- Department of Neurosurgery, Yokohama Sakae Kyosai Hospital, Yokohama,
- Department of Neurology, Yokohama Sakae Kyosai Hospital, Yokohama,
- Department of Neurosurgery, Shima Neurosurgical Orthopedic Clinic, Kawasaki, Kanagawa, Japan.
Correspondence Address:
Kazuya Morita, Department of Neurosurgery, Yokohama Sakae Kyosai Hospital, Yokohama, Japan.
DOI:10.25259/SNI_172_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kazuya Morita1, Akira Tamase1, Hiroyuki Abe1, Kentaro Mori1, Issei Fukui1, Ryotaro Yamashita2, Mutsuki Takeda2, Tatsu Nakano2, Hiroshi Shima3, Motohiro Nomura1. Bow hunter’s syndrome treated by anterior decompression with fusion: A case report. 31-Mar-2022;13:115
How to cite this URL: Kazuya Morita1, Akira Tamase1, Hiroyuki Abe1, Kentaro Mori1, Issei Fukui1, Ryotaro Yamashita2, Mutsuki Takeda2, Tatsu Nakano2, Hiroshi Shima3, Motohiro Nomura1. Bow hunter’s syndrome treated by anterior decompression with fusion: A case report. 31-Mar-2022;13:115. Available from: https://surgicalneurologyint.com/surgicalint-articles/11503/
Abstract
Background: Bow hunter’s syndrome (BHS) is a rare condition induced by occlusion or compression of the vertebral artery (VA) during head movement or rotation. Here, we report a patient with BHS effectively treated with an anterior cervical discectomy and fusion (ACDF).
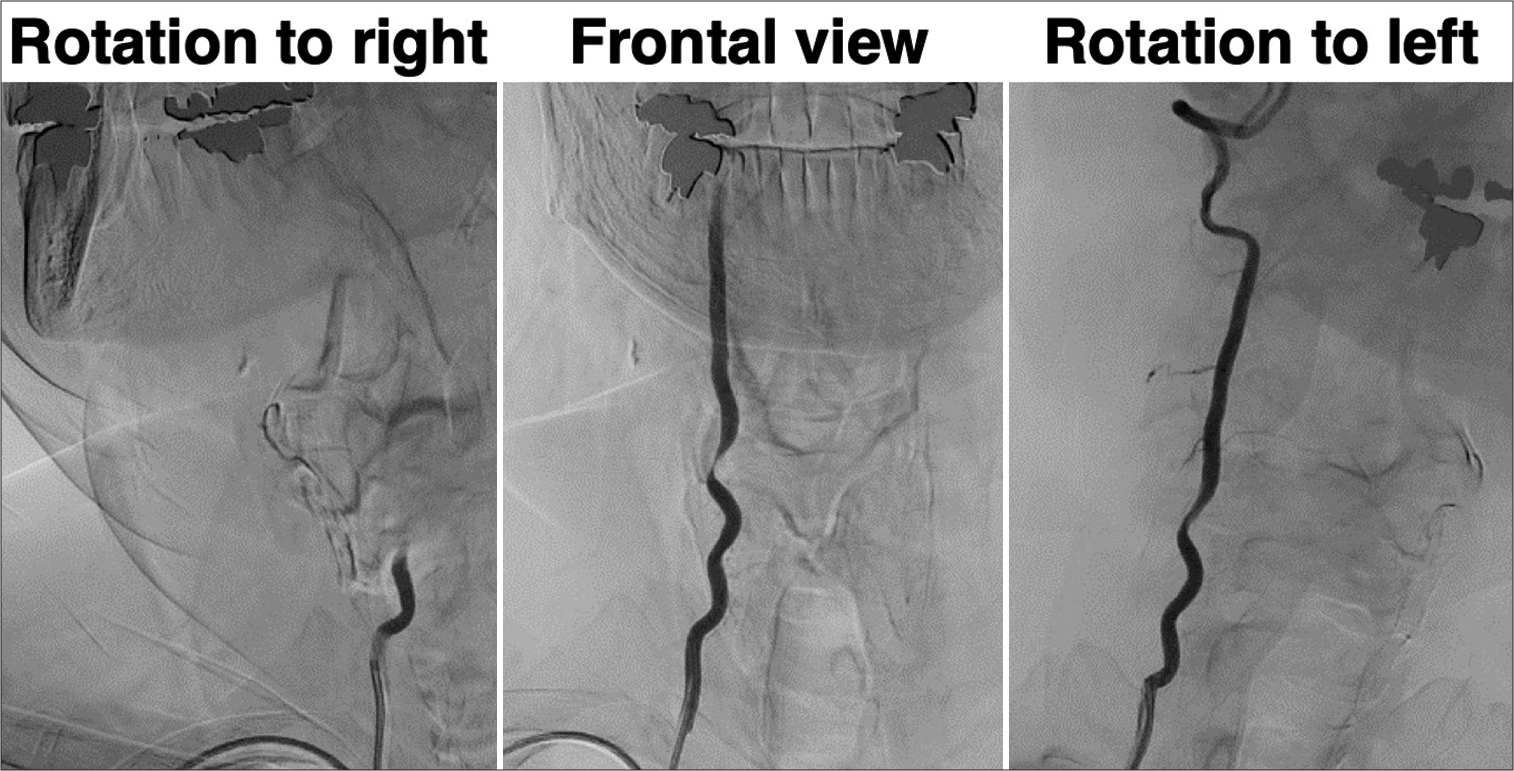
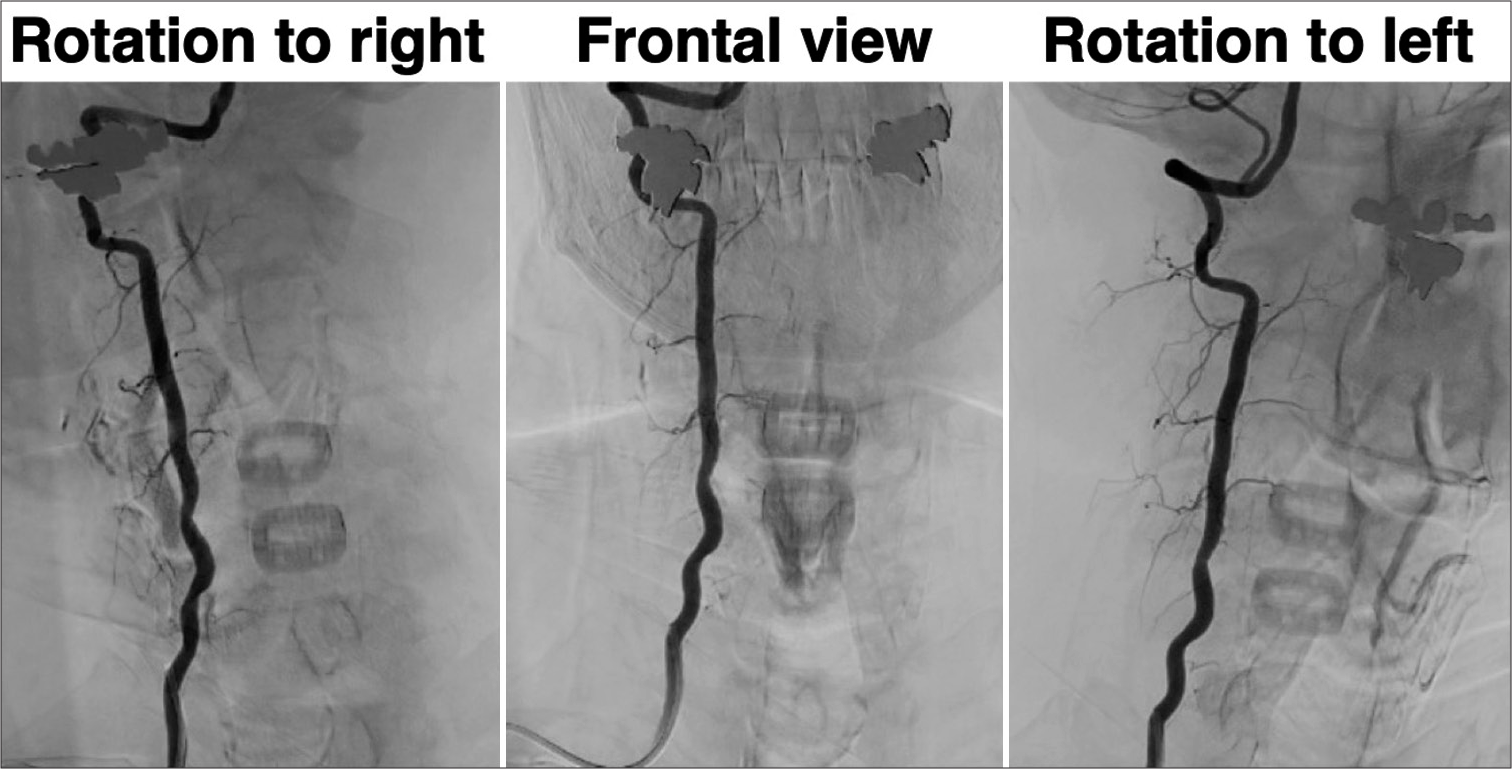
Case Description: A 75-year-old male experienced recurrent embolic strokes to the posterior circulation. This was attributed angiographically to transient stenosis of the right VA due to a right-sided C5-C6 osteophyte when the head was rotated to the right; the stenosis was improved when the patient rotated his head to the left. The patient successfully underwent a C5-C6 ACDF for removal of the right-sided lateral osteophyte which resulted in no further transient right-sided VA occlusion.
Conclusion: Following a C5-C6 ACDF for removal of a right lateral osteophyte, a 75-year-old male’s intermittent right-sided VA occlusion responsible for multiple posterior circulation emboli was relieved.
Keywords: ACDF, Bow hunter’s syndrome, Osteophyte, Repeated infarction
INTRODUCTION
Bow hunter’s syndrome (BHS) is a rare condition characterized by vertebrobasilar insufficiency associated with transient occlusion typically of the dominant vertebral artery (VA) due to bony impingement (i.e., osteophyte formation) during head movement/rotation.[
CASE PRESENTATION
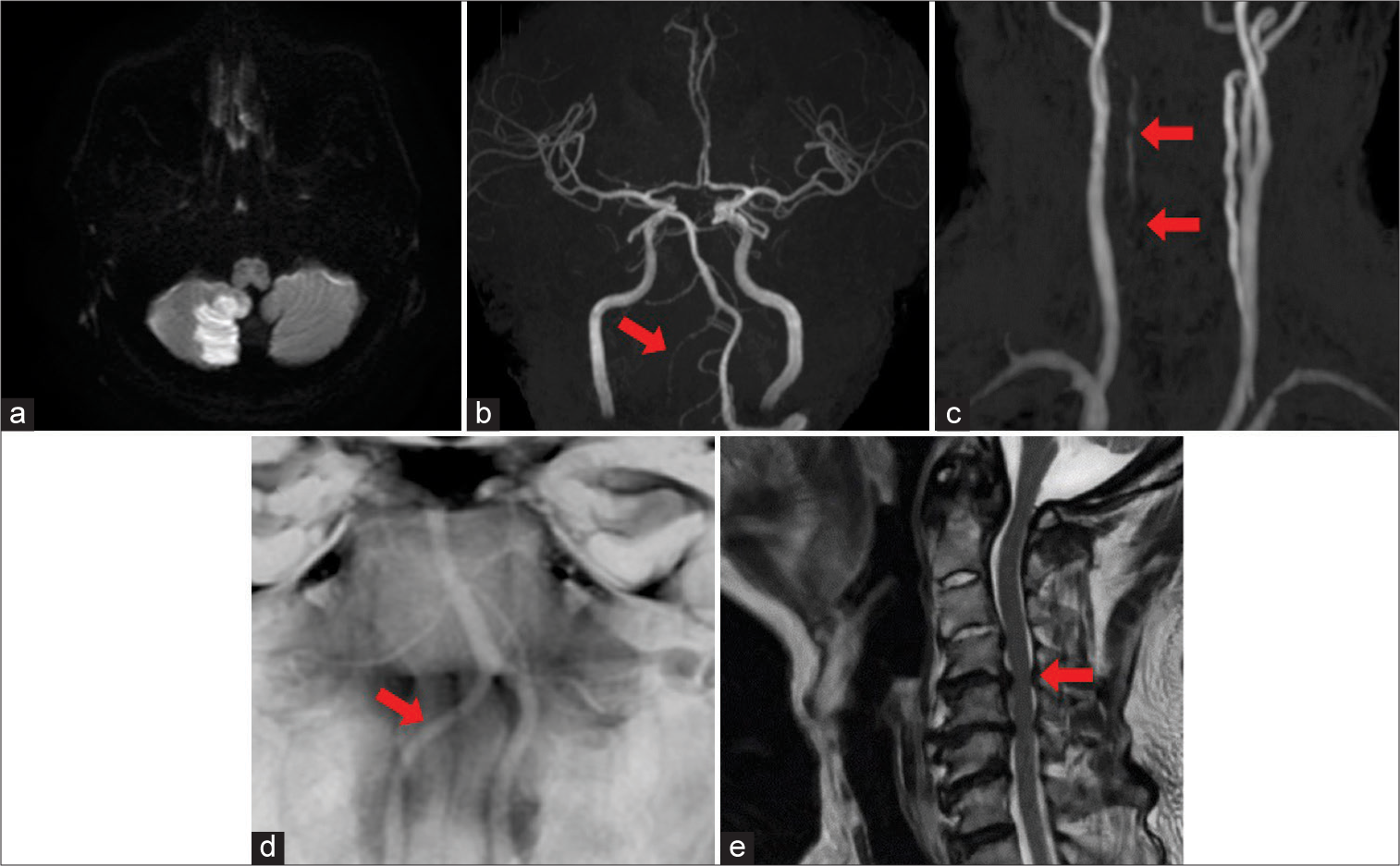
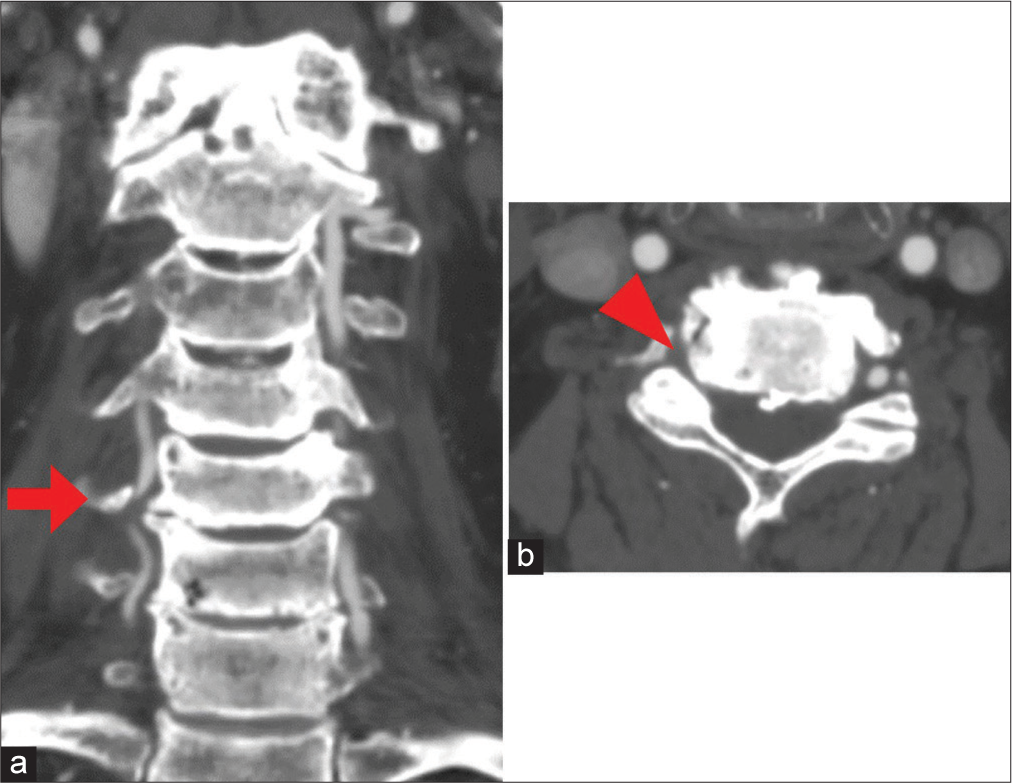
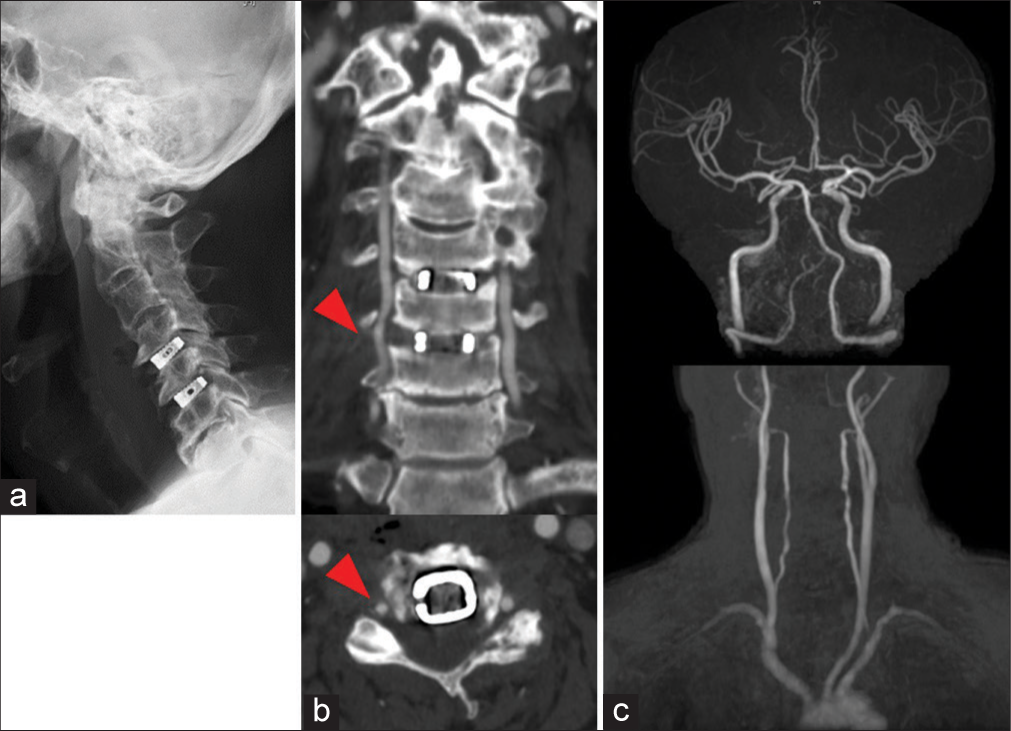
A 75-year-old male presented with the left upper limb weakness. The brain magnetic resonance images (MRI) and MR angiography (MRA) showed evidence of multiple embolic infarctions from the right VA to the right cerebellum, right parieto-occipital junction, and right occipital lobe. The cervical MRI documented significant spinal stenosis and contrast-enhanced computed tomography (CE-CT) revealed a large lateral right-sided C5-C6 osteophyte. Angiography showed it transiently compressed the right VA when the head was rotated to the right, but with relief of VA compression, when the head was rotated to the left [
Figure 1:
Magnetic resonance imaging on admission. (a) Diffusion-weighted image showing high-intensity area in the right cerebellum. (b and c) Faint opacification of the right VA (arrow). (d) BPAS demonstrating the diameter of the right VA is smaller than that of the left (arrow). (e) Stenosis of spinal canals at C4/5 (arrow) in addition to C5/6.
Surgery
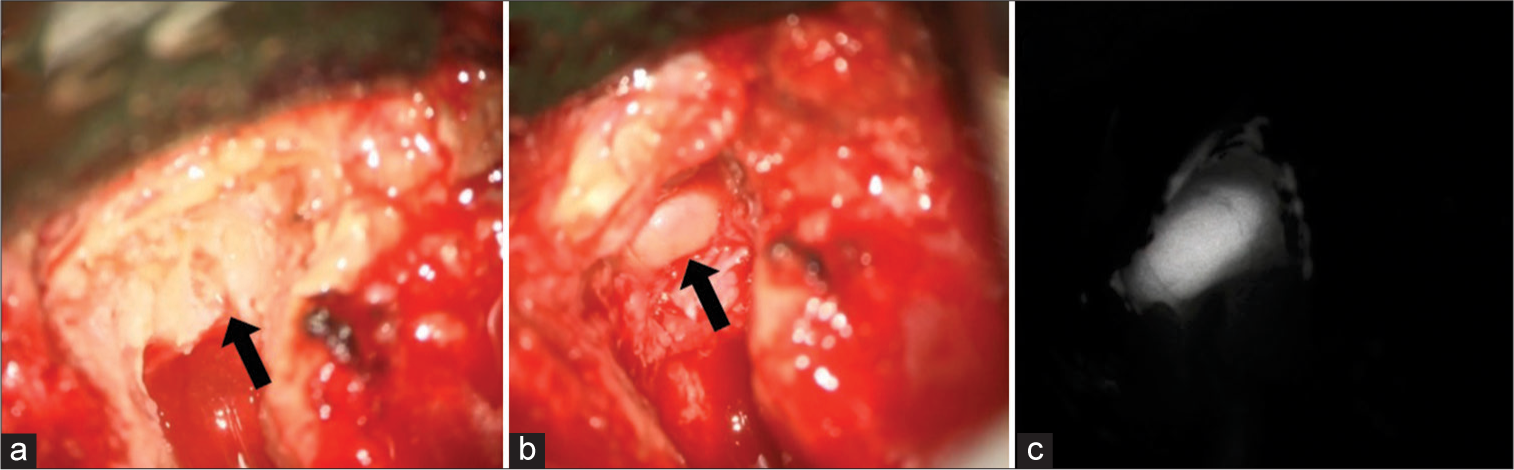
To prevent recurrent thromboembolic events, the right VA was decompressed by performing a routine C5-C6 ACDF with excision of the right-sided C5-C6 osteophyte; this successfully decompressed the right VA [
Postoperative confirmation of VA decompression
The patient’s postoperative course was uneventful. Sufficient right-sided C5-C6 osteophyte resection and right VA decompression were confirmed on the postoperative CECT and 3D-CTA [
DISCUSSION
BHS
BHS is characterized by transient symptoms induced by rotation or extension of the neck resulting in occlusion/stenosis of a VA, and resultant compromises to the posterior circulation. Symptoms typically include syncope, vertigo, dizziness, impaired vision, paresis, and pain in the extremities.[
The treatment of BHS
The treatments for BHS include anterior cervical discectomy/ corpectomy fusion with decompression/removal of osteophytes (90.6%), posterior decompression with/without fusion addressing occlusions of the V2 or V3 segments of the VA, or endovascular management (i.e., stenting for significant tortuosity of the VA without bony compression).[
CONCLUSION
A 75-year-old male with BHS due to a right-sided C5-C6 osteophyte that would transiently compress the right VA when the patient’s head was rotated to the right, presented with repeated cerebral/cerebellar posterior circulation infarctions. Following a routine C5-C6 ACDF with the right-sided osteophyte resection, the transient right VA occlusion was alleviated, and the patient’s symptoms were permanently resolved.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Iida Y, Murata H, Johkura K, Higashida T, Tanaka T, Tateishi K. Bow Hunter’s syndrome by nondominant vertebral artery compression: A case report, literature review, and significance of downbeat nystagmus as the diagnostic clue. World Neurosurg. 2018. 111: 367-72
2. Jost GF, Dailey AT. Bow Hunter’s syndrome revisited: 2 new cases and literature review of 124 cases. Neurosurg Focus. 2015. 38: E7
3. Motiei-Langroudi R, Griessenauer CJ, Alturki A, Adeeb N, Thomas AJ, Ogilvy CS. Bow Hunter’s syndrome from a tortuous V1 segment vertebral artery treated with stent placement. World Neurosurg. 2017. 98: 878.e11-5
4. Sorensen BF. Bow Hunter’s stroke. Neurosurgery. 1978. 2: 259-61
5. Strickland BA, Pham MH, Bakhsheshian J, Russin JJ, Mack WJ, Acosta FL. Bow Hunter’s syndrome: Surgical management (video) and review of the literature. World Neurosurg. 2017. 103: 953.e7-12