- Department of Neurosurgery, Shizuoka City Shimizu Hospital, Shizuoka,
- Department of Pathology, Keio University School of Medicine, Tokyo, Japan.
Correspondence Address:
Shinya Ichimura
Department of Neurosurgery, Shizuoka City Shimizu Hospital, Shizuoka,
DOI:10.25259/SNI_79_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kento Takahara, Yoichi Mochizuki, Shinya Ichimura, Yutaka Kurebayashi, Koji Fujii. Brain metastasis from urachal carcinoma. 02-Aug-2019;10:152
How to cite this URL: Kento Takahara, Yoichi Mochizuki, Shinya Ichimura, Yutaka Kurebayashi, Koji Fujii. Brain metastasis from urachal carcinoma. 02-Aug-2019;10:152. Available from: http://surgicalneurologyint.com/surgicalint-articles/9556/
Abstract
Background: Urachal carcinoma (UC) is a rare variant of bladder carcinoma. Only seven cases of brain metastasis from UC have been reported in the literature thus far.
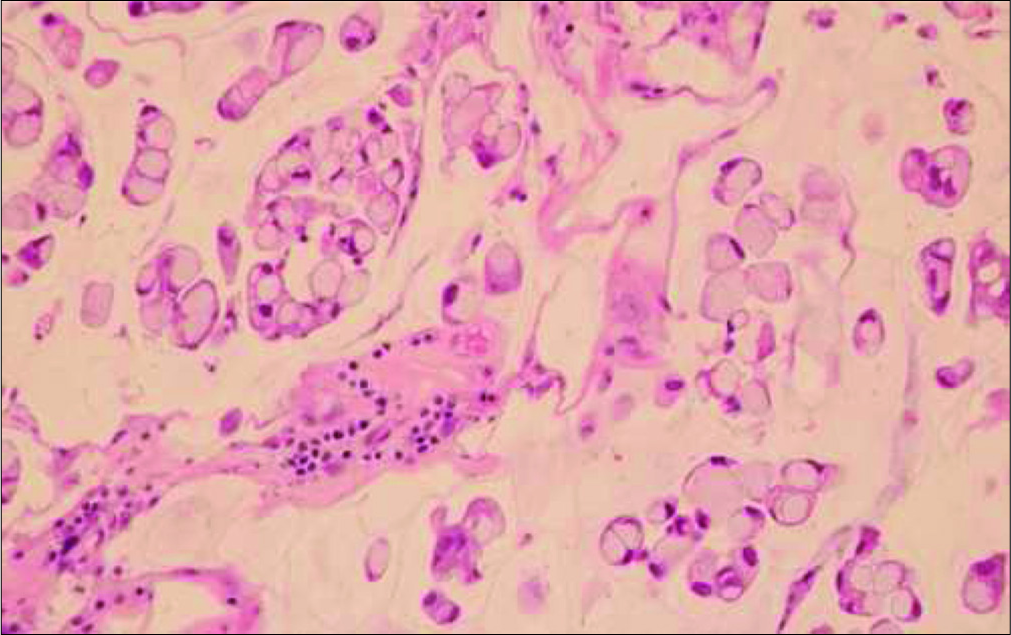
Case Description: A 77-year-old female was diagnosed with a brain tumor in her left cerebellum 2 years after she underwent surgery for a primary UC in the bladder. Surgery was performed via a midline suboccipital approach and the tumor was totally removed. The excised lesion was pathologically diagnosed as a metastasis and displayed typical pathological features of urachal adenocarcinoma with abundant mucin mixed with signet ring cells. A recurrence was observed at the site of tumor removal 6 months after surgery, and then, gamma knife radiotherapy was performed to the lesion.
Conclusion: According to the five previously reported similar cases and our case, tumor removal is the treatment of choice. Routine whole brain radiotherapy is not the best treatment choice; however, local radiotherapy including conventional local radiotherapy or gamma knife radiotherapy could be implemented instead.
Keywords: Brain metastasis, Radiotherapy, Urachal carcinoma
INTRODUCTION
Urachal carcinoma (UC) is a rare urological tumor, accounting for 0.17–0.34% of all bladder carcinomas.[
CASE REPORT
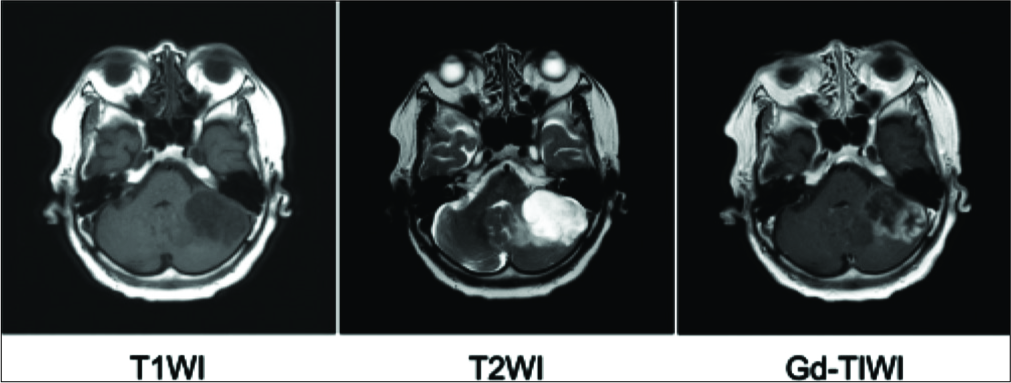
A 77-year-old female had been diagnosed with UC and had undergone total cystectomy 2 years prior to presentation with dizziness for which she was referred to our department. Magnetic resonance imaging revealed a 35-mm sized lesion in the left cerebellum. This lesion showed low intensity on T1-weighted images, high intensity with perifocal edema on T2-weighted images, and avid heterogeneous enhancement on T1-weighted images after gadolinium administration [
Figure 1:
Preoperative magnetic resonance imaging showing a 35-mm sized mass in the left cerebellum that showed low intensity on T1-weighted image (left), high intensity with perifocal oedema on T2-weighted image (middle), and heterogeneous enhancement on T1-weighted image with gadolinium administration (right).
DISCUSSION
UC is a rare variant of bladder carcinoma which differs from normal bladder carcinoma in several ways: Instead of arising from the urothelium, it is believed to originate from an urachal remnant that underwent intestinal metaplasia or from progenitor cells of the cloaca left behind during embryologic development. This theory is reflected in the pathohistological differences observed between these two cancer types.[
Generally speaking, UC is treated in a way comparable to normal bladder carcinoma. Surgery is the treatment of choice, whereas chemotherapy and radiotherapy can be chosen for advanced cases. In cases with infiltration of adjacent organs or with distant or lymph node metastasis, poor prognosis is expected; the 5-year survival rate is believed to be 20% or less.[
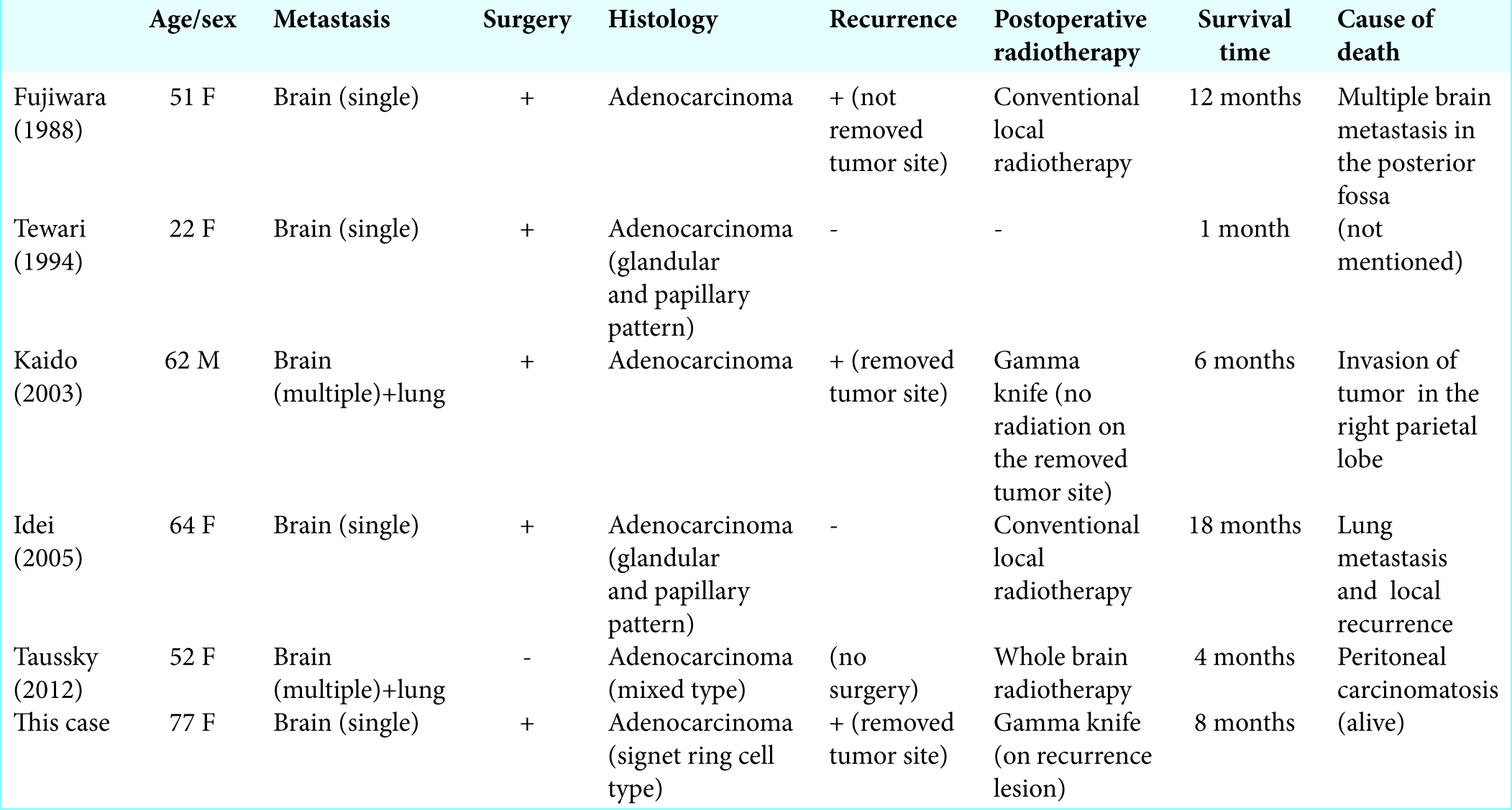
As of now, seven cases of brain metastasis from UC have been reported.[
According to the five cases and our own case, the efficacy of radiotherapy remains unclear. Whole brain radiotherapy was provided in one case for multiple lesions, but there was no effect on tumor size.[
CONCLUSION
We reported a rare case of brain metastasis from urachal carcinoma. According to the five previously reported similar cases and our case, tumor removal is the treatment of choice. Routine whole brain radiotherapy is not the best treatment choice; however, local radiotherapy including conventional local radiotherapy or gamma knife radiotherapy could be implemented instead.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arakawa Y, Inoue D, Sakuyama T, Nagasaki E, Aiba K. Strontium-89 therapy and subarachnoid phenol block successfully eliminated intractable pain of metastasis in the patient with advanced urachal carcinoma. Gan To Kagaku Ryoho. 2011. 38: 59-60
2. Behrendt MA, van Rhijn BW. Genetics and biological markers in urachal cancer. Transl Androl Urol. 2016. 5: 655-61
3. Bruins HM, Visser O, Ploeg M, Hulsbergen-van de Kaa CA, Kiemeney LA, Witjes JA. The clinical epidemiology of urachal carcinoma: Results of a large, population based study. J Urol. 2012. 188: 1102-7
4. DeGeorge KC, Holt HR, Hodges SC. Bladder cancer: Diagnosis and treatment. Am Fam Phys. 2017. 96: 507-14
5. Fujiwara S, Takaki T, Hikita T, Kanzaki H, Kuroiwa S. Brain metastasis from urachal carcinoma. Surg Neurol. 1988. 29: 475-6
6. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M. The global burden of cancer 2013. JAMA Oncol. 2015. 1: 505-27
7. Hirshman BR, Wilson B, Ali MA, Proudfoot JA, Koiso T, Nagano O. Superior prognostic value of cumulative intracranial tumor volume relative to largest intracranial tumor volume for stereotactic radiosurgery-treated brain metastasis patients. Neurosurgery. 2018. 82: 473-80
8. Idei M, Urasaki E, Yokota A. Metastatic brain tumor originating from urachal carcinoma: Case report. No Shinkei Geka. 2005. 33: 1015-9
9. Kaido T, Uemura H, Hirao Y, Uranishi R, Nishi N, Sakaki T. Brain metastases from urachal carcinoma. J Clin Neurosci. 2003. 10: 703-5
10. Lin X, DeAngelis LM. Treatment of brain metastases. J Clin Oncol. 2015. 33: 3475-84
11. Moreno AJ, Rebollo CG, Calle FA, Villa LP, Carrillo JJ, Villalta EJ. Urachal adenocarcinoma with late brain metastases. Arch Esp Urol. 2010. 63: 550-4
12. Mylonas KS, O Malley P, Ziogas IA, El-Kabab L, Nasioudis D. Malignant urachal neoplasms: A population-based study and systematic review of literature. Urol Oncol. 2017. 35: 33-3
13. Sheldon CA, Clayman RV, Gonzalez R, Williams RD, Fraley EE. Malignant urachal lesions. J Urol. 1984. 131: 1-8
14. Taussky D, Karakiewicz PI, Latour M, Blais N. Brain metastasis from urachal carcinoma: The importance of locally aggressive treatment. Rare Tumors. 2012. 4: e17-
15. Tewari MK, Khosla VK, Sharma BS, Vashistha RK, Khandelwal NK, Kak VK. Brain metastasis from urachal carcinoma: Case report. Surg Neurol. 1994. 42: 340-2