- Department of Neurosurgery, Military Teaching Hospital Mohammed V of Rabat, Mohammed V Faculty of Medecine and Pharmacy of Rabat, Morocco.
- Department of Radiology, Military Teaching Hospital Mohammed V of Rabat, Mohammed V Faculty of Medecine and Pharmacy of Rabat, Morocco.
- Department of Bacteriology, Military Teaching Hospital Mohammed V of Rabat, Mohammed V Faculty of Medecine and Pharmacy of Rabat, Morocco.
Correspondence Address:
Saad Moussa Elmi, Department of Neurosurgery, Military Teaching Hospital Mohammed V of Rabat, Mohammed V University of Rabat, Morocco.
DOI:10.25259/SNI_759_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Saad Moussa Elmi1, Fresnel Lutèce Ontsi Obame1, Yao Christian Hugues Dokponou1, Madina Rabileh Yassin2, Soufiyan El Attari3, Abad C. Chérif El Asri1, Miloudi Gazzaz1. Brain abscess caused by Morganella morganii: A case report and review of the literature. 12-Jan-2024;15:7
How to cite this URL: Saad Moussa Elmi1, Fresnel Lutèce Ontsi Obame1, Yao Christian Hugues Dokponou1, Madina Rabileh Yassin2, Soufiyan El Attari3, Abad C. Chérif El Asri1, Miloudi Gazzaz1. Brain abscess caused by Morganella morganii: A case report and review of the literature. 12-Jan-2024;15:7. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12706
Abstract
Background: Morganella morganii is a Gram-negative enteric rod found in the intestinal tracts of humans, mammals, and reptiles as normal flora. It is highly implicated in urinary tract infections, wound infections, and septicemia. The cerebral nervous system, especially brain abscess attributed to M. morganii, remains extremely rare. To the best of the author’s knowledge, only eight documented cerebral brain abscesses caused by M. morganii have been reported in the literature.
Case Description: A 48-year-old man presented with headache, fever, and irritability two months after endoscopic endonasal repair of the cranial base defect. Following imaging studies, a large left frontal abscess was found. The patient underwent a fine-needle aspiration through a burr hole following antimicrobial therapy.
Conclusion: We report this case to create awareness among neurosurgeons and microbiologists that M. morganii, even though uncommon, is a cause of cerebral brain abscess. Prompt surgical management and appropriate antimicrobial therapy is the treatment of choice.
Keywords: Case report, Infection, Morganella morganii
INTRODUCTION
Morganella morganii is a Gram-negative aerobe belonging to the Enterobacteriaceae family. It is normally found as a part of normal flora inhabiting the intestinal tract of humans, mammals, and reptiles. Morganella species are commonly isolated in clinical laboratories and have been implicated in urinary tract infections, wound infections, and sepsis. This bacterial species may cause pyogenic infections elsewhere in the body when it has been accidentally introduced.[
Nevertheless, it is an extremely rare pathogen of cerebral nervous system (CNS) infection, especially brain abscess, with only eight documented cases.[
Herein, we present the case of a 48-year-old man with an isolated brain abscess caused by M. morganii, which was successfully managed by surgical aspiration followed by antimicrobial therapy.
CASE REPORT
Clinical presentation
A 48-year-old man presented with a headache and fever. This man had a medical history of cranial base defect situated in the cribriform plate, which was successfully repaired by endoscopic endonasal technique two months earlier. There was no history of otalgia, otorrhea, sinusitis, or urinary infection. At admission, the patient was conscious with a Glasgow coma scale of 15 with a cognitive impairment such as irritability and reduced verbal output suggestive of a frontal lobe syndrome. There was no focal neurological deficit.
Diagnosis assessment
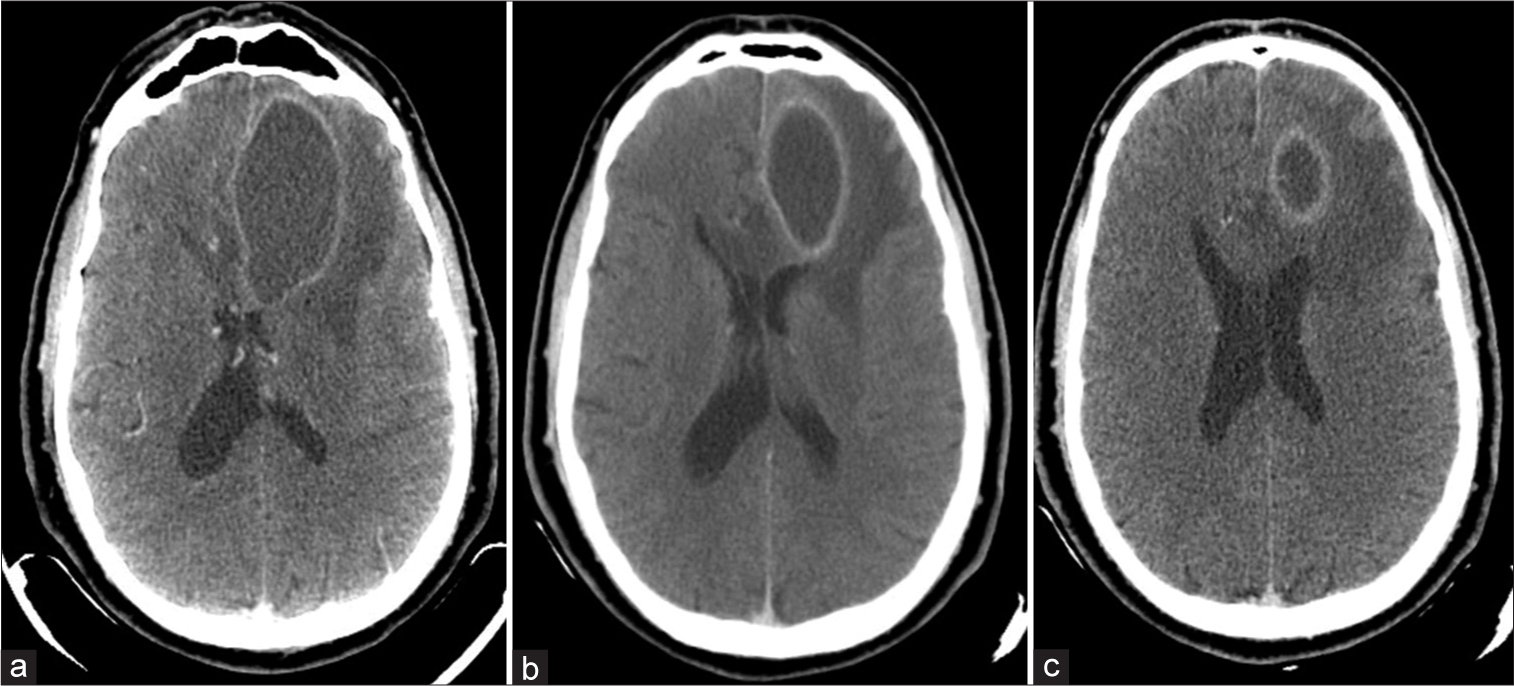
Computed tomography (CT) of the head with and without contrast was performed. It demonstrated a left frontal abscess characterized by a hypodense center, a hyperdense ring with marked perilesional hypodense area suggestive of edema [
The blood laboratory test was normal.
Therapeutic intervention
The patient underwent needle aspiration of the brain abscess through a left frontal burr hole. The pus sample was collected and sent to the microbiology laboratory for analysis, and the patient was started on empiric antimicrobial therapy.
Follow-up
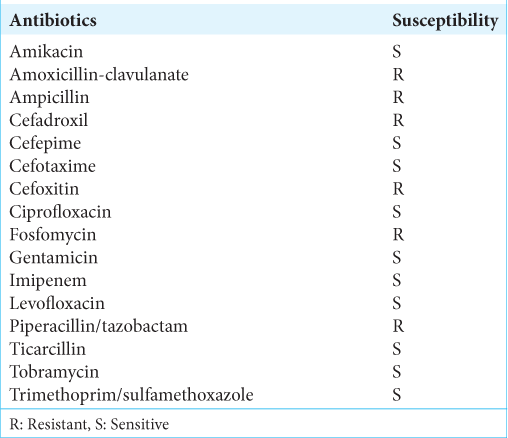
Antimicrobial identification and testing revealed M. morganii susceptible to ticarcillin, imipenem, aminoglycosides, quinolones, and third-generation cephalosporins [
The patient was treated with intravenous Ceftriaxone and Flagyl. Despite abscess aspiration and antibiotic treatment, the patient continued to be symptomatic. A repeat CT scan of the brain one week after the first aspiration was performed and showed a recollection of the abscess, which required a second aspiration. Intravenous antibiotics were changed to imipenem and continued for a total of 6 weeks.
The third CT scan [
DISCUSSION
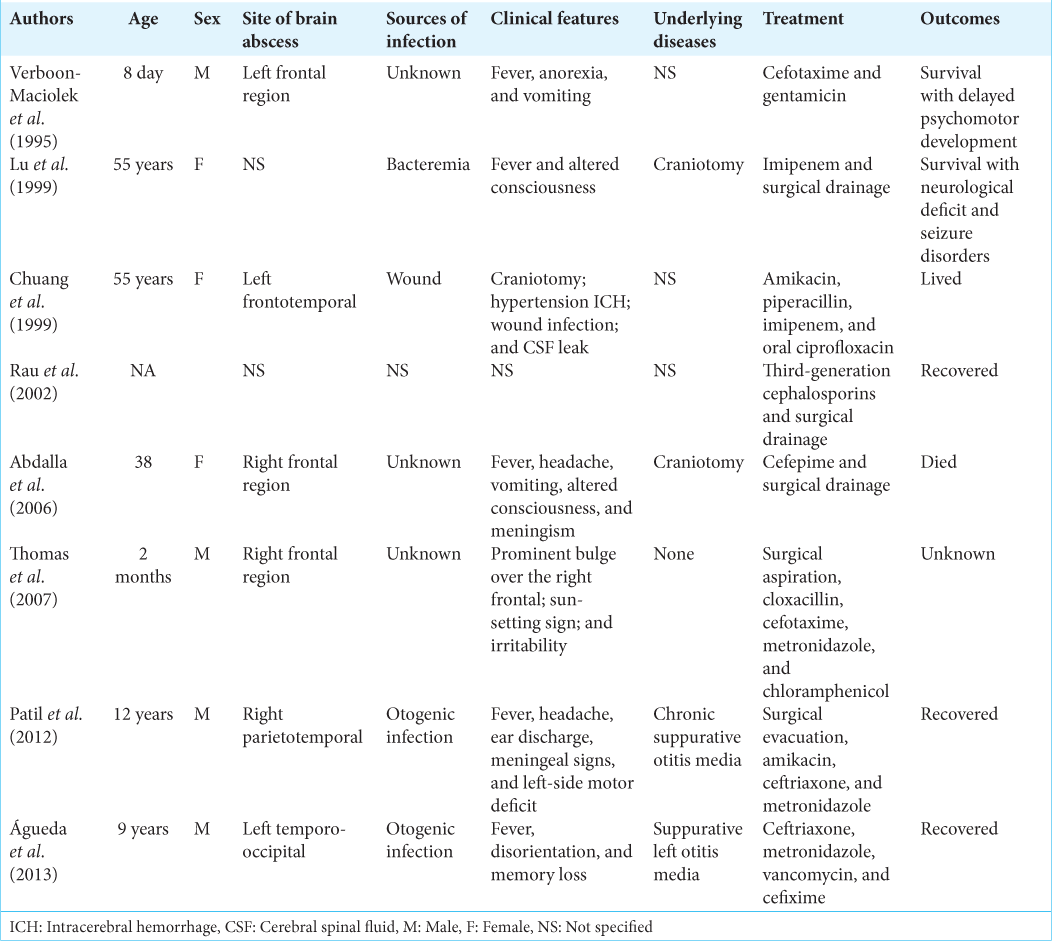
M. morganii is a rare causative pathogen in CNS infections, especially brain abscesses. In a review of the literature, we found only nine cases, including our cerebral brain abscess caused by M. morganii reported since the first reported case by Verboon-Maciolek et al., in 1995,[
The successful treatment of a brain abscess requires a combination of both medical and surgical approaches. However, the surgical approach has a pivotal role in the management of brain abscesses. Our patient underwent a needle aspiration. The previous reports showed that the advantages of aspiration are simplicity, reduced morbidity, and the fact that it can be carried out at any stage of the evolution of the abscess. Initial therapy should be commenced with broad-spectrum antibiotics that cross the blood–brain and blood-cerebral spinal fluid barriers in adequate concentrations. After the pus is drained and the antibiotic sensitivity reports become available, specific bactericidal agents for the cultured organism should be administered. M. morganii is usually susceptible to third-generation cephalosporins and aminoglycosides. It is characteristically resistant to many beta-lactam antibiotics. In this case, the patient responded well to the surgical aspiration, followed by appropriate antibiotic therapy.
CONCLUSION
We report this case to create awareness among neurosurgeons and microbiologists that M. morganii, even though uncommon, is a cause of cerebral brain abscess; a high index of suspicion is required when a patient with brain abscess has previously undergone endoscopic endonasal surgery.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that appropriate patient consent has been obtained.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of Artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abdalla J, Saad M, Samnani I, Lee P, Moorman J. Central nervous system infection caused by Morganella morganii. Am J Med Sci. 2006. 331: 44-7
2. Águeda S, Leitão A, Rocha G, Guimarães H. Cerebral abscess and empyema due to Morganella morganii. Pediatr Ther. 2013. 3: 147
3. Chuang YC, Chang WN, Huang CR, Chen HJ. Morganella morganii central nervous system infection: Case report and review. Infect Dis Clin Pract. 1999. 8: 50-1
4. Lu CH, Chang WN, Chuang YC. Resistance to third-generation cephalosporins in adult gram-negative bacillary meningitis. Infection. 1999. 27: 208-11
5. Patil AB, Nadagir SD, Lakshminarayana S, Syeda FM. Morganella morganii subspecies morganii, biogroup a: An unusual causative pathogen of brain abscess. J Neurosci Rural Pract. 2012. 3: 370-2
6. Rau CS, Chang WN, Lin YC, Lu CH, Liliang PC, Su TM. Brain abscess caused by aerobic Gram-negative Bacilli: Clinical features and therapeutic outcomes. Clin Neurol Neurosurg. 2002. 105: 60-5
7. Thomas VA, Sathish KT, Agarwal I, Chacko AG. Unusual cause of brain abscess in an infant. J Pediatr Neurosci. 2007. 2: 94-5
8. Verboon-Maciolek M, Vandertop WP, Peters AC, Roord JJ, Geelen SP. Neonatal brain abscess caused by Morganella morgagni. Clin Infect Dis. 1995. 20: 471