- Neurosurgery Unit, IRCCS Istituto delle Scienze Neurologiche di Bologna, Bologna, Italy,
- Department of Biomedical and Neuromotor Sciences (DIBINEM), Alma Mater Studiorum University of Bologna, Bologna, Italy.
Correspondence Address:
Emanuele La Corte
Neurosurgery Unit, IRCCS Istituto delle Scienze Neurologiche di Bologna, Bologna, Italy,
DOI:10.25259/SNI_765_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Emanuele La Corte1,2, Clarissa A. E. Gelmi1,2, Nicola Acciarri1. Carpal tunnel syndrome caused by the entrapment of a bifid Lanz IIIA Type anatomical variant of median nerve: A case report and systematic literature review. 03-Feb-2021;12:37
How to cite this URL: Emanuele La Corte1,2, Clarissa A. E. Gelmi1,2, Nicola Acciarri1. Carpal tunnel syndrome caused by the entrapment of a bifid Lanz IIIA Type anatomical variant of median nerve: A case report and systematic literature review. 03-Feb-2021;12:37. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10561
Abstract
Background: Carpal tunnel syndrome (CTS) is the most common entrapment peripheral neuropathy. Median nerve may present several anatomical variations such as a high division or bifid median nerve (BMN). A thorough knowledge of the normal anatomy and variations of the median nerve at the wrist are fundamental to reduce complications during carpal tunnel release.
Case Description: A 63-year-old man with CTS underwent preoperative ultrasound that showed the entrapment of the median nerve and disclosed a BMN Lanz IIIA Type anatomical variation at the carpal tunnel. During the surgery, the anatomical variant of a BMN at the wrist has been visualized. Both nervous rami entirely occupied the carpal canal and this may have predisposed to the development of the entrapment syndrome. Nor persistent median artery, or other associated abnormalities, have been identified. At the 6 months follow-up control, the patient referred a good surgical recovery with complete resolution of the preoperative symptoms of the median nerve entrapment.
Conclusion: A rare case of Lanz IIIA BMN Type at the wrist has been encountered in a patient with a CTS and a systematic review and practical considerations have been presented with the aim of raising awareness to the neurosurgical community of a such rare variant that could be encountered during carpal tunnel release procedures. CTS may be caused by the entrapment of a BMN Lanz IIIA Type anatomical variant of median nerve. Preoperative US would help to identify such patients to reduce risk of iatrogenic injuries.
Keywords: Anatomy, Bifid median nerve, Carpal tunnel syndrome, Median nerve, Peripheral nervous system diseases
INTRODUCTION
Carpal tunnel syndrome (CTS) is the most common entrapment peripheral neuropathy with a prevalence of 6%.[
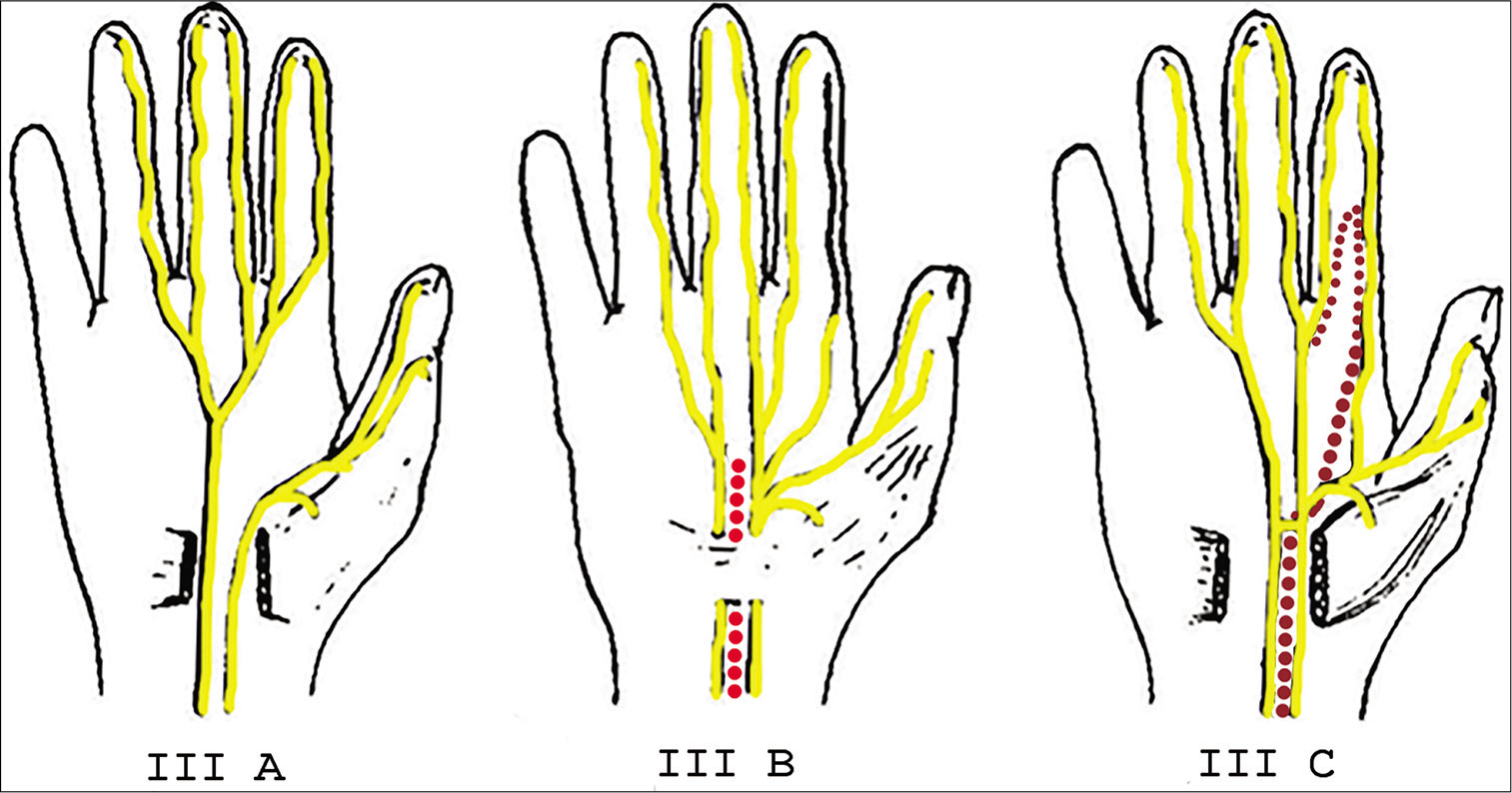
Group 0: Extraligamentous thenar branch (standard anatomy). Group I: Thenar branch variations in relation to the transverse carpal ligament (TCL). Group II: Distal accessory thenar branches. Group III: High division of the median nerve. Group IV: Proximal accessory thenar branches.
In 2009, Al-Qattan et al. further subclassified the high division of the median nerve, differentiating six subgroups, according to the associated anomalies:[
Subgroup I: Bifid median nerve (BMN) without persistent median vessels or abnormalities Subgroup II: BMN with persistent median vessels without any pathology Subgroup III: BMN with persistent median vessels with aneurysm, thrombosis, or arteriovenous malformation Subgroup IV: BMN with each division passing separately in the carpal tunnel Subgroup V: BMN with aberrant muscle between its two divisions Subgroup VI: BMN with aberrant branches.
A thorough knowledge of the normal anatomy and variations of the median nerve at the wrist is fundamental to reduce complications during carpal tunnel release. In the present paper, we present a rare case of BMN, or Lanz IIIA Type, at the wrist in a patient with CTS and an associated systematic review to give awareness to the neurosurgical community of such scenario.
MATERIALS AND METHODS
The present case has been reported according to the international CARE guidelines.[
Literature review search strategy
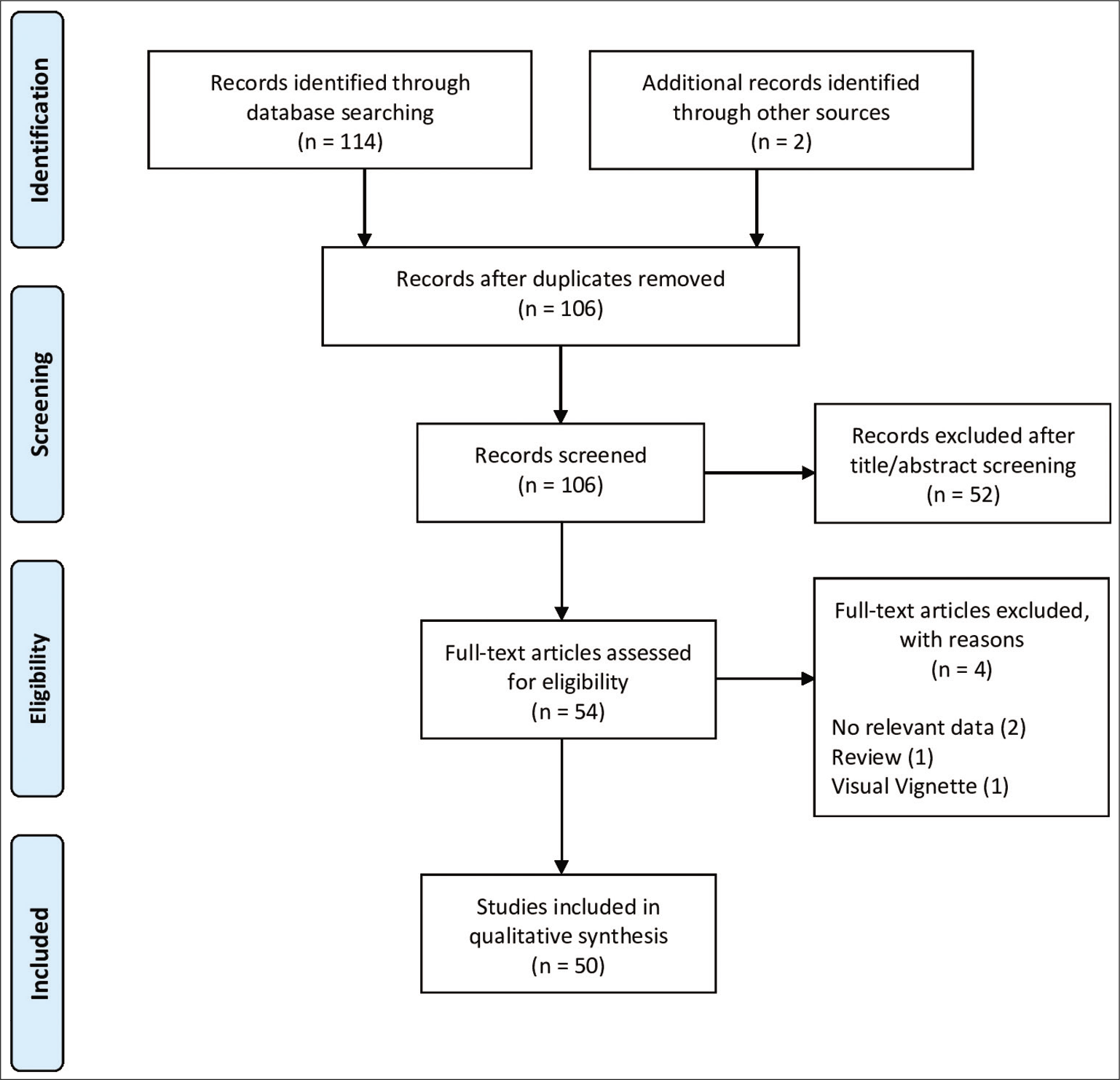
A systematic literature review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement guidelines, limited to the English language.[
Selection criteria
Only studies dealing with the presence of BMN within or proximal to the carpal tunnel were included, also considering anatomical and radiological researches. The articles without relevant data, review, visual vignette, or sonographic studies with a cohort already screened for only patients with BMN were excluded. Studies involving magnetic resonance imaging (MRI) and ultrasonography (US) as presurgical diagnostic test were included only if sufficient individual data on the prevalence of BMN and its clinical correlation could be obtained to meet the inclusion criteria.
Data extraction
Data from the included studies were extracted, organized, and analyzed using Microsoft Excel 2019 (Microsoft Corp., Redmond, WA, USA). Collected variables included first author, publication year, number of the total wrists considered, and number of those which presented BMN and other associated anatomical features (i.e., persistent median artery [PMA]/vein, anomalous tendon, neural loop, and aberrant muscle), Lanz and Al-Qattan classifications, presence of an associated CTS, and its presumed etiology.[
CASE REPORT
A 63-year-old man complained with a 6-month history of nocturnal paresthesia and intermittent burning pain of the right arm and hand, along with the distribution of the right median nerve. His clinical history was characterized by diabetes mellitus Type 2 and hypertension. He worked as a chef and his previous surgical history was negative. A first nonsurgical approach has been proposed to the patient but without beneficial response. The patient furtherly complained a worsening of his symptoms resulting in progressive motor and sensory deficits, such as loss of texture discrimination and fine motor hand skills. Electrophysiological diagnostics showed a marked alteration of the right median nerve, with an increased distal motor latency, reduction of nerve conduction velocity, and the presence of sporadic fibrillations to the abductor pollicis brevis muscle.
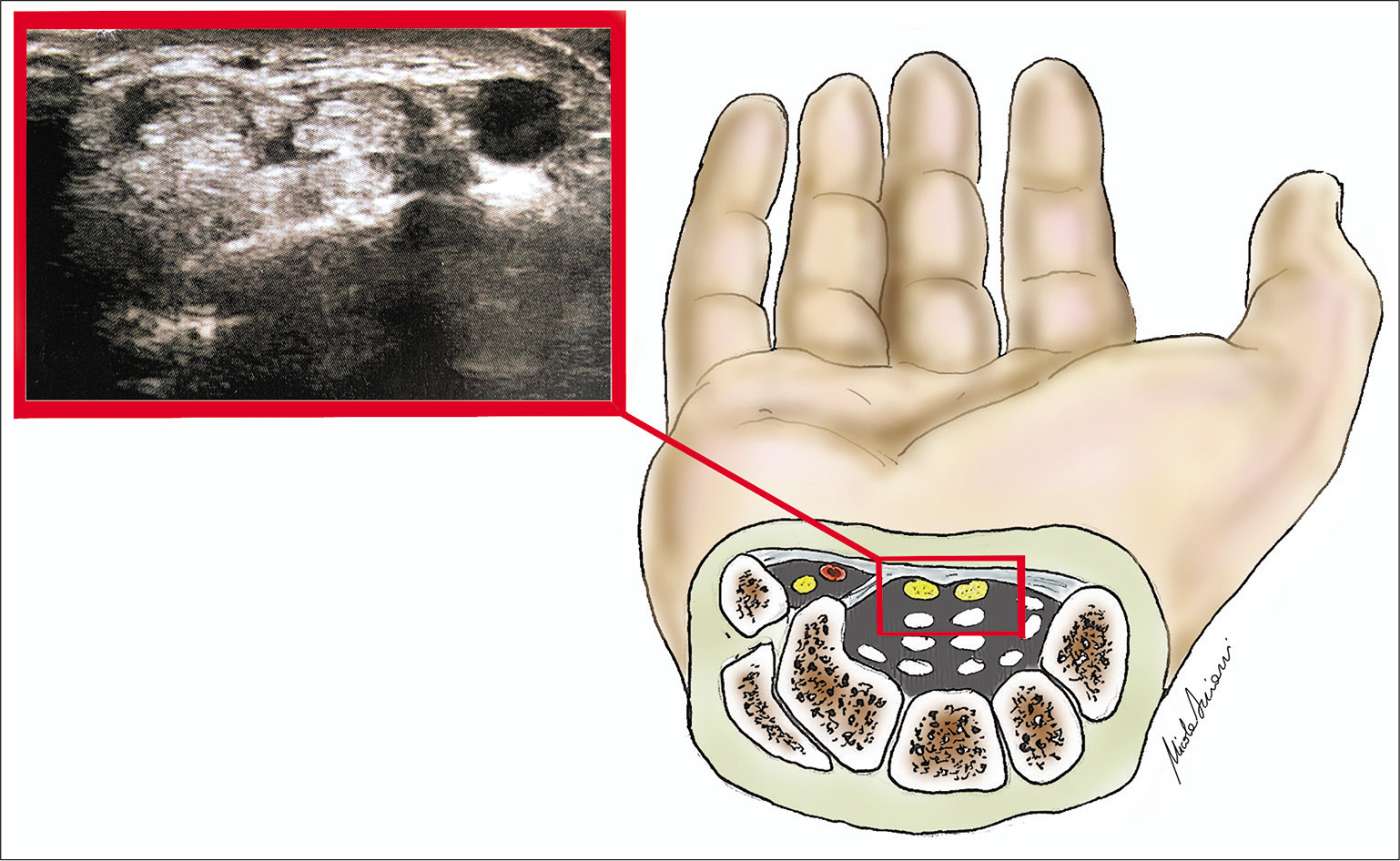
The patient came to our office and general physical examination was normal. Neurological examination disclosed an impairment of his right hand movements, specifically motor and sensory deficit attributable to the right median nerve, with mild thenar atrophy, positive Tinel’s sign and Phalen’s test. An open surgical decompression of the carpal tunnel was proposed. Preoperative ultrasound confirmed the entrapment of median nerve and disclosed a BMN anatomical variation Lanz IIIA Type, subgroup I, at the carpal tunnel [
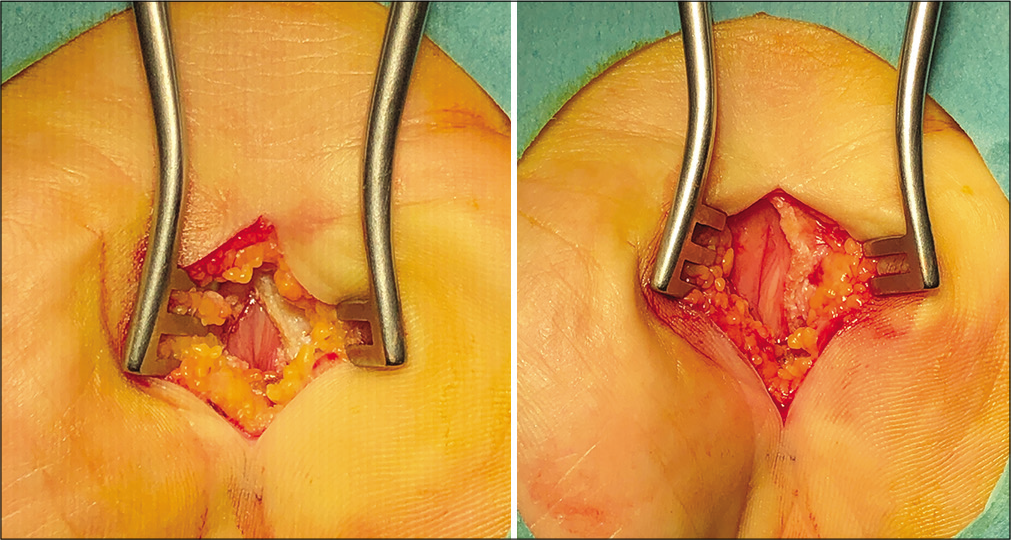
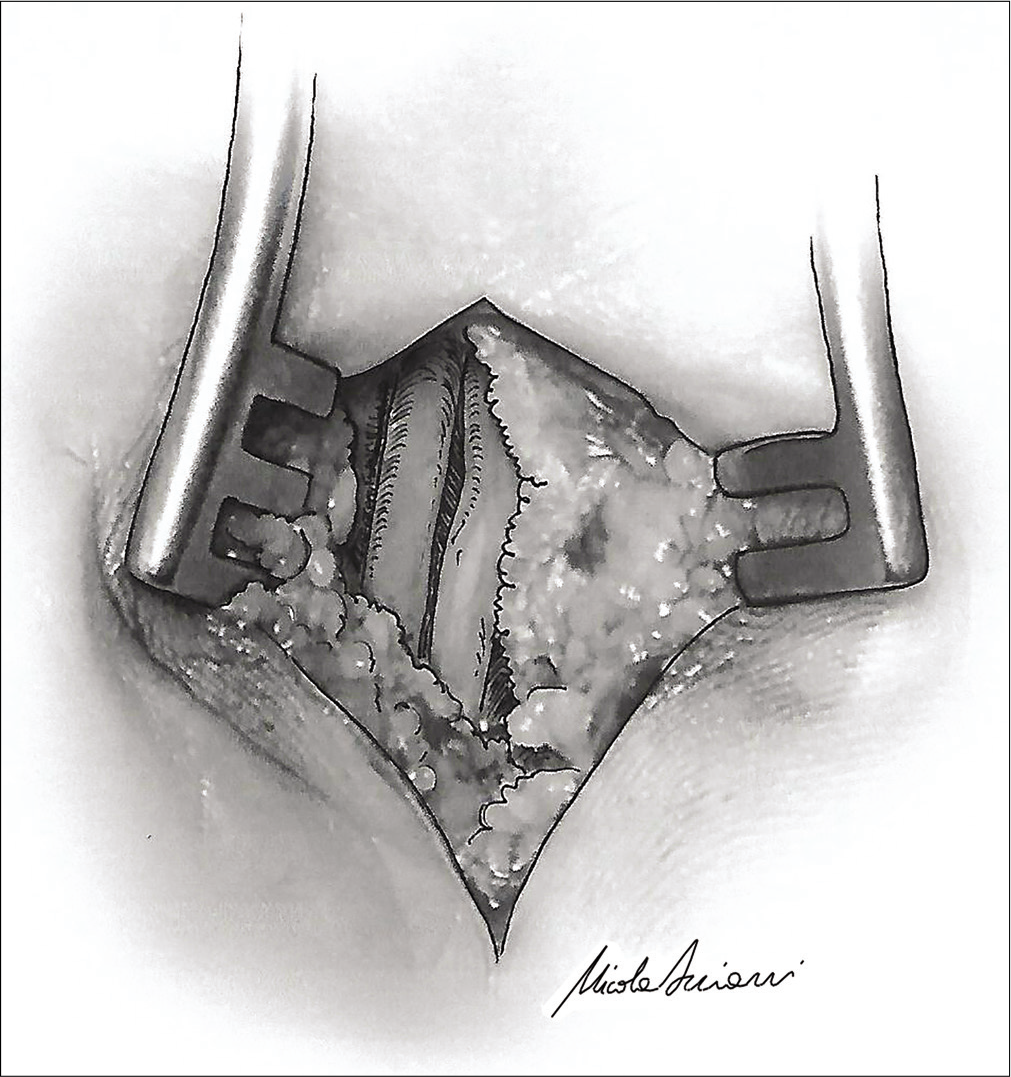
The anatomical landmarks were recognized, and, under local anesthesia, a 4 cm skin incision has been made at the intersection of the proximal extension of the radial side of the ring finger with the Kaplan’s cardinal line. The subcutaneous tissue with its fat component was incised until the exposure of the TCL. Afterwards, TCL has been incised and, underneath, the anatomical variant of a BMN at the wrist has been visualized [
The BMN macroscopically appeared as pale nerves indicating a chronic suffering. Both nervous rami entirely occupied the carpal canal and this may have predisposed to the development of the entrapment syndrome. No PMA nor other associated abnormalities have been identified. The TCL has been completely sectioned and BMN completely released [
Closure of subcutaneous and skin layers have done in a standard fashion. At the 6 months follow-up control, the patient referred a good surgical recovery with complete resolution of the preoperative symptoms of the median nerve entrapment.
RESULTS
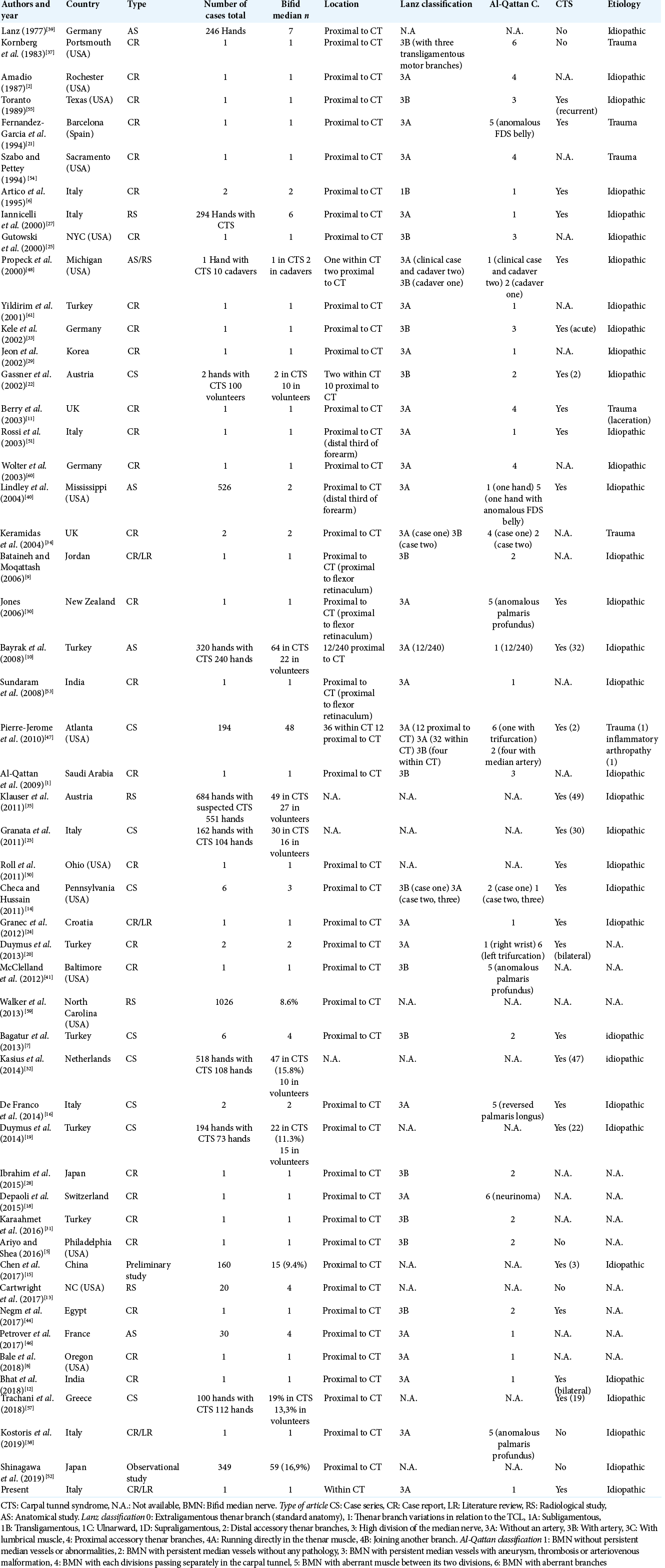
The results of the systematic literature review are summarized in the [
Afterward, Amadio reported a prevalence of 3.3% in his anatomical series and described one case of a BMN with two separate compartments within the carpal tunnel. Moreover, he stated that these branches can also distally join together, or they may have a communicating bridge.[
In the surgical literature, different authors tried to establish a correlation between the presence of BMN and the development of CTS. Iannicelli et al. reported six patients with BMN in a population of 294 with CTS, underlying the importance of using US for recognizing such anatomical variations.[
DISCUSSION
A rare case of Lanz IIIA BMN Type at the wrist has been encountered in a patient with a CTS and systematic review and practical considerations have been presented with the aim of raising awareness to the neurosurgical community of such scenario that could be encountered during CTR procedures.
The median nerve originates from the spinal roots of the brachial plexus at the level of C5–T1, bringing both motor and sensory fibers. At the level of the wrist, it is the only nervous structure to run through the carpal tunnel, deep to the TCL, then it divides into medial and lateral branches. In most individuals, the median nerve is observed as a singular nerve structure proximal to and within the carpal tunnel,[
At present, surgeons frequently rely only on clinical examination and nerve conduction studies to diagnose CTS, but they may require further tools to preferentially choose the tailored surgical approach in each patient. The use of both MRI and US to identify median nerve anomalies has been also reported.[
MRI with standard morphological sequences can be used to determine many peripheral nerve disorders; in particular, for the patients with CTS, it can reveal morphological changes, such as enlarged median nerve, nerve flattening, increased signal intensity of the nerve, and flexor retinaculum bowing.[
However, the sensitivity and specificity of conventional morphological MRI sequences are low.[
US at high frequencies easily recognizes the nerves as fascicular hypoechoic structures and also detects their corresponding relationship with vessels, such as the PMA. Its use as an adjunctive tool to study the cross-sectional area of the median nerve at the carpal tunnel is also appropriate to diagnose and grade the CTS. Some studies have expressed 99% of sensitivity and 100% of specificity for US to identify CTS with the additional advantage over the neurophysiological studies by showing the anatomy of the canal and its contents, as both BMN and PMA, that are common anatomical variants often associated with other median nerve anomalies.[
Furthermore, the use of diffusion tensor imaging (DTI) has been considered for the efficacy in the diagnosis and management of CTS, resulting to be an important imaging technique which enables visualization and characterization of the median nerve, although the quality of images depends on field homogeneity, coil, as well as the gradient systems used, making it technically challenging.[
CTR surgery can be currently performed either with the endoscopic approach or with the conventional open approach, which might be recommended in those cases with the presence of BMN, or other structural abnormalities, to allow a proper view of the corresponding anatomical structures, preferring the access from the ulnar side to be able to cut under clear vision throughout the procedure.[
Despite a significant correlation between the presence of BMN and the pathogenesis of CTS has not been ascertained in the literature, however, when it is present, the risk of developing the compression of median nerve at the carpal tunnel increases, also because it is chaperoned by PMA in almost half of the reported cases.
CONCLUSION
CTS may be caused by the entrapment of a BMN Lanz IIIA Type anatomical variant of median nerve. Preoperative US would help to identify those patients presenting with anatomical variants at increased risk of iatrogenic injuries to better plan the surgery. Therefore, US use should be encouraged as pre-operative routine work-up in CTR surgery.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Qattan MM, Al-Zahrani K, Al-Omawi M. The bifid median nerve re-visited. J Hand Surg Eur Vol. 2009. 34: 212-4
2. Amadio PC. Anatomic variations of the median nerve within the carpal tunnel. Clin Anat. 1988. 1: 23-31
3. Amadio PC. Bifid median nerve with a double compartment within the transverse carpal canal. J Hand Surg Am. 1987. 12: 366-8
4. Andreisek G, Crook DW, Burg D, Marincek B, Weishaupt D. Peripheral neuropathies of the median, radial, and ulnar nerves: MR imaging features. Radiographics. 2006. 26: 1267-87
5. Ariyo O, Shea J. Bilateral triad of persistent median artery, a bifid median nerve and high origin of its palmar cutaneous branch: A case report and clinical implications. Int J Morphol. 2016. 34: 997-1001
6. Artico M, Cervoni L, Stevanato G, Andrea VD, Nucci F. Bifid median nerve: Report of two cases. Acta Neurochir (Wien). 1995. 136: 160-2
7. Bagatur AE, Yalcinkaya M, Atca AO. Bifid median nerve causing carpal tunnel syndrome: MRI and surgical correlation. Orthopedics. 2013. 36: 451-7
8. Bale L, Brandt N, Enos N. An unusual digital neural loop in a cadaver with bilateral high branching median nerves-case report. Rom J Morphol Embryol. 2018. 59: 293-6
9. Bataineh ZM, Moqattash ST. A complex variation in the superficial palmar arch. Folia Morphol (Warsz). 2006. 65: 406-9
10. Bayrak IK, Bayrak AO, Kale M, Turker H, Diren B. Bifid median nerve in patients with carpal tunnel syndrome. J Ultrasound Med. 2008. 27: 1129-36
11. Berry MG, Vijh V, Percival NJ. Bifid median nerve: Anatomical variant at the carpal tunnel. Scand J Plast Reconstr Surg Hand Surg. 2003. 37: 58-60
12. Bhat AK, Acharya AM, Kurup JK, Chakraborti A. Bilateral bifid median nerve with bilateral carpal tunnel syndrome: An atypical presentation, a rare cause and a familiar disease. J Hand Surg Asian Pac Vol. 2018. 23: 274-7
13. Cartwright MS, Baute V, Caress JB, Walker FO. Ultrahigh-frequency ultrasound of fascicles in the median nerve at the wrist. Muscle Nerve. 2017. 56: 819-22
14. Checa A, Hussain H. Sonographic assessment of a bifid median nerve and median artery in carpal tunnel syndrome. J Rheumatol. 2011. 38: 1694-6
15. Chen L, Chen J, Hu B, Jiang LX. Sonographic findings of the bifid median nerve and persistent median artery in carpal tunnel: A preliminary study in Chinese individuals. Clinics (Sao Paulo). 2017. 72: 358-62
16. de Franco P, Erra C, Granata G, Coraci D, Padua R, Padua L. Sonographic diagnosis of anatomical variations associated with carpal tunnel syndrome. J Clin Ultrasound. 2014. 42: 371-4
17. de Krom MC, Knipschild PG, Kester AD, Thijs CT, Boekkooi PF, Spaans F. Carpal tunnel syndrome: Prevalence in the general population. J Clin Epidemiol. 1992. 45: 373-6
18. Depaoli R, Coscia DR, Alessandrino F. In-continuity neuroma of the median nerve after surgical release for carpal tunnel syndrome: Case report. J Ultrasound. 2015. 18: 83-5
19. Duymuş M, Orman G, Özben S, Hüseyinoğlu N, Ulaşli AM. The association between bifid median nerve and carpal tunnel syndrome: Is it really a risk factor?. Arch Rheumatol. 2014. 29: 105-9
20. Duymus M, Yilmaz O, Ulasli AM, Asal N, Kosar U. Coexistence of trifid and bifid median nerve in a patient with bilateral carpal tunnel syndrome. Turk Neurosurg. 2013. 23: 685-7
21. Fernandez-Garcia S, Pi-Folguera J, Estallo-Matino F. Bifid median nerve compression due to a musculotendinous anomaly of FDS to the middle finger. J Hand Surg Br. 1994. 19: 616-7
22. Gassner EM, Schocke M, Peer S, Schwabegger A, Jaschke W, Bodner G. Persistent median artery in the carpal tunnel: Color Doppler ultrasonographic findings. J Ultrasound Med. 2002. 21: 455-61
23. Granata G, Caliandro P, Pazzaglia C, Minciotti I, Russo G, Martinoli C. Prevalence of bifid median nerve at wrist assessed through ultrasound. Neurol Sci. 2011. 32: 615-8
24. Granec D, Bićanić G, Borić I, Delimar D. Bifid median nerve in a patient with carpal tunnel syndrome-correlation of clinical, diagnostic and intraoperative findings: Case report and review of the literature. Acta Clin Croat. 2012. 51: 667-71
25. Gutowski KA, Olivier WA, Mehrara BJ, Friedman DW. Arteriovenous malformation of a persistent median artery with a bifurcated median nerve. Plast Reconstr Surg. 2000. 106: 1336-9
26. Henry BM, Zwinczewska H, Roy J, Vikse J, Ramakrishnan PK, Walocha JA. The prevalence of anatomical variations of the median nerve in the carpal tunnel: A systematic review and meta-analysis. PLoS One. 2015. 10: e0136477
27. Iannicelli E, Chianta GA, Salvini V, Almberger M, Monacelli G, Passariello R. Evaluation of bifid median nerve with sonography and MR imaging. J Ultrasound Med. 2000. 19: 481-5
28. Ibrahim M, Hattori Y, Doi K, Sakamoto S, Madura T. Bifid median nerve-a case report. Hand Surg. 2015. 20: 482-3
29. Jeon IH, Kim PT, Park IH, Park BC, Ihn JC. High bifurcation of median nerve at the wrist causing common digital nerve injury in endoscopic carpal tunnel release. J Hand Surg Br. 2002. 27: 580-2
30. Jones DP. Bilateral palmaris profundus in association with bifid median nerve as a cause of failed carpal tunnel release. J Hand Surg Am. 2006. 31: 741-3
31. Karaahmet OZ, Umay E, Gurcay E, Cakci A. Bifid median nerve and persistent median artery with ultrasound evaluation. J Clin Neuromuscul Dis. 2016. 18: 101-2
32. Kasius KM, Claes F, Meulstee J, Verhagen WI. Bifid median nerve in carpal tunnel syndrome: Do we need to know?. Muscle Nerve. 2014. 50: 835-43
33. Kele H, Verheggen R, Reimers CD. Carpal tunnel syndrome caused by thrombosis of the median artery: The importance of high-resolution ultrasonography for diagnosis. Case report. J Neurosurg. 2002. 97: 471-3
34. Keramidas EG, Rodopoulou S, Miller G. Bifid median nerve in trauma patients: How rare is it? Two case reports and review of the literature. Eur J Trauma. 2004. 30: 323-6
35. Klauser AS, Halpern EJ, Faschingbauer R, Guerra F, Martinoli C, Gabl MF. Bifid median nerve in carpal tunnel syndrome: Assessment with US cross-sectional area measurement. Radiology. 2011. 259: 808-15
36. Koh SH, Kwon BC, Park C, Hwang SY, Lee JW, Kim SS. A comparison of the performance of anatomical MRI and DTI in diagnosing carpal tunnel syndrome. Eur J Radiol. 2014. 83: 2065-73
37. Kornberg M, Aulicino PL, DuPuy TE. Bifid median nerve with three thenar branches-case report. J Hand Surg Am. 1983. 8: 583-4
38. Kostoris F, Bassini S, Longo E, Murena L. Carpal tunnel syndrome associated with bifid median nerve and palmaris profundus-case report and literature review. J Hand Surg Asian Pac Vol. 2019. 24: 238-42
39. Lanz U. Anatomical variations of the median nerve in the carpal tunnel. J Hand Surg Am. 1977. 2: 44-53
40. Lindley SG, Kleinert JM. Prevalence of anatomic variations encountered in elective carpal tunnel release. J Hand Surg Am. 2003. 28: 849-55
41. McClelland WB, Means KR. Palmaris profundus tendon prohibiting endoscopic carpal tunnel release: Case report. J Hand Surg Am. 2012. 37: 695-8
42. Mitchell R, Chesney A, Seal S, Mcknight L, Thoma A. Anatomical variations of the carpal tunnel structures. Can J Plast Surg. 2009. 17: e3-7
43. Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009. 151: 264-9
44. Negm AA, Nagm A, Altamimyh H, Ghanem M. Ultrasonography of a bifid median nerve causing carpal tunnel syndrome: MSUS or MRI, which is better?. Rheumatol Int. 2017. 37: 1591-2
45. Padua L, Coraci D, Erra C, Pazzaglia C, Paolasso I, Loreti C. Carpal tunnel syndrome: Clinical features, diagnosis, and management. Lancet Neurol. 2016. 15: 1273-84
46. Petrover D, Bellity J, Vigan M, Nizard R, Hakime A. Ultrasound imaging of the thenar motor branch of the median nerve: A cadaveric study. Eur Radiol. 2017. 27: 4883-8
47. Pierre-Jerome C, Smitson RD, Shah RK, Moncayo V, Abdelnoor M, Terk MR. MRI of the median nerve and median artery in the carpal tunnel: Prevalence of their anatomical variations and clinical significance. Surg Radiol Anat. 2010. 32: 315-22
48. Propeck T, Quinn TJ, Jacobson JA, Paulino AF, Habra G, Darian VB. Sonography and MR imaging of bifid median nerve with anatomic and histologic correlation. Am J Roentgenol. 2000. 175: 1721-5
49. Riley DS, Barber MS, Kienle GS, Aronson JK, von SchoenAngerer T, Tugwell P. CARE guidelines for case reports: Explanation and elaboration document. J Clin Epidemiol. 2017. 89: 218-35
50. Roll SC, Evans KD. Sonographic representation of bifid median nerve and persistent median artery. J Diagn Med Sonogr. 2011. 27: 89-94
51. Rossi C, Cellocco P, Costanzo G. Bifid median nerve as a determinant of carpal tunnel syndrome recurrence after endoscopic procedures. A case report. J Orthop Traumatol. 2003. 4: 92-4
52. Shinagawa S, Tajika T, Oya N, Endo F, Kuboi T, Hamano N. Prevalence of bifid median nerve and the cross-sectional area as assessed by ultrasonography in healthy japanese subjects. J Hand Surg Glob Online. 2019. 1: 74-8
53. Sundaram SM, Kumar MS, Sethupathi BB, Nayak SR, Krishnamurthy A. Split median nerve with variation in its common digital branch-a case report. Neuroanatomy. 2008. 7: 15-6
54. Szabo RM, Pettey J. Bilateral median nerve bifurcation with an accessory compartment within the carpal tunnel. J Hand Surg Am. 1994. 19: 22-3
55. Toranto IR. Aneurysm of the median artery causing recurrent carpal tunnel syndrome and anatomic review. Plast Reconstr Surg. 1989. 84: 510-2
56. Tountas CP, MacDonald CJ, Meyerhoff JD, Bihrle DM. Carpal tunnel syndrome. A review of 507 patients. Minn Med. 1983. 66: 479-82
57. Trachani E, Rigopoulou A, Veltsista D, Gavanozi E, Chrysanthopoulou A, Chroni E. Occurrence of bifid median nerve in healthy and carpal tunnel syndrome patients. J Electromyogr Kinesiol. 2018. 39: 77-80
58. Wafaie AM, Afifi LM, Moussa KM, Mansour AM, Abbas HM. Role of diffusion tensor imaging in carpal tunnel syndrome: A case control comparative study to electrophysiological tests and clinical assessment. Egypt J Radiol Nucl Med. 2018. 49: 1068-75
59. Walker FO, Cartwright MS, Blocker JN, Arcury TA, Suk JI, Chen H. Prevalence of bifid median nerves and persistent median arteries and their association with carpal tunnel syndrome in a sample of latino poultry processors and other manual workers. Muscle Nerve. 2013. 48: 539-44
60. Wolter TP, Kleiner U, Noah EM, Pallua N. Persistent carpal tunnel syndrome after both endoscopic and open release: A rare case of a bifid median nerve in two separate compartments. Eur J Plast Surg. 2003. 26: 102-4
61. Yildirim S, Akan M, Aydoǧdu E. Bifid median nerve. Plast Reconstr Surg. 2001. 108: 584-5