- Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY 11530, United States and Editor-in-Chief of Surgical Neurology International.
Correspondence Address:
Nancy E. Epstein M.D., F.A.C.S., Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY 11530, United States and Editor-in-Chief of Surgical Neurology International.
DOI:10.25259/SNI_175_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. Can anterior cervical diskectomy/fusion (ACDF) be safely performed in ambulatory surgical centers (ASC’s)?. 31-Mar-2023;14:110
How to cite this URL: Nancy E. Epstein. Can anterior cervical diskectomy/fusion (ACDF) be safely performed in ambulatory surgical centers (ASC’s)?. 31-Mar-2023;14:110. Available from: https://surgicalneurologyint.com/surgicalint-articles/12232/
Abstract
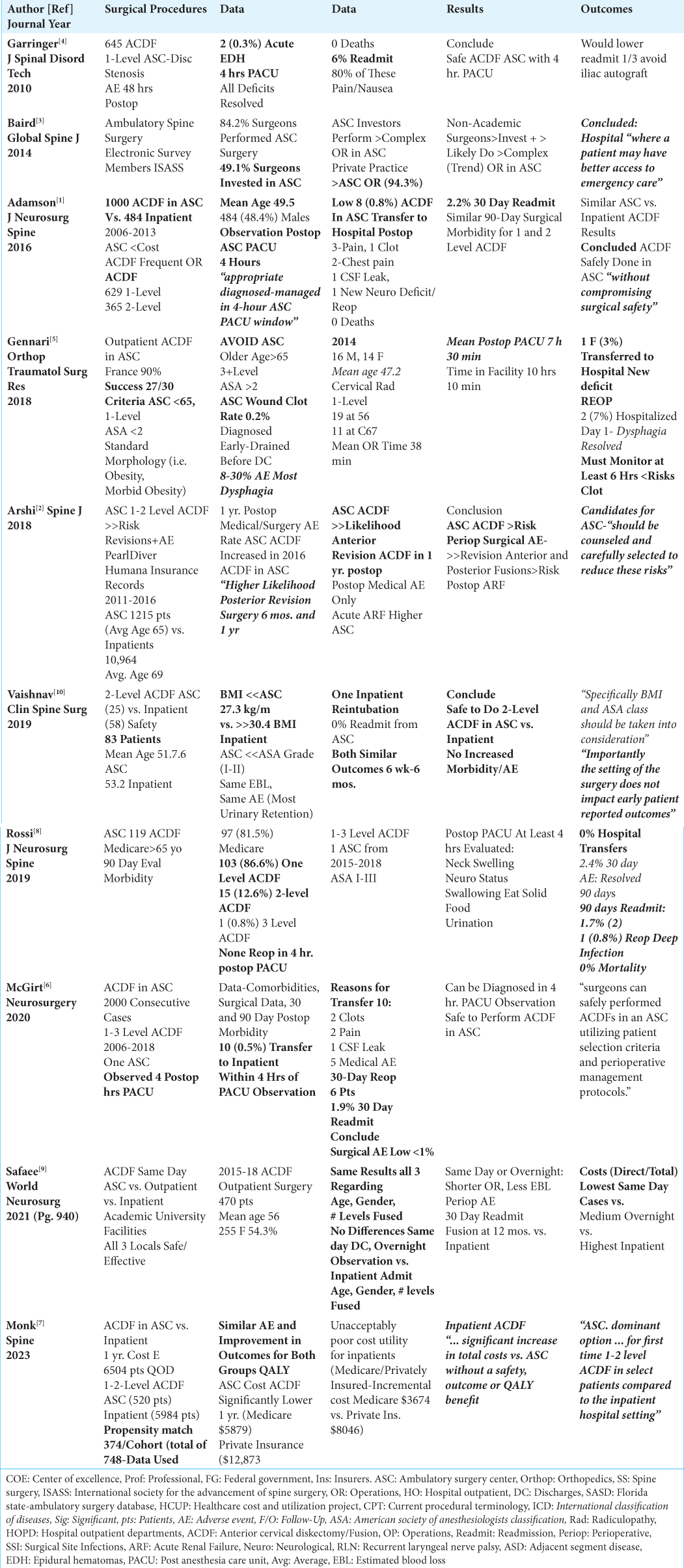
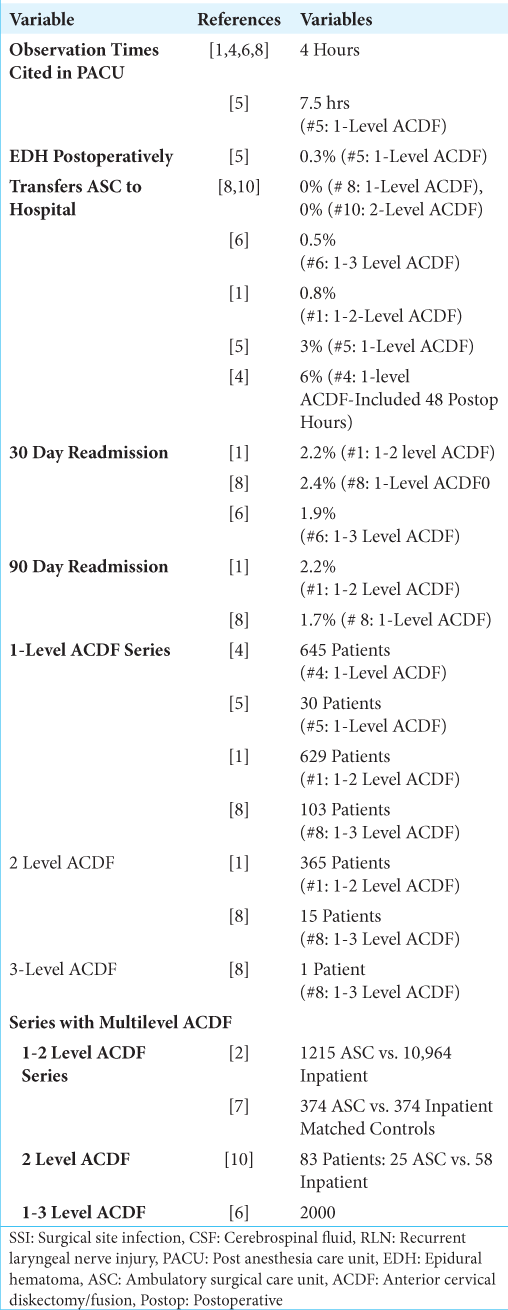
Background: Can anterior cervical diskectomy/fusion (ACDF) be safely performed in ambulatory surgical centers (ASC’s: i.e. discharges 4-7.5 hr. postoperatively) that meet the following stringent “exclusion criteria”; elevated Body Mass Index (BMI), major comorbidities, age > 65, American Society of Anesthesiology (ASA) scores > II, and largely multilevel ACDF.
Materials: Presently, most ACDF are still being performed in hospital-based outpatient surgical centers (HBSC: utilizing 23-hour stays), or as inpatients.
Results: Notably, unreliable disparate study designs involving very different patient populations resulted in nearly comparable, but implausible outcomes for 1-level vs. multilevel ACDF series performed in ASC. A summary of these outcome data included the following rates of; i.e. postoperative hospital transfers (0-6%), 30-day (up to 2.2%), and up to 90 day (2.2%) emergency department (ED) visits, readmissions, and reoperations.
Conclusion: Nevertheless, it is just common sense that “less should be less”, that 1-level ACDF should involve less risk compared with multilevel ACDF procedures performed in ASC.
Keywords: Adverse events, Ambulatory surgi-center (ASC), Anterior cervical diskectomy/fusion (ACDF), Efficacy, Hospital-based outpatient surgi-center (HBSC), Inpatient facility, Morbidity, Outcomes, Safety, Single vs multilevel
INTRODUCTION
Can anterior cervical diskectomy/fusions (ACDF) be safely performed in ambulatory surgical centers (ASC- discharges 4-7.5 hrs. postoperatively) adhering to “stringent exclusion criteria”. As outlined in many studies, these exclusion criteria included; avoiding elevated BMI (i.e. obesity/ morbid obesity, non-routine “morphology”), major comorbidities, age > 65, American Society of Anesthesiology (ASA) scores > II, and as raised by Gennari et al., multilevel ACDF?[
“Careful Patient Selection” for ACDF Surgery in ASC Using Multiple “Exclusion Criteria”
Two Studies Emphasized Inclusion/Exclusion Criteria for 1-level ACDF to Be Performed in ASC
Two studies emphasized careful patient selection utilizing multiple “inclusion” and “exclusion criteria” for performing 1-level ACDF in ASC [
Three Studies Emphasized Inclusion/Exclusion Criteria for Multilevel ACDF to be Performed in ASC
Three studies emphasized careful patient selection utilizing multiple “inclusion” and “exclusion criteria” for performing multilevel ACDF/mixed procedures in ASC [
Medicolegal Suits Due to Ignoring Exclusion Criteria for ACDF Surgery Performed in ASC
Experience with two medicolegal suits reviewed by this neurosurgeon highlight how critical it is to follow exclusion criteria when choosing to performing ACDF in ASC. In the first case, a morbidly obese alcoholic underwent a 1-level ACDF in an ASC; within 2 hours of discharge to home, he sustained a fatal cardiorespiratory arrest. A second patient, over 65 years of age, underwent a multilevel ACDF in an ASC, and was discharged home within less than the requisite 4 hour postoperative observation window despite an excessive amount of Jackson-Pratt drainage. He too sustained a cardiac arrest at home, but remained vegetative for over 1 year before expiration. Notably, there must be many other “unreported” cases of ACDF being negligently performed in ASC (i.e. failure to follow “exclusion criteria”) resulting in irrevocable patient harm.
Nearly Comparable Morbidity Rates for 1-Level vs. Multilevel ACDF Performed in ASC: This Makes No Sense as “Less (Surgery) Should Be Less (Morbidity)”
First, Documentation of Safe Performance of 1-Level and/ or Multilevel ACDF in ASC
Several studies documented the relative safety of performing 1-level vs. multilevel ACDF in ASC (same day discharges) [
Rates for Multilevel ACDF Compared with Single-Level ACDF Makes No Sense
Despite differences in immediate postoperative hospital transfer rates for 1-level vs. multilevel ACDF performed in ASC (i.e. 0-6% for 1-level vs. 0-0.8% for multilevel procedures), our analysis of these studies showed nearly comparable 30-day (1.9-2.4%), and 90 day ED visits, readmissions, and reoperation rates (1.7-2.2%) [
Difficulty Comparing Variable Study Designs Involving Different Patient Populations
We had difficulty comparing results of 1-level vs. multilevel ACDF performed in ASC due to marked variability in study designs resulting in operations being performed on fundamentally different patient populations.
Results of 1-level ACDF Performed in ASC
Two studies looked specifically at the results of 1-level ACDF performed in ASC [
Results for 1 to 2-level ACDF Performed in ASC
Several series looked at results for patients undergoing 1-2 level ACDF in ASC [
Results for 2-level ACDF Performed in ASC vs. Inpatient
Vaishnav et al. (2019) compared outcomes for 2-level ACDF performed in ASC vs. as inpatients; despite significant differences including lower BMI and lower ASA scores for ASC patients, they found similar outcomes at 6 postoperative weeks and 6 postoperative months [
Results of 1 to 3-level ACDF Performed in ASC
When McGirt et al. (2020) performed 2000 consecutive 1-3 level ACDF in an ASC utilizing a 4 h. PACU observation window, 10 (0.5%) patients required immediate postoperative hospital transfers for; 2 hematomas, 2 with pain alone, 1 CSF leak, and 5 medical adverse events [
Concern About More Complex Spine Surgery Being Performed in ASC
Baird et al. (2014) observed that 84.2% of spine surgeons now work in ASC, with 49.1% being invested in these facilities [
CONCLUSION
Different study designs showed nearly comparable outcomes for patients undergoing 1-level vs. multilevel ACDF performed in ASC. Nevertheless, common sense should dictate that “less (surgery) should be less (morbidity)”, meaning 1-level ACDF should involve less surgical risk vs. multilevel procedures performed in ASC.[
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Adamson T, Godil SS, Mehrlich M, Mendenhall S, Asher AL, McGirt MJ. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: Analysis of 1000 consecutive cases. J Neurosurg Spine. 2016. 24: 878-84
2. Arshi A, Wang C, Park HY, Blumstein GW, Buser Z, Wang JC. Ambulatory anterior cervical discectomy and fusion is associated with a higher risk of revision surgery and perioperative complications: An analysis of a large nationwide database. Spine J. 2018. 18: 1180-7
3. Baird EO, Brietzke SC, Weinberg AD, McAnany SJ, Qureshi SA, Cho SK. Ambulatory spine surgery: A survey study. Global Spine J. 2014. 4: 157-60
4. Garringer SM, Sasso RC. Safety of anterior cervical discectomy and fusion performed as outpatient surgery. J Spinal Disord Tech. 2010. 23: 439-43
5. Gennari A, Mazas S, Coudert P, Gile O, Vital JM. Outpatient anterior cervical discectomy: A French study and literature review. Orthop Traumatol Surg Res. 2018. 104: 581-4
6. McGirt MJ, Rossi V, Peters D, Dyer H, Coric D, Asher AL. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting: Analysis of 2000 consecutive cases. Neurosurgery. 2020. 86: E310-5
7. Monk SH, Hani U, Pfortmiller D, Smith MD, Kim PK, Bohl MA. Anterior cervical discectomy and fusion in the ambulatory surgery center versus inpatient setting: One-year cost-utility analysis. Spine (Phila Pa 1976). 2023. 48: 155-63
8. Rossi V, Asher A, Peters D, Zuckerman SL, Smith M, Henegar M. Outpatient anterior cervical discectomy and fusion in the ambulatory surgery center setting: Safety assessment for the Medicare population. J Neurosurg Spine. 2019. p. 1-6
9. Safaee MM, Chang D, Hillman JM, Shah SS, Wadhwa H, Ames CP. Cost analysis of outpatient anterior cervical discectomy and fusion at an academic medical center without dedicated ambulatory surgery centers. World Neurosurg. 2021. 146: e940-6
10. Vaishnav A, Hill P, McAnany S, Gang CH, Qureshi S. Safety of 2-level anterior cervical discectomy and fusion (ACDF) performed in an ambulatory surgery setting with same-day discharge. Clin Spine Surg. 2019. 32: E153-9