- Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq
- Department of Neurosurgery, College of Medicine, University of Baghdad, Baghdad, Iraq
- Department of Neurosurgery, College of Medicine, University of Warith Al-Anbiyaa, Karbala, Iraq,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, Ohio, United States.
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Cincinnati, Cincinnati, Ohio, United States.
DOI:10.25259/SNI_973_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammed A. Alrawi1, Muthanna N. Abdulqader1, Hayder R. Salih1, Saleh Abdulkareem Saleh2, Mohammedbaqer Ali Al-Ghuraibawi3, Mustafa M. Altaweel1, Mustafa Ismail1, Samer S. Hoz4. Bilateral basal ganglia hemorrhage in a 2-year-old child. 01-Dec-2023;14:415
How to cite this URL: Mohammed A. Alrawi1, Muthanna N. Abdulqader1, Hayder R. Salih1, Saleh Abdulkareem Saleh2, Mohammedbaqer Ali Al-Ghuraibawi3, Mustafa M. Altaweel1, Mustafa Ismail1, Samer S. Hoz4. Bilateral basal ganglia hemorrhage in a 2-year-old child. 01-Dec-2023;14:415. Available from: https://surgicalneurologyint.com/surgicalint-articles/12650/
Abstract
Background: Basal ganglia hemorrhage (BGH) is an intracerebral subtype of hemorrhage located in the caudate nucleus, putamen, globus pallidus, or adjacent structures such as the thalamus or internal capsule. Bilateral involvement of both basal ganglia is exceedingly infrequent. Herein, we report a case of a 2-year-old female who was discovered to have spontaneous bilateral BGH with a unique hemorrhagic extension.
Case Description: A 2-year-old female child who presented with a decreased level of consciousness, seizure, and fever was discovered to have bilateral BGH during imaging evaluation that extended from the head of the caudate to involve the putamen, globus pallidus, and anterior limb of the internal capsule.
Conclusion: Bilateral BGH is extremely rare, and to the best of our knowledge, this is the first case report in pediatric age groups.
Keywords: Bilateral basal ganglia hemorrhage, Intracerebral hemorrhage, Pediatric, Spontaneous
INTRODUCTION
Intracerebral hemorrhage (ICH) represents the second most common cause of stroke and is characterized by bleeding in the brain parenchyma with or without intraventricular extension. ICH comprises 10–15% of all strokes and has substantial mortality and morbidity associated with long-term disability.[
Basal ganglia hemorrhage (BGH) constitutes 34.2% of all ICH subtypes and is located in the caudate nucleus, putamen, and globus pallidus. However, adjacent structures such as the thalamus or internal capsule can also be involved. Secondary to cerebral lobes, ICH, putamen, and thalamus are the most common sites, with 32.7% and 15%, respectively.[
Bilateral BGH is an outstandingly infrequent context, with only limited reports having been documented to date. The etiology can be either traumatic or spontaneous. However, spontaneous bilateral BGH has not been reported in the pediatric age group. Herein, we report a case of a 2-year-old female who was discovered to have spontaneous bilateral BGH with a unique hemorrhagic extension.
CASE PRESENTATION
A 2-year-old female child who had no obvious history of chronic disease or perinatal complications presented to the emergency department of the general hospital after developing a fever, generalized tonic-clonic seizures, and ataxia. The physical examination was unremarkable except for ataxic gait. After the family refused to consent to the lumbar puncture, the child was treated conservatively and discharged well according to the family will after symptomatic improvement with no complications.
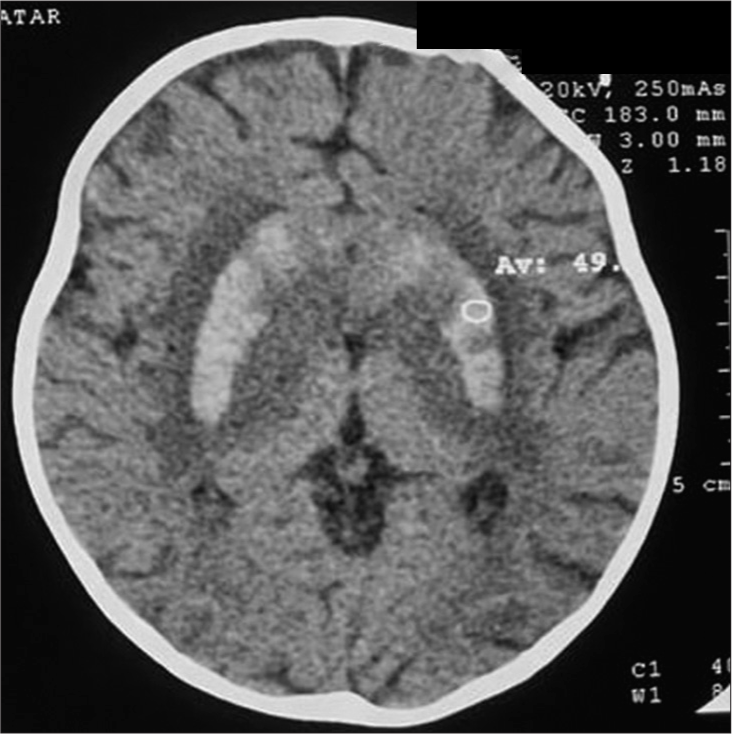
A few days later, the child returned to the hospital due to a recurrence of the symptoms, including fever, status epilepticus, and decreased level of consciousness that required re-admission. Although the fever and seizure attacks were controlled, the conscious level remained the same without improvement. Furthermore, the child deteriorates and develops spasticity in both upper and lower limbs. A neurosurgical consultation was requested, and after obtaining a non-contrast brain computed tomography (CT) scan, it revealed bilateral hyperdense areas symmetrically involving both caudate and lentiform nuclei with bilateral perifocal edema without midline shift or bony lesions [
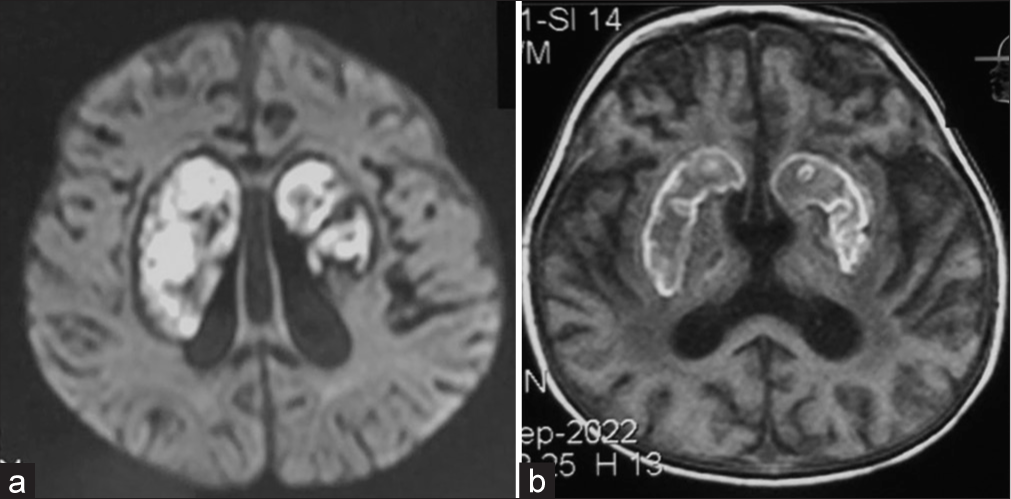
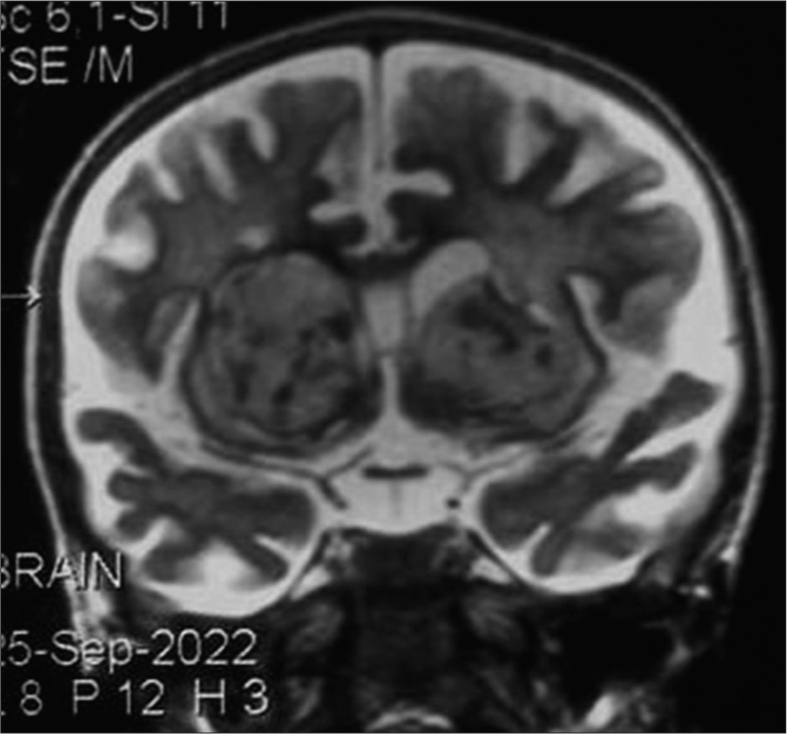
A 1-month follow-up brain magnetic resonance imaging (MRI) demonstrated a hemorrhage that involves both basal ganglia with 4.5 cm × 1.8 cm on the right side and 3.2 cm × 2 cm on the left side, which applies the mass effect on the frontal horn of both lateral ventricles [
Figure 2:
(a) Axial view of brain magnetic resonance imaging (MRI) demonstrates bilateral basal ganglia hemorrhage (BGH) with 4.5 cm × 1.8 cm on the right side and 3.2 cm × 2 cm on the left side, the hemorrhage extended from the head of the caudate nucleus bilaterally to involve globus pallidus, putamen, and anterior limb of the internal capsule; moreover, the hematoma compresses the anterior horn of both lateral ventricles. (b) Axial view of brain MRI demonstrates bilateral BGH, which extended from the head of the caudate nucleus bilaterally to involve globus pallidus, putamen, and anterior limb of the internal capsule; furthermore, the hematoma compresses the anterior horn of both lateral ventricles.
DISCUSSION
BGH is a subtype of ICH and mainly occurs in the putamen or the nearby structure, such as the thalamus and internal capsule. Furthermore, BGH is classified into two main types: Traumatic and spontaneous. Although the incidence of spontaneous unilateral BGH is about 24.6/100,000 person-year, spontaneous bilateral BGH is exceedingly rare, with only 40 reported cases.[
The adult population represents nearly all the documented cases of the bilateral involvement of spontaneous BGH. On the other hand, one case of a 13-year-old female with unusual dengue viral hemorrhagic encephalitis has been reported by Nadarajah et al.[
There is no consensus regarding the pathophysiological events that lead to the development of spontaneous bilateral BGH; however, the findings of the Alhashim et al. review attribute the causes of spontaneous bilateral BGH to uncontrolled hypertension (50%), intoxication, and metabolic (18.33%), vascular anomalies (16.66%), and infectious agents (10%).[
The presentation of spontaneous ICH in children mostly included headaches, vomiting, impaired consciousness, convulsions, and focal neurological deficits,[
The most reported site that is involved in bilateral BGH is the bilateral putamen (71.70%), followed by bilateral pallidum (15.09%).[
Because spontaneous bilateral BGH is an extremely rare condition, we could not find similar pediatric cases in the literature to compare with and could not obtain any information about the hospital course and treatment. However, in this case, the reported child had a progressive course that was highlighted by seizure attacks, fever, and all limb spasticity until, finally, the child developed a lack of awareness.
Almost all patients with bilateral BGH have a poorer outcome than solitary ICH, mainly due to the destruction of crossing and non-crossing fibers, bilateral diaschisis phenomenon, severely disturbed consciousness, quadriparesis, and pseudobulbar palsy.[
The complications encountered with bilateral BGH were aspiration pneumonia, quadriparesis, hemiparesis, recurrent stroke, and death.[
In summary, to the best of the authors’ knowledge, this is the first case report of spontaneous bilateral BGH in the pediatric group. The patient was a 2-year-old female child who presented with fever, decreased level of consciousness, and seizures. The radiological imaging of the brain revealed a bilateral hemorrhage that involved the head of the caudate nucleus, putamen, globus pallidus, and anterior limb of the internal capsule.
CONCLUSION
Spontaneous bilateral BGH is an extremely rare finding, and this is the first case report in the pediatric age group. The brain radiological imaging of the reported 2-year-old child confirms bilateral ICH that extends from the head of the caudate nucleus to involve the putamen, globus pallidus, and anterior limb of the internal capsule.
Ethical approval
Not applicable.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alhashim A, Hadhiah K, Al-Dandan H, Aljaman M, Alabdali M, Alshurem M. Spontaneous simultaneous bilateral basal ganglia hemorrhage (SSBBGH): Systematic review and data analysis on epidemiology, clinical feature, location of bleeding, etiology, therapeutic intervention and outcome. Vasc Health Risk Manag. 2022. 18: 267-76
2. Bahrami M, Keyhanifard M, Afzali M. Spontaneous intracerebral hemorrhage, initial computed tomography (CT) scan findings, clinical manifestations and possible risk factors. Am J Nucl Med Mol Imaging. 2022. 12: 106-12
3. Boulouis G, Blauwblomme T, Hak JF, Benichi S, Kirton A, Meyer P. Nontraumatic pediatric intracerebral hemorrhage. Stroke. 2019. 50: 3654-61
4. Hassan MS, Mohamed Ali A, Farah Osman M, Ahmed A. Spontaneous bilateral basal ganglia hemorrhage due to severe hypertension. Vasc Health Risk Manag. 2022. 18: 473-7
5. Hu YZ, Wang JW, Luo BY. Epidemiological and clinical characteristics of 266 cases of intracerebral hemorrhage in Hangzhou, China. J Zhejiang Univ Sci B. 2013. 14: 496-504
6. Nadarajah J, Madhusudhan KS, Yadav AK, Gupta AK, Vikram NK. Acute hemorrhagic encephalitis: An unusual presentation of dengue viral infection. Indian J Radiol Imaging. 2015. 25: 52-5
7. Piastra M, De Luca D, Genovese O, Tosi F, Caliandro F, Zorzi G. Clinical outcomes and prognostic factors for spontaneous intracerebral hemorrhage in pediatric ICU: A 12-year experience. J Intensive Care Med. 2019. 34: 1003-9
8. Seo JS, Nam TK, Kwon JT, Park YS. Multiple spontaneous simultaneous intracerebral hemorrhages. J Cerebrovasc Endovasc Neurosurg. 2014. 16: 104-11
9. Shaheed TA, Glover N, Alboiny S. Nontraumatic spontaneous bilateral basal ganglia hemorrhage: A rare case report. Cureus. 2020. 12: e11299
10. Yang Z, Chen J, Mu J. Simultaneous bilateral basal ganglia hemorrhage. Curr Drug Deliv. 2017. 14: 807-15
11. Yen CP, Lin CL, Kwan AL, Lieu AS, Hwang SL, Lin CN. Simultaneous multiple hypertensive intracerebral haemorrhages. Acta Neurochir (Wien). 2005. 147: 393-9
12. Zhao J, Chen Z, Wang Z, Yu Q, Yang W. Simultaneous bilateral hypertensive basal ganglia hemorrhage. Neurol Neurochir Pol. 2016. 50: 275-9
13. Ziai WC, Carhuapoma JR. Intracerebral hemorrhage. Continuum (Minneap Min). 2018. 24: 1603-22