- Department of Neurosurgery, University of Texas Southwestern, Dallas, Texas, United States.
- Department of Anesthesia and Pain Management, University of Texas Southwestern, Dallas, Texas, United States.
Correspondence Address:
Salah G. Aoun, University of Texas Southwestern, Dallas, Texas, United States.
DOI:10.25259/SNI_901_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: James P. Caruso1, Mark N. Pernik1, Zachary D. Johnson1, Tarek Y. El Ahmadieh1, Babatunde Ogunnaike2, Owoicho Adogwa1, Salah G. Aoun1, Carlos A. Bagley1. Blood preservation techniques in complex spine surgery: Illustrative case and review of therapeutic options. 11-Oct-2021;12:515
How to cite this URL: James P. Caruso1, Mark N. Pernik1, Zachary D. Johnson1, Tarek Y. El Ahmadieh1, Babatunde Ogunnaike2, Owoicho Adogwa1, Salah G. Aoun1, Carlos A. Bagley1. Blood preservation techniques in complex spine surgery: Illustrative case and review of therapeutic options. 11-Oct-2021;12:515. Available from: https://surgicalneurologyint.com/surgicalint-articles/11168/
Abstract
Background: Complex spine surgery predisposes patients to substantial levels of blood loss, which can increase the risk of surgical morbidity and mortality.
Case Description: A 29-year-old achondroplastic male required thoracolumbar deformity correction. However, he refused potential allogeneic blood transfusions for religious reasons. He, therefore, underwent pre-operative autologous blood donation and consented to the use of the intraoperative cell salvage device. Immediately prior to the incision, he underwent acute normovolemic hemodilution. Throughout the case, we additionally utilized meticulous hemostasis. Postoperatively, he was supplemented with iron and erythropoietin and recovered well. When he required a revision procedure 3 months later, similar strategies were successfully employed.
Conclusion: Numerous strategies exist pre-operatively, intraoperatively, and post-operatively to optimize blood loss management for patients who refuse blood transfusions but warrant major spinal deformity surgery.
Keywords: Achondroplasia, Blood loss, Deformity, Spinal fusion, Transfusion
INTRODUCTION
Reconstructive spine surgery often results in significant blood loss.[
CASE REPORT
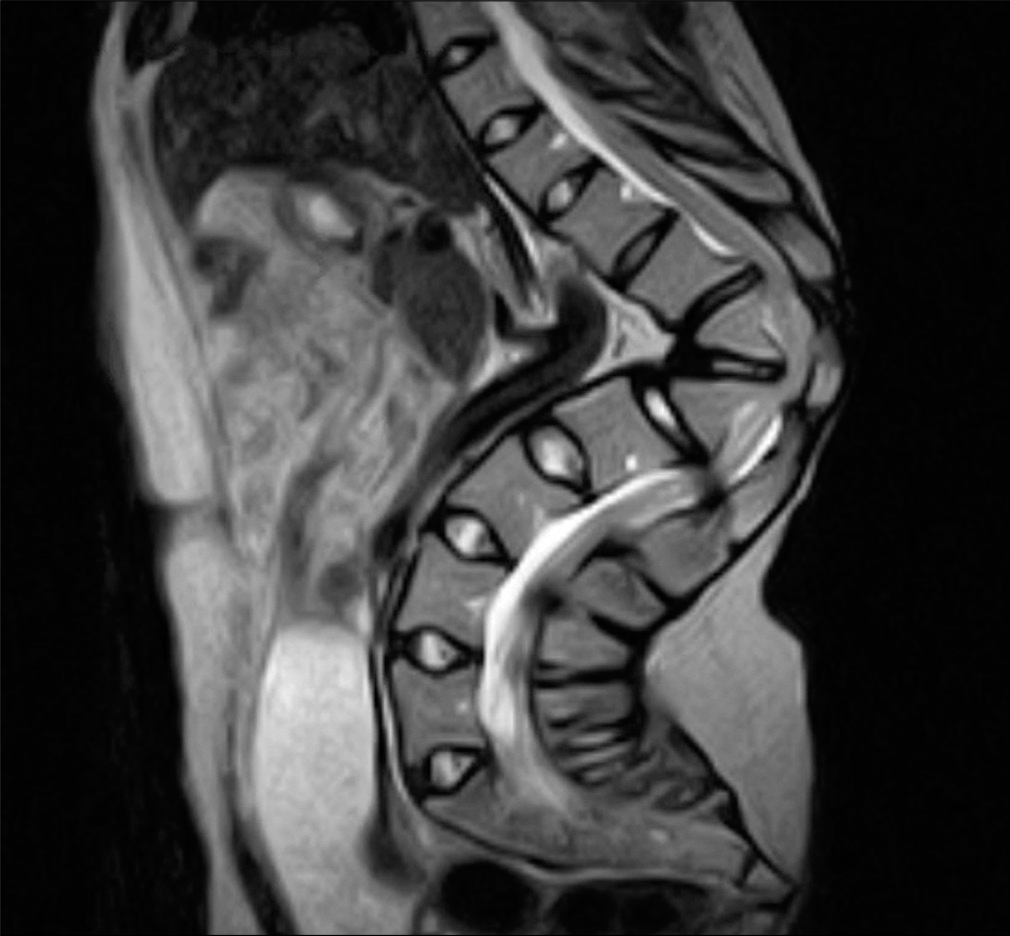
A gentleman with achondroplasia presented to our clinic with worsening mechanical back pain and myelopathy attributed to a progressive T12/L1 kyphosis. Magnetic resonance/Computed tomography (MR/CT) imaging documented a severe thoracolumbar kyphotic deformity with the apex at T12-L1. Additionally, the Cobb angle was nearly 90 degrees, with associated draping of the neural elements over the spinal column [
Blood product/adjuvant therapy management
For religious reasons, the patient refused heterologous blood transfusions for this surgery. His pre-operative hemoglobin was 14.3 g/dL, and 2 units of autologous blood were harvested from the patient immediately before surgery. He underwent preoperative acute normovolemic hemodilution (PANH) and consented to using an intraoperative cell salvage device. Transpedicular vertebral column resections were performed at the T12 and L1 levels, resulting in circumferential decompression of the thecal sac, and an expandable cage filled with autograft bone was placed between the inferior endplate of T11 and the superior endplate of L2.
Intraoperative blood loss and resuscitative measures
Estimated blood loss during the surgery was approximately 1 l. Intra-operatively, he received the two units of his autologous blood, 600 cc of his own blood products from the cell salvage device, and approximately 2 l of crystalloid/colloid fluid resuscitation. The immediate postoperative hemoglobin was 6.5 g/dL, and he received iron and EPO supplements. He remained neurologically and hemodynamically stable.
Postoperative course
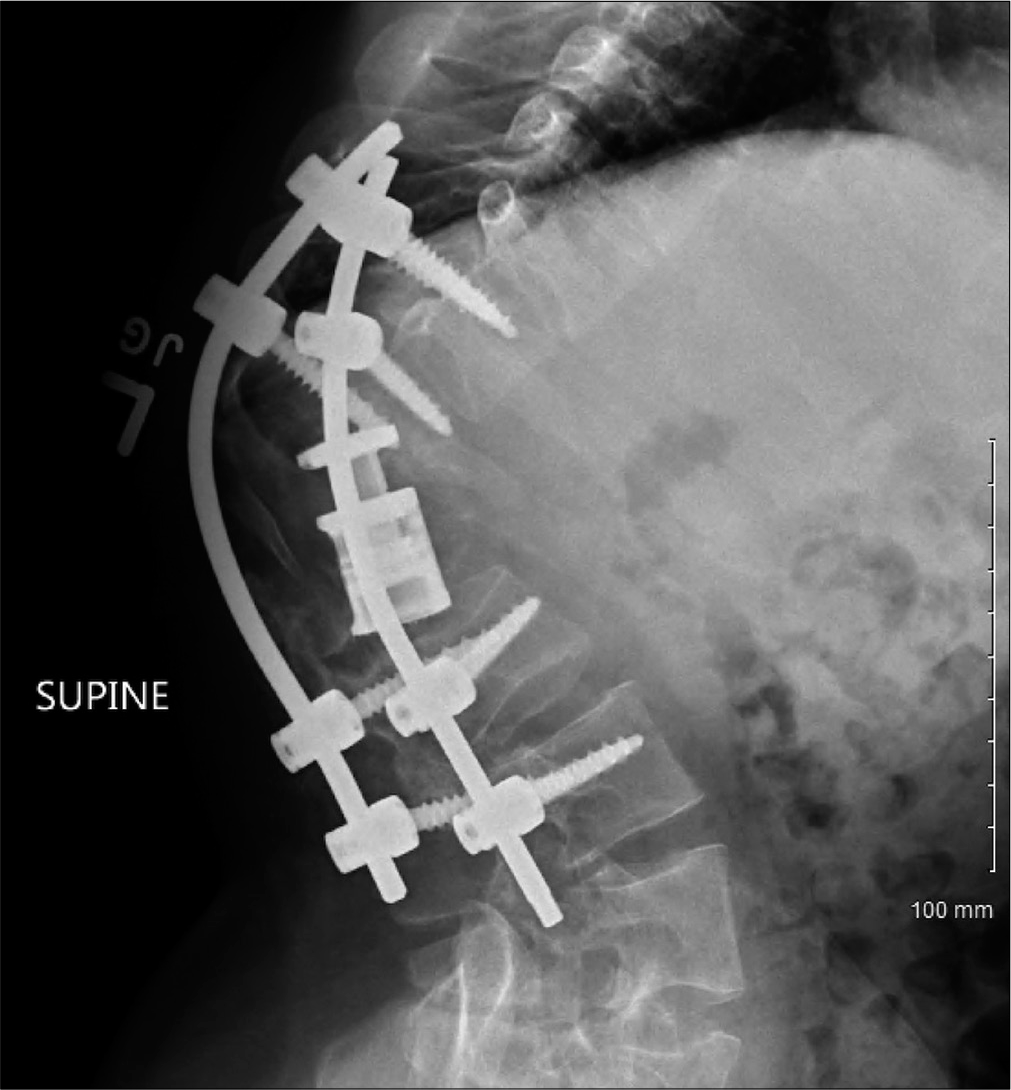
Post-operatively, the patient’s neurological exam remained unchanged. Imaging demonstrated expected post-surgical changes, adequate instrumentation placement, and improvement of the kyphotic deformity at T12/L1. 1 month later, the patient represented to with progressive paraparesis and urinary retention. Standing thoracolumbar X-rays revealed a worsening kyphotic deformity [
Second surgery and hematological management
For 3 days prior to the second spine operation consisting of extension of the fusion to the T9 level, the patient underwent EPO supplementation, PANH, with intraoperative utilization of the cell salvage device. Blood loss was approximately 500 cc. Post-operatively, he restarted EPO and iron supplementation and was ultimately discharged home. His hemoglobin on postoperative day 30 recovered to 11.8, and his EPO was discontinued. 1-year later, his mechanical back pain had improved as had his paraparesis.
DISCUSSION
Perioperative and intraoperative techniques
For patients who decline autologous blood transfusions for major spinal deformity surgery, the use of immediate preoperative blood donation (PABD) and PANH techniques to support perioperative hemoglobin levels are well known. Our patient underwent PABD and PANH, which minimized his need for postoperative allogeneic transfusions.[
Postoperative techniques
Our patient was supplemented perioperatively with recombinant EPO to stimulate endogenous hemoglobin production and facilitate the function of erythroid precursor cells.[
CONCLUSION AND AUTHORS’ PREFERRED TREATMENT RECOMMENDATIONS
Blood loss management remains a crucial topic of study in complex spine surgery. Here, thoracolumbar spine deformity correction in a 29-year-old achondroplastic warranted preoperative and postoperative iron and EPO supplementation, immediate preoperative autologous blood donation with PANH, and intraoperative cell-salvage techniques.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
None.
References
1. Barile L, Fominskiy E, di Tomasso N, Castro LE, Landoni G, de Luca M. Acute normovolemic hemodilution reduces allogeneic red blood cell transfusion in cardiac surgery: A systematic review and meta-analysis of randomized trials. Anesth Analg. 2017. 124: 743-52
2. Bess RS, Lenke LG. Blood loss minimization and blood salvage techniques for complex spinal surgery. Neurosurg Clin N Am. 2006. 17: 227-34
3. Carson JL, Stanworth SJ, Roubinian N, Fergusson DA, Triulzi D, Doree C. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2016. 10: CD002042
4. Fisahn C, Jeyamohan S, Norvell DC, Tubbs RS, Moisi M, Chapman JR. Association between allogeneic blood transfusion and postoperative infection in major spine surgery. Clin Spine Surg. 2017. 30: E988-92
5. Gum JL, Carreon LY, Kelly MP, Hostin R, Robinson C, Burton DC. Cell saver for adult spinal deformity surgery reduces cost. Spine Deform. 2017. 5: 272-6
6. Janssen SJ, Braun Y, Wood KB, Cha TD, Schwab JH. Allogeneic blood transfusions and postoperative infections after lumbar spine surgery. Spine J. 2015. 15: 901-9
7. Oppitz PP, Stefani MA. Acute normovolemic hemodilution is safe in neurosurgery. World Neurosurg. 2013. 79: 719-24
8. Shapiro F, Sethna N. Blood loss in pediatric spine surgery. Eur Spine J. 2004. 13: S6-17
9. Vargas-Pabon M, Diaz-Trapiella A, Hurtado MJ, Varela ND, Sabio JL. Erythropoietin as adjuvant to pre-operative autologous blood donation in total hip arthroplasty: New algorithm for use. Transfus Apher Sci. 2005. 33: 91-7