- Department of Neurosurgery, University Hospitals Leuven, Leuven, Belgium.
- Department of Pediatrics, University Hospitals Leuven, Leuven, Belgium.
Correspondence Address:
Tom Deleu, Department of Neurosurgery, University Hospitals Leuven, Leuven, Belgium.
DOI:10.25259/SNI_1016_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tom Deleu1, Katrien Jansen2, Frank Van Calenbergh1. Brain overgrowth associated with megalencephaly-capillary malformation syndrome causing progressive Chiari and syringomyelia. 20-May-2022;13:211
How to cite this URL: Tom Deleu1, Katrien Jansen2, Frank Van Calenbergh1. Brain overgrowth associated with megalencephaly-capillary malformation syndrome causing progressive Chiari and syringomyelia. 20-May-2022;13:211. Available from: https://surgicalneurologyint.com/surgicalint-articles/11605/
Abstract
Background: Megalencephaly-capillary malformation (M-CM) syndrome is a rare overgrowth syndrome characterized by macrocephaly, port-wine stains, asymmetric brain growth, hydrocephalus, and developmental delay. Cerebellar tonsil herniation is often seen, but rarely with syringomyelia.
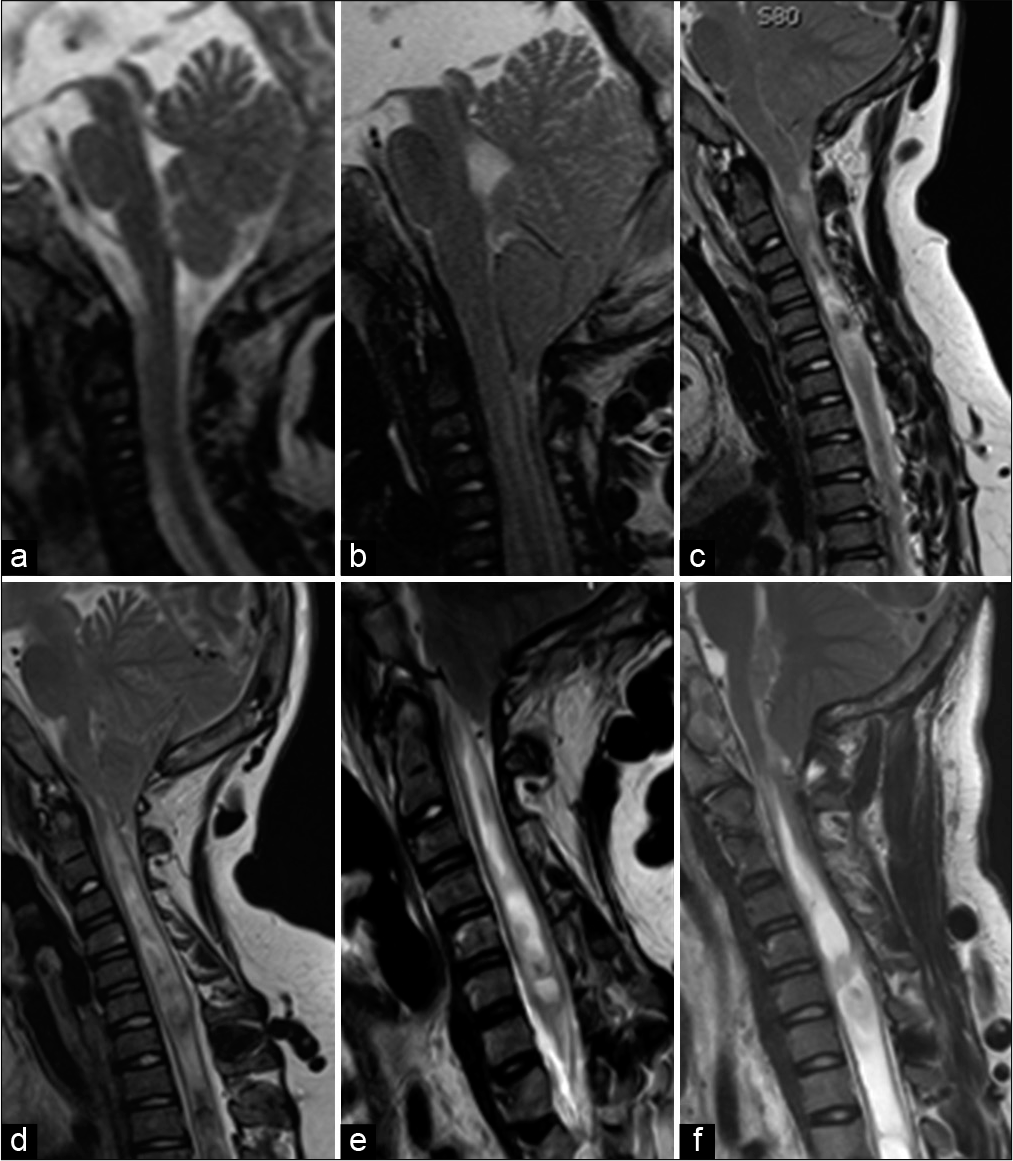
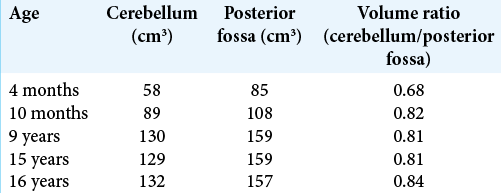
Case Description: A newborn with M-CM syndrome developed a progressive Chiari malformation type I (CM-I) with syringomyelia. At 4 months, he was treated for subdural hematomas, while at 10 months, he required a shunt for hydrocephalus. At 16 years of age, he newly presented a left hemiparesis and ataxia. Notably, successive volumetric measurements of the posterior fossa/cerebellum showed disproportionate cerebellar growth over time that correlated with the appearance of a CM-I. Following a suboccipital craniectomy with C1-laminectomy and duraplasty, he neurologically improved.
Conclusion: M-CM with CM-I and syringomyelia rarely present together. Here, we treated an infant with M-CM who developed a progressive CM-I malformation and syringomyelia reflecting disproportionate growth of the cerebellum/posterior fossa over a 16-year period.
Keywords: Chiari I malformation, Megalencephaly-capillary malformation, Overgrowth syndromes, Syringomyelia
INTRODUCTION
Macrocephaly-cutis marmorata telangiectatica congenita (M-CMTC) is a rare condition. It is characterized by macrocephaly, port-wine stains, asymmetric growth, polydactyly, joint hyperlaxity, and central nervous system abnormalities (i.e., including hydrocephalus and developmental delay).[
CASE REPORT
A male infant, diagnosed with M-CMTC/M-CM, presented with diffuse capillary malformations on his face, neck, shoulders, and limbs at birth. At 4 months of age, the MRI showed progressive macrocrania with large subdural hematomas requiring evacuation. Volumetric measurements of the posterior fossa and cerebellum on sequential MRI’s (i.e., using the iPlan™ software [Brainlab AG, Munich, Germany]) were performed. They showed a steep rise in the ratio of cerebellar to posterior fossa volume between the MRI at 4 months and at 10 months that coincided with the appearance of a CM-I [
DISCUSSION
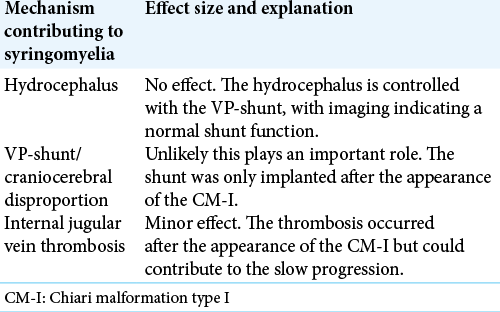
Syringomyelia
Seventy percent of M-CM patients have a CM-I,[
Vascular malformations
Vascular malformations are one of the two main features of the M-CM syndrome.[
CONCLUSION
An infant presented with M-CM syndrome; at 4 months, he had subdural hematomas, and at 10 months, hydrocephalus requiring shunt placement. Over the subsequent 16-year follow-up, and due to disproportionate growth of the cerebellum and posterior fossa, he developed a progressive CM-I malformation and holocord syringomyelia warranting a suboccipital craniectomy and C1 laminectomy, with duraplasty.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arnautovic A, Splavski B, Boop FA, Arnautovic KI. Pediatric and adult Chiari malformation Type I surgical series 1965-2013: A review of demographics, operative treatment, and outcomes. J Neurosurg Pediatr. 2015. 15: 161-77
2. Clayton-Smith J, Kerr B, Brunner H, Tranebjaerg L, Magee A, Hennekam RC. Macrocephaly with cutis marmorata, haemangioma and syndactyly a distinctive overgrowth syndrome. Clin Dysmorphol. 1997. 6: 291-302
3. Conway RL, Pressman BD, Dobyns WB, Danielpour M, Lee J, Sanchez-Lara PA. Neuroimaging findings in Macrocephaly-Capillary malformation: A longitudinal study of 17 patients. Am J Med Genet A. 2007. 143: 2981-3008
4. Martínez-Glez V, Romanelli V, Mori MA, Gracia R, Segovia M, González-Meneses A. Macrocephaly-capillary malformation: Analysis of 13 patients and review of the diagnostic criteria. Am J Med Genet A. 2010. 152A: 3101-6
5. Mirzaa GM, Conway RL, Gripp KW, Lerman-Sagie T, Siegel DH, deVries LS. Megalencephaly-capillary malformation (MCAP) and megalencephaly-polydactyly-polymicrogyriahydrocephalus (MPPH) syndromes: Two closely related disorders of brain overgrowth and abnormal brain and body morphogenesis. Am J Med Genet A. 2012. 158A: 269-91
6. Patel PN, Levi JR, Cohen MB. Lemierre’s syndrome in the pediatric population: Trends in disease presentation and management in literature. Int J Pediatr Otorhinolaryngol. 2020. 136: 110213
7. Rivière JB, Mirzaa GM, O’Roak BJ, Beddaoui M, Alcantara D, Conway RL. De novo germline and postzygotic mutations in AKT3, PIK3R2 and PIK3CA cause a spectrum of related megalencephaly syndromes. Nat Genet. 2012. 44: 934-40
8. Strahle J, Muraszko KM, Kapurch J, Bapuraj JR, Garton HJ, Maher CO. Chiari malformation Type I and syrinx in children undergoing magnetic resonance imaging: Clinical article. J Neurosurg Pediatr. 2011. 8: 205-13
9. Wright DR, Frieden IJ, Orlow SJ, Shin HT, Chamlin S, Schaffer JV. The misnomer “macrocephaly-cutis marmorata telangiectatica congenita syndrome” report of 12 new cases and support for revising the name to macrocephaly-capillary malformations. Arch Dermatol. 2009. 145: 287-93