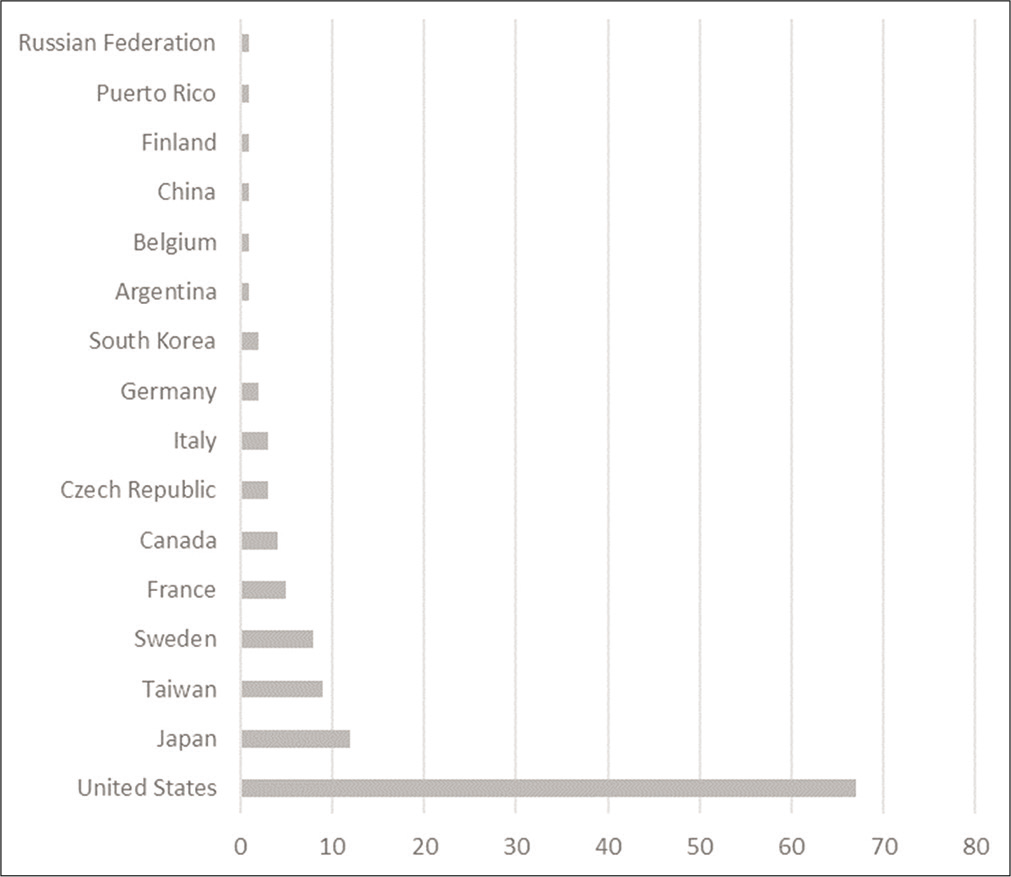
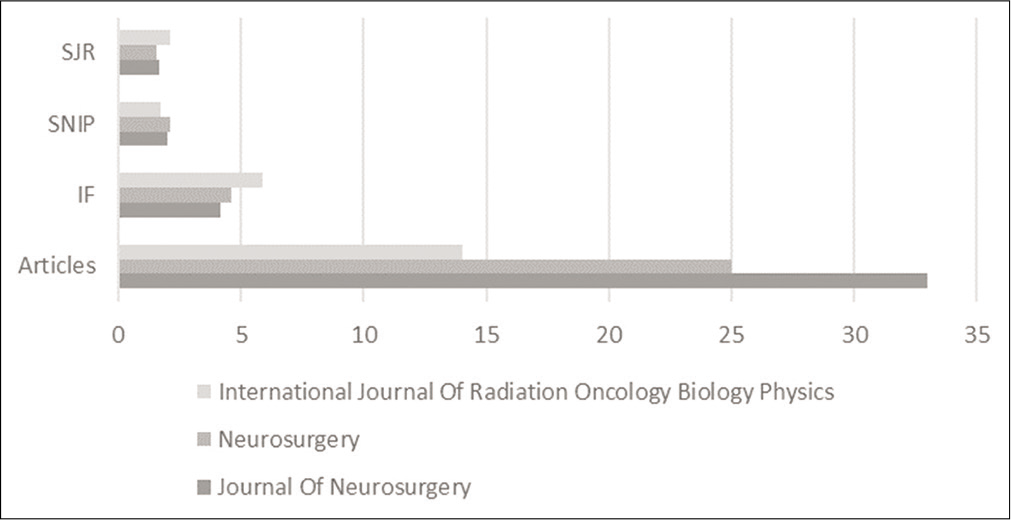
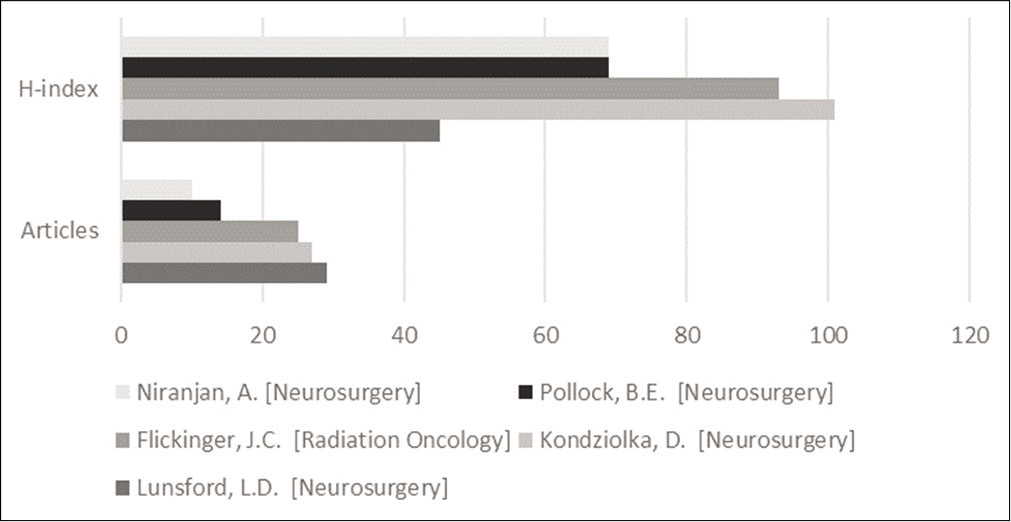
Results: The top-100 articles on the radiosurgical management of AVM were published between 1972 and 2016. Approximately one-third of the publications were produced between 1995 and 2000. The average citations per year for all papers were seven. The most-studied entity was pertinent to the clinical application of gamma knife radiosurgery in AVM (68%). The United States was the most active country in studying the radiosurgical application in AVM. The Journal of Neurosurgery published approximately one-third of the most-cited articles in the list. The top-3 most contributing authors, publishing 80% of articles in the list, were Lunsford et al.
Conclusion: The radiosurgical management of AVMs evolved significantly throughout the years. Identifications of the publication trends facilitate the acquisition of evidence-based articles for authors investigating various radiosurgical techniques in the treatment of AVMs.
Keywords: Arteriovenous malformation, Bibliometric, Citation analysis, Stereotactic radiosurgery
INTRODUCTION
Cerebral arteriovenous malformations (AVMs) are vascular lesions characterized by a pathological connection between the venous and arterial circulation through a nidus.[
The treatment option for accessible AVMs is usually achieved by complete surgical resection.[
Radiosurgery is defined as “The localized, focused, high-dose, irradiation commonly performed using Gamma knife (Leksell Gamma Knife® Perfexion, Elekta, Stockholm, Sweden), CyberKnife (Accuray Incorporated, 1310 Chesapeake Terrace, Sunnyvale, CA 94089, USA), or linear accelerator (LINAC).”[
Bibliometric analyses serve to address the top-cited articles in a discipline-specific scientific topic.[
Considering the growing field of radiosurgery and its application in the management of AVMs, it is paramount to perform a bibliometric analysis of the most-influential articles in the literature. The main aim of the study is to identify, analyze, and report the current knowledge of the top-100 most-cited articles on the radiosurgical management of cerebral AVMs.
MATERIALS AND METHODS
The identification of the most-cited articles on the radiosurgical management of AVM in the Scopus database was accessed in July 2020. The title-specific search using “arteriovenous malformation” as a search keyword was conducted. The outcome of the search was rearranged based on the article’s citations count in descending order. The acquisition of the top-100 articles discussing the radiosurgical management was selected after fulfilling our inclusion and exclusion criteria. Articles discussing the radiosurgical management of cerebral AVM as a primary outcome were included. Spinal or non-intracranial AVM, conference papers, and non-English articles predominantly discussing the endovascular or microsurgical management were excluded from the study.
The examined top-100 most cited articles were categorized into the following four entities: (1) clinical, (2) gamma knife radiosurgery, (3) linear accelerator (LINAC) radiosurgery, and (4) proton beam radiosurgery. In the performance of this bibliometric review, the following citometric relevant parameters were collected; article title, authors, 1st author’s specialty, contributing institutions, journals, country of origin, year of publication, citation count (CC), Citation per year (CY), Hirsch index (H-Index), Journal’s Source Normalized Impact Per Paper, Journal’s SCImago Journal Rank, and Journal Impact Factor.
The present study does not involve human subjects. Therefore, it is exempted from ethical approval, giving the nature of the study being non-interventional.
RESULTS
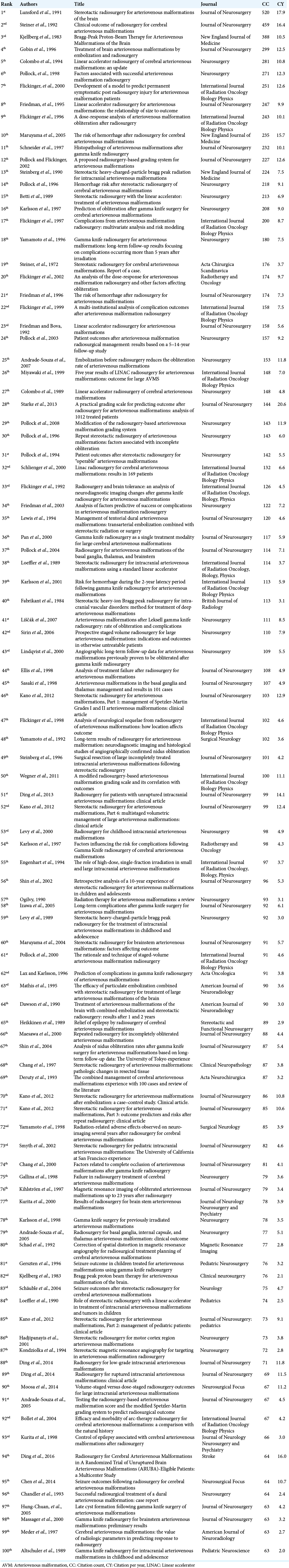
The keyword-based literature review resulted in identifying 9939 articles discussing AVM and, of which the top-100 articles according to the inclusion criteria were examined [
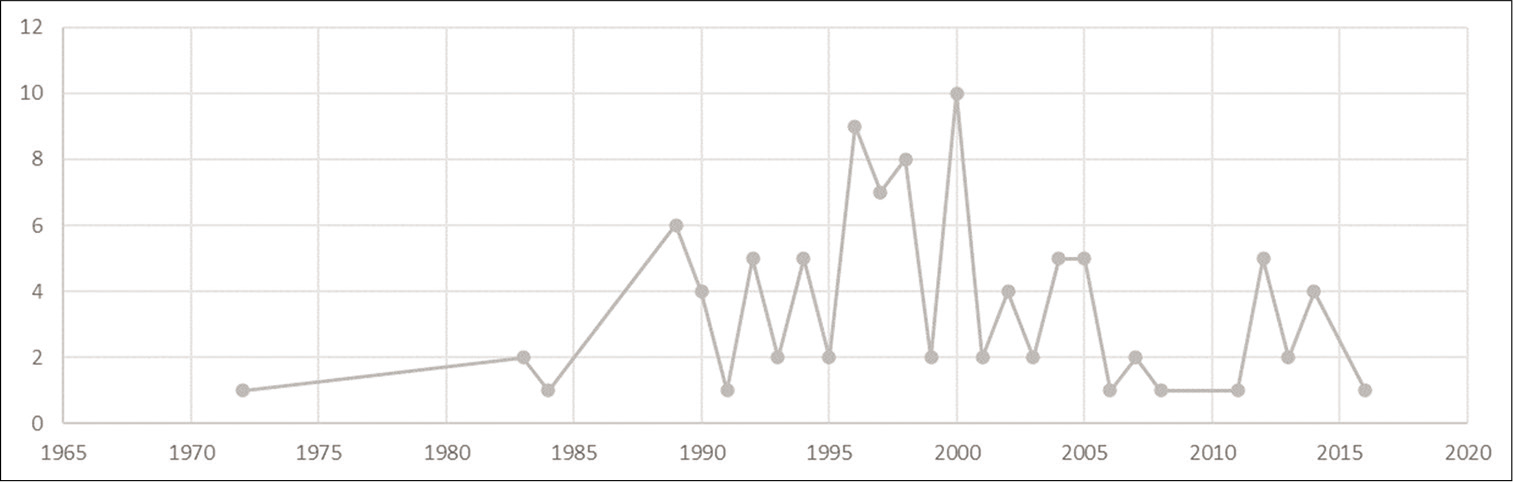
The top-100 articles on the radiosurgical management of AVM were published between 1972 and 2016 [
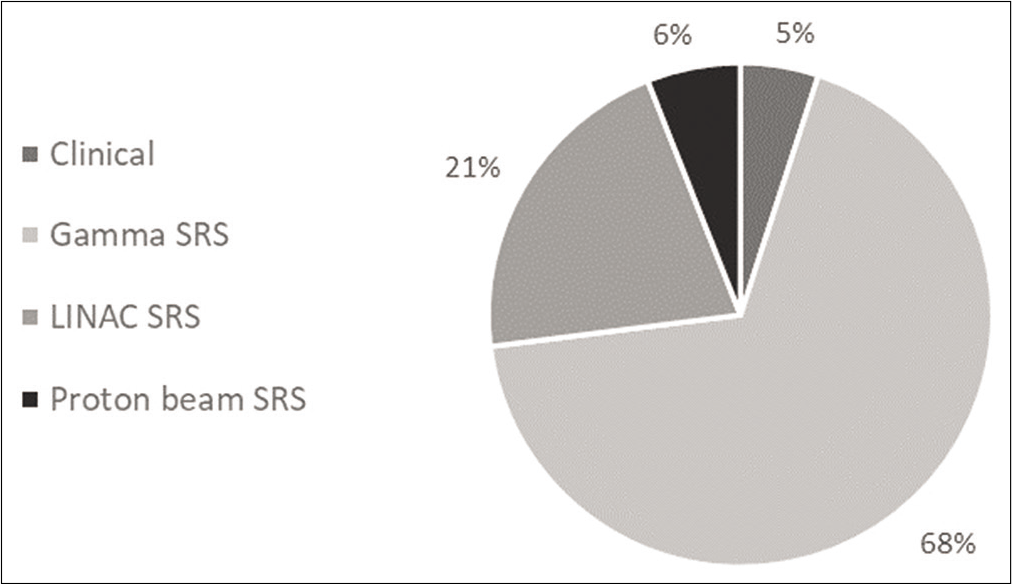
Approximately one-third of publications were produced between 1995 and 2000. The Top-100 articles have accumulated 11,456 citations and the rate of self-citation accounted for 12.12%. The average CY for all papers was seven. The most-studied entity was pertinent to the clinical application of Gamma knife radiosurgery in AVM (68%) [
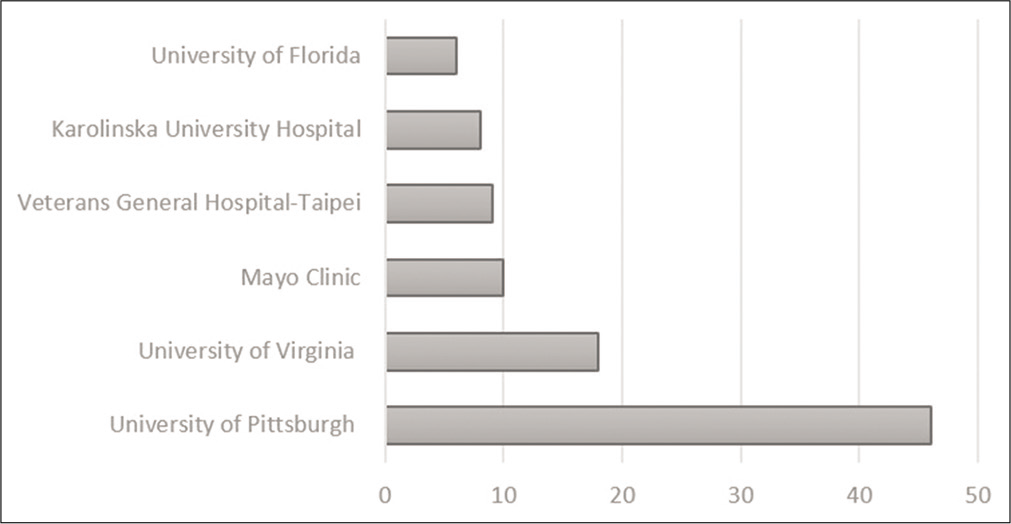
The University of Pittsburgh was the most prolific by producing 46 articles in the list [
The top-most cited article based on the citation count was authored by Lunsford et al., published in 1991 by JNS as “Stereotactic radiosurgery for AVMs of the brain,” to which it collected 520 citations over the years and was ranked the 2nd most-cited based on the citation per year.
The top most cited articles based on the citation per year was authored by Starke et al., published in 2013 by the JNS entitled “A practical grading scale for predicting outcome after radiosurgery for AVMs: analysis of 1012 treated patients” in which it had 20.6 CY and has accumulated 144 citation count over the year.
DISCUSSION
Articles addressing the radiosurgical management of AVMs evolved throughout the decades. Publications commenced by targeting the utilization of stereotactic radiosurgery using Gamma knife in the early 1970s. In the 1980s, as a result of the development and advancement of neuroimaging and proton/photon radiation technology, the publication trends shifted toward proton beam and linear accelerator (LINAC) radiosurgery. In addition, the earliest detailed reports on the utilization of proton beam radiosurgery for AVM with the longest follow-up period were published. In the top-100 list, most articles peaked in the publication in the 1990s, comprising 45% of all articles. Those articles were targeting all aspects of the radiosurgical management of AVM including the clinical outcome, Gamma knife, LINAC, and proton beam radiosurgery. In the 21st century, the majority of publications were highlighting the dose-response and clinical outcome predictions, comprising approximately half of the articles in the top-100 list.
The article ranking first in the top-100 list was published in 1991 by Lunsford et al. titled “Stereotactic radiosurgery for arteriovenous malformations of the brain” which received a total of 520 CC and 17.9 CY.[
A year later, the second highest cited article was published by Steiner et al. titled “Clinical outcome of radiosurgery for cerebral arteriovenous malformations” to which it received 459 CC and 16.4 CY.[
Gamma knife radiosurgery
Articles predominantly discussing the application of gamma knife radiosurgery peaked in terms of publication from 1972 to 2016. Operable and non-operable AVMs, deep-seated lesions, staging, and the risk of hemorrhage were the areas of interest to authors investigating the radiosurgical aspect of AVM. Gamma knife radiosurgery populated the majority of publications in the top 100 most cited articles on the radiosurgical management of AVM, comprising around two thirds of the articles. In the category of gamma knife radiosurgery, the first utilization of radiosurgery in obliterating AVM was discussed in the literature. Gobin et al. published an article (ranked 4th) titled “Treatment of brain AVMs by embolization and radiosurgery” to which it received 299 CC and 12.5 CY.[
LINAC radiosurgery
Articles in addressing LINAC radiosurgery had a publication peak between 1989 and 2007. Around one-fifth of the articles in the top-100 most cited publications on the radiosurgical management of AVM were investigating the usage of LINAC radiosurgery. In addition, the earliest reports on the usage of LINAC radiosurgery were published in the late 80s. Around 61% of articles addressing LINAC radiosurgery peaked in publication in the 90s. In the early years of the 21st century, articles have carried out what has been previously published in the literature, with a relatively larger number of cohorts. Colombo et al. published an article (ranked 5th) titled “Linear accelerator radiosurgery of cerebral AVMs: an update” to which it received 281 CC and 10.8 CY.[
Proton beam radiosurgery
In the “proton beam radiosurgery” entity, articles peaked in the publication from 1983 to 1990. During this period, the earliest, most detailed, and longest follow-up data on the application of proton beam radiosurgery were published. In addition, authors discussed the technicality of proton beam radiosurgery, treatment protocols, and the approach to the selection criteria of patients who were rendered fit to undergo such therapy. Kjellberg et al. published an article (ranked 3rd) titled “Bragg-Peak Proton-Beam Therapy for Arteriovenous Malformations of the Brain” to which it received 388 CC ad 10.5 CY.[
Clinical articles
Articles addressing the clinical entity of the radiosurgical management of AVM were published between 1990 and 2014. During the specified period, articles predominantly investigated predictors of successful obliteration of AVM utilizing radiosurgery. Furthermore, articles comprehensively investigated and compared dose-staged versus volume-staged radiosurgical treatment of AVM in terms of outcome and complications. Friedman et al. published an article (ranked 34th) titled “Analysis of factors predictive of success or complications in arteriovenous malformation radiosurgery” with 122 CC and 7.2 CY.[
The present bibliometric analysis on the radiosurgical management of AVM highlights the following clinical key aspects to practitioners in the field: (1) radiosurgery remains an important technique in managing patients with inoperable AVMs. (2) Complete obliteration of the lesion can be achieved by radiosurgery. (3) The obliteration rate of AVM following radiosurgery can be predicted by several factors including; age, location, volume, and the number of draining veins. (4) Prior embolization of the lesion facilitates the radiosurgical management of large-sized AVMs. (5) LINAC radiosurgery can successfully treat AVMs of relatively larger volumes (>10 cc). (6) Proton beam radiosurgery, in the form of heavy-charged particles, can be utilized to treat inaccessible AVMs. (7) Radiosurgery, before microsurgical resection, may be of use to treat large-sized and complex AVMs.
Limitations
In the current bibliometric analysis, few obstacles need to be acknowledged which may limit the generalizability of the findings. First, the rate of self-citations was encountered in more than one-tenth of the articles. Therefore, self-citations might falsely increase the CC for all published articles. However, this might be caused by the small society of radiosurgery and the limited number of institutions performing such advanced technology early in the history of radiation treatment (1970s). Second, a title-based search in a keyword-fashion might miss some articles published in the literature, and hence, not included in the analysis. Third, as the CC was considered to rank the articles in a descending order, older articles were likely to accumulate a higher number of citations throughout the years. However, the CY was calculated for all articles to balance this limitation. Fourth, only one database was utilized to conduct this bibliometric analysis. Fifth, due to the time; the relatively newer technology (i.e., CyberKnife) did not appear in our list. However, we expect an increasing number of publications relevant to this topic in the near future. Although bibliometric analyses assess the intellectual scholarly work from a quantitative perspective, the present study identified key and influential articles within this relatively growing field in the management of AVM.
CONCLUSION
The radiosurgical management of AVMs evolved significantly throughout the years. Articles addressing the application of Gamma knife radiosurgery were the most frequently published category by neurosurgeons in the field. The toptwo most cited articles in the list were both published in the JNS. Identifications of the publication trends serves as a benchmark for gaining evidence-based knowledge for authors investigating various radiosurgical techniques in AVMs.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alfaifi A, AlMutairi O, Allhaidan M, Alsaleh S, Ajlan A. The top 50 most-cited articles on acoustic neuroma. World Neurosurg. 2018. 111: e454-64
2. Almutairi O, Albakr A, Al-Habib A, Ajlan A. The top-100 most-cited articles on meningioma. World Neurosurg. 2017. 107: 1025-32.e5
3. Al-Shahi R, Warlow C. A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults. Brain. 2001. 124: 1900-26
4. Awad AJ, Walcott BP, Stapleton CJ, Ding D, Lee CC, Loeffler JS. Repeat radiosurgery for cerebral arteriovenous malformations. J Clin Neurosci. 2015. 22: 945-50
5. Brada M, Kitchen N. How effective is radiosurgery for arteriovenous malformations?. J Neurol Neurosurg Psychiatry. 2000. 68: 548-9
6. Cheng W, Kang Q, Xiao Q. Bibliometric analysis of the top 100 influential studies on carotid artery stenting. World Neurosurg. 2019. 122: e1321-31
7. Ding D, Starke RM, Kano H, Lee JYK, Mathieu D, Pierce J. Radiosurgery for unruptured brain arteriovenous malformations: An international multicenter retrospective cohort study. Neurosurgery. 2017. 80: 888-98
8. Ding D, Xu Z, Shih HH, Starke RM, Yen CP, Sheehan JP. Stereotactic radiosurgery for partially resected cerebral arteriovenous malformations. World Neurosurg. 2016. 85: 263-72
9. Friedman WA, Bova FJ, Bollampally S, Bradshaw P, Riina H, Gutin PH. Analysis of factors predictive of success or complications in arteriovenous malformation radiosurgery. Neurosurgery. 2003. 52: 296-308
10. Friedman WA, Bova FJ, Mendenhall WM. Linear accelerator radiosurgery for arteriovenous malformations: The relationship of size to outcome. J Neurosurg. 1995. 82: 180-9
11. Gobin YP, Laurent A, Merienne L, Schlienger M, Aymard A, Houdart E. Treatment of brain arteriovenous malformations by embolization and radiosurgery. J Neurosurg. 1996. 85: 19-28
12. Kiraz M, Demir E. A bibliometric analysis of publications on spinal cord injury during 1980-2018. World Neurosurg. 2020. 136: e504-13
13. Kjellberg RN, Hanamura T, Davis KR, Lyons SL, Adams RD. Bragg-peak proton-beam therapy for arteriovenous malformations of the brain. N Engl J Med. 1983. 309: 269-74
14. Lo EH. Linear accelerator radiosurgery of cerebral arteriovenous malformations: An update. Neurosurgery. 1994. 35: 342
15. Lunsford LD, Kondziolka D, Flickinger JC, Bissonette DJ, Jungreis CA, Maitz AH. Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg. 1991. 75: 512-24
16. Panagopoulos D, Karydakis P, Giakoumettis D, Themistocleous M. The 100 most cited papers about brain metastases. World Neurosurg. 2020. 138: 98-114
17. Pollock BE, Flickinger JC, Lunsford LD, Maitz A, Kondziolka D. Factors associated with successful arteriovenous malformation radiosurgery. Neurosurgery. 1998. 42: 1239-44
18. Sharma B, Lawrence DW. Top-cited articles in traumatic brain injury. Front Hum Neurosci. 2014. 8: 879
19. Steinberg GK, Chang SD, Levy RP, Marks MP, Frankel K, Marcellus M. Surgical resection of large incompletely treated intracranial arteriovenous malformations following stereotactic radiosurgery. J Neurosurg. 1996. 84: 920-8
20. Steinberg GK, Fabrikant JI, Marks MP, Levy RP, Frankel KA, Phillips MH. Stereotactic heavy-charged-particle bragg-peak radiation for intracranial arteriovenous malformations. N Engl J Med. 1990. 323: 96-101
21. Steiner L, Lindquist C, Adler JR, Torner JC, Alves W, Steiner M. Clinical outcome of radiosurgery for cerebral arteriovenous malformations. J Neurosurg. 1992. 77: 1-8