- Department of Neurosurgery, Ichinomiya Neurosurgical Hospital, Hita, Japan.
- Department of Neurosurgery, Uchikado Neuro-Spine Clinic, Fukuoka, Japan.
- Department of Neurosurgery, Social Insurance Tagawa Hospital, Fukuoka, Japan.
- Department of Neurosurgery, Yame General Hospital, Yame, Japan.
Correspondence Address:
Yoshinori Hisamitsu, Department of Neurosurgery, Ichinomiya Neurosurgical Hospital, Hita, Japan.
DOI:10.25259/SNI_967_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yoshinori Hisamitsu1, Hisaaki Uchikado2, Takehiro Makizono3, Tomoya Miyagi1, Takahiro Miyahara4. Case of lumbar ligamentum flavum hematoma with epidural hematoma resulting in cauda equina compression. 25-Nov-2022;13:550
How to cite this URL: Yoshinori Hisamitsu1, Hisaaki Uchikado2, Takehiro Makizono3, Tomoya Miyagi1, Takahiro Miyahara4. Case of lumbar ligamentum flavum hematoma with epidural hematoma resulting in cauda equina compression. 25-Nov-2022;13:550. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12024
Abstract
Background: Lumbar ligamentum flavum hematomas (LFHs) are rare. However, when they occur and contribute to epidural cauda equina compression, timely surgical intervention is frequently warranted.
Case Description: A 69-year-old female presented with the left lower extremity sciatica and gait disturbance of 2 weeks’ duration that ultimately evolved into a paraparesis/cauda equina syndrome. When the lumbar MRI revealed left-sided L4-L5 epidural compression attributed to a hemorrhage into the hypertrophied ligamentum flavum (HLF), she successfully underwent a bilateral fenestration/decompressive procedure. Pathologically, neovascularization and rupture of the ventral layers of the degenerated and thickened HLF contributed to the LFH.
Conclusion: Arterial neovascularization (i.e., arterial feeding vessels from paramuscular/prelaminar lumbar branches) contributed to a left-sided L4-L5 LFH that resulted in epidural cauda equina compression in a 69-year-old female. Following surgical focal fenestration/decompression, the patient’s symptoms/signs resolved.
Keywords: Cauda equina syndrome, Decompressive surgery, Degenerative lumbar spine, Hypertrophied ligamentum flavum hematoma, Lumbar canal stenosis, Neovascularization, Prelaminar artery
INTRODUCTION
Lumbar ligamentum flavum hematomas (LFHs) are rare; we were only able to identify 28 such cases in the literature [
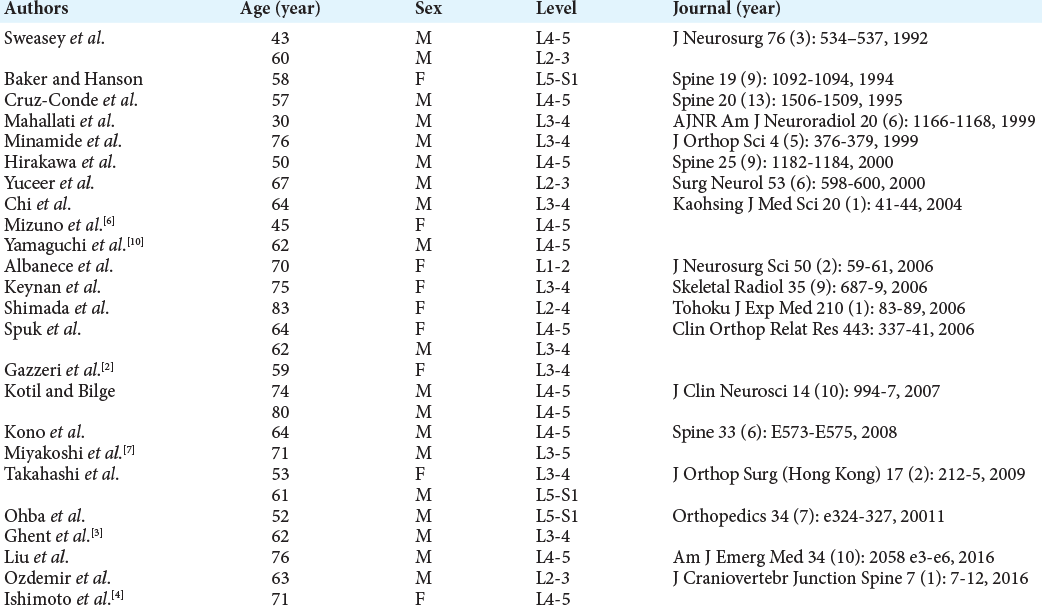
Table 1:
Reported Twenty-eight cases of lumbar ligamentum flavum hematoma.[
CASE REPORT
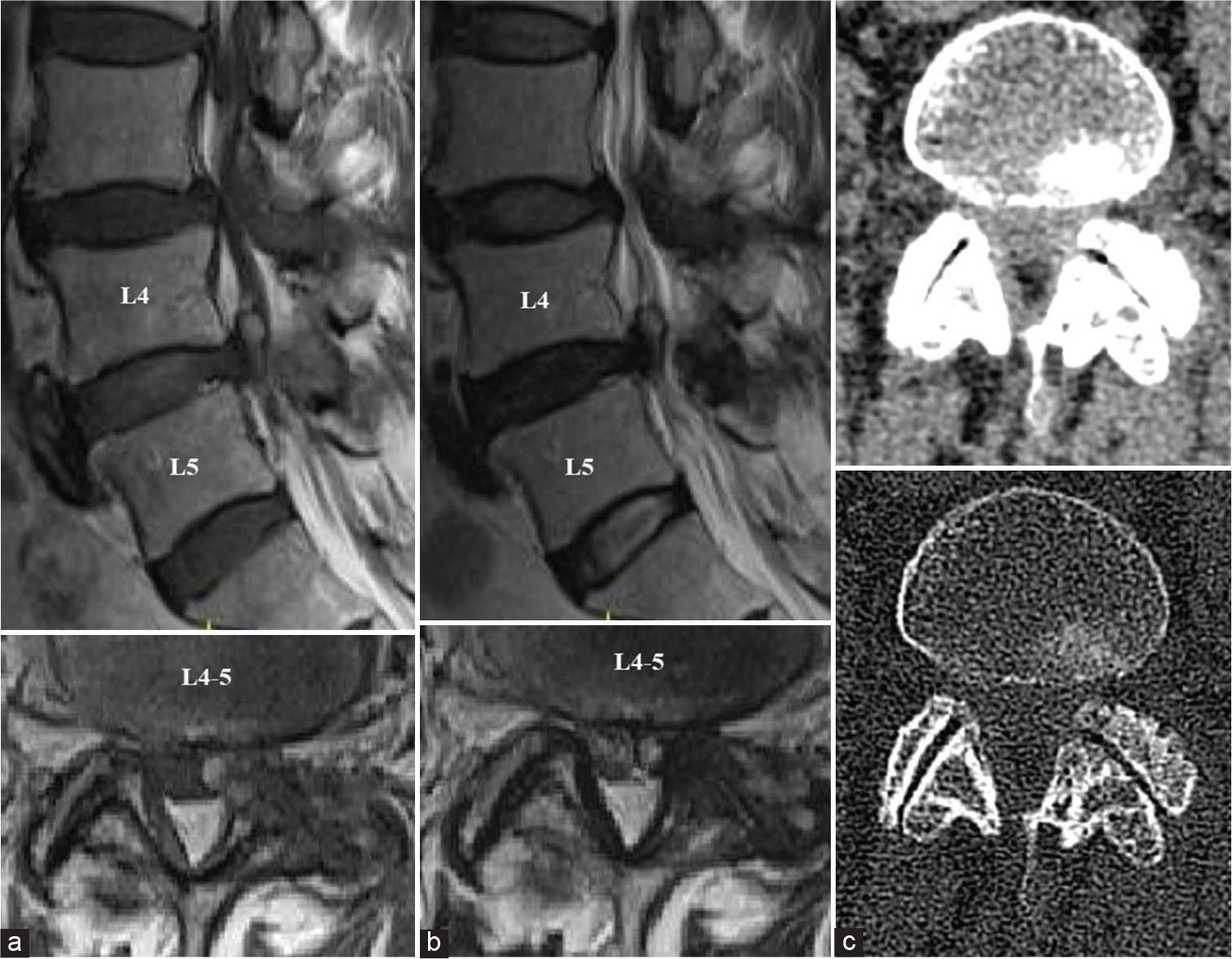
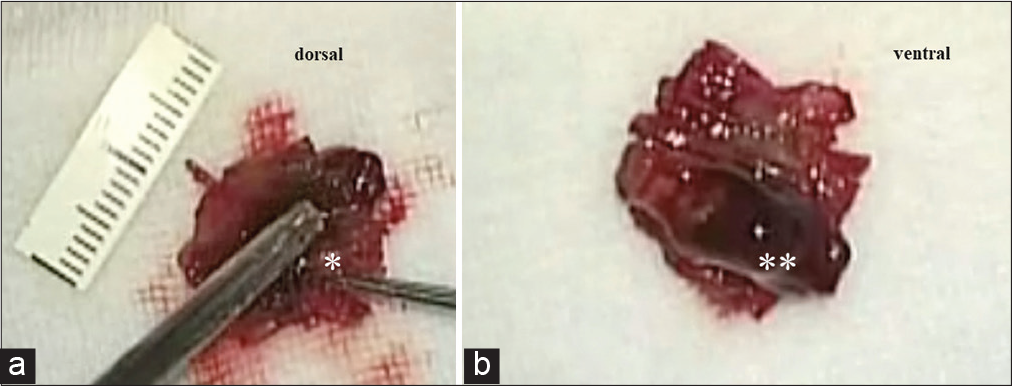
A 69-year-old female presented with 2 weeks of progressive left lower extremity sciatica and paraparesis/partial cauda equina syndrome. The lumbar MR showed a left-sided L4-L5 epidural hematoma and LFH within the left HLF [
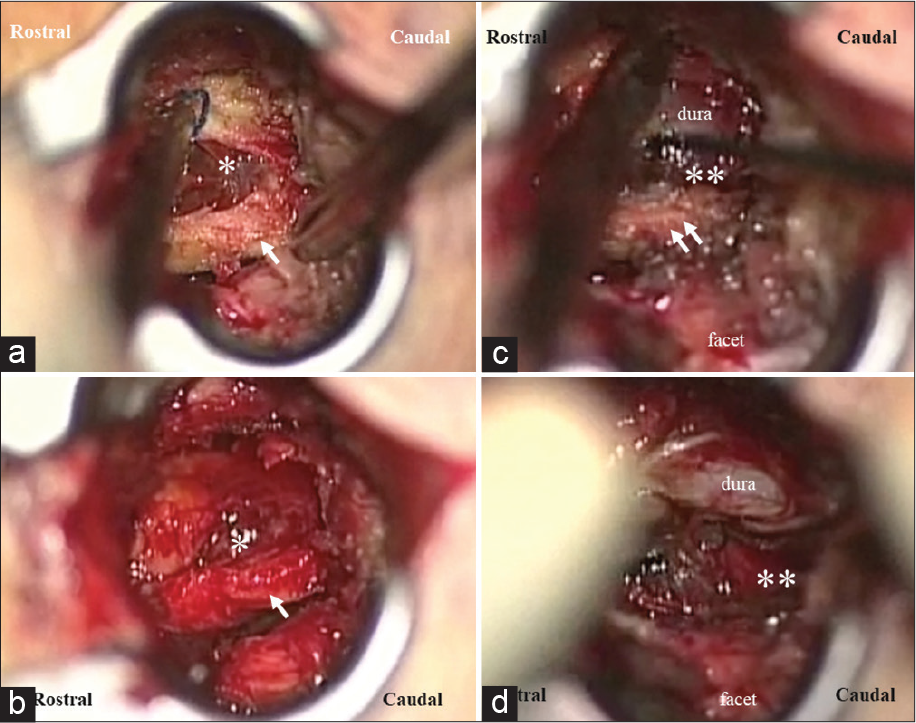
Figure 2:
Midline fenestration at L4-5 level: intraoperative findings. (a) A left-sided L4-L5 hematoma (asterisk) within hypertrophied ligamentum flavum (HLF) (arrow). (b) Hematoma (asterisk) in dorsal layer of left HLF (arrow); image after removed of the right HLF. (c) Epidural hematoma (double asterisks) on the ventral side of HLF (double arrows). (d) Resection of the left HLF revealed an epidural hematoma (double asterisks).
DISCUSSION
The histopathology of LFH has largely been attributed to ligamentum flavum degeneration with neovascularization.[
Etiology of LFH
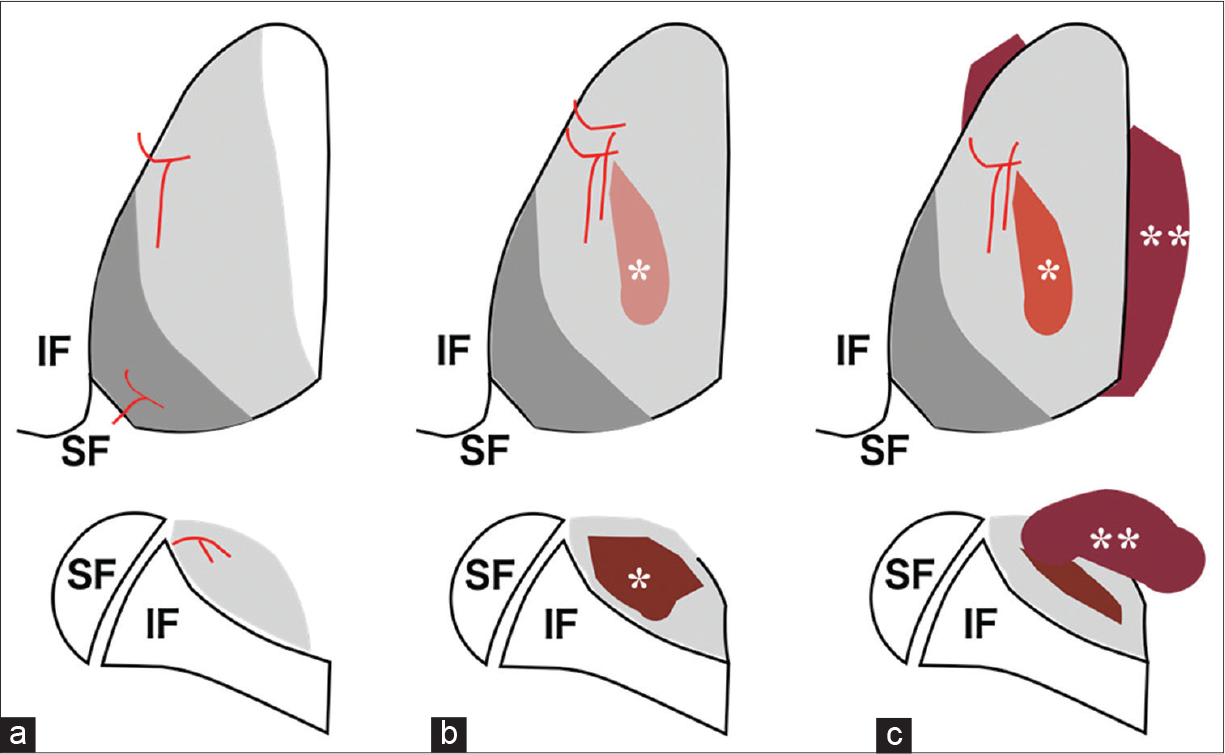
Mechanical stress and angiogenesis both contribute to the development/progression of HLF and LFH [
CONCLUSION
Hemorrhage into the lumbar left-sided HLF due to neovascularization resulted in L4-5 epidural compression that successfully resolved following a fenestration/ decompressive procedure.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ak H, Vural S. Simultaneous presence of juxtafacet cyst and ligamentum flavum hematoma. Asian J Neurosurg. 2020. 15: 184-6
2. Gazzeri R, Canova A, Fiore C, Galarza M, Neroni M, Giordano M. Acute hemorrhagic cysts of the ligamentum flavum. J Spinal Disord Tech. 2007. 20: 536-8
3. Ghent F, Ye X, Yan M, Mobbs RJ. A contrast-enhancing lumbar ligamentum flavum haematoma. BMJ Case Rep. 2014. 2014: bcr2013202521
4. Ishimoto Y, Kawakami M, Curtis E, Cooper C, Moriguchi N, Nakagawa Y. A succession of MRI scans supports the diagnosis of lumbar ligamentum flavu hematoma: A case report and review of the literature. Case Rep Orthop. 2018. 2018: 2860621
5. Kaneko T, Oshima Y, Inoue H, Iwai H, Takano Y, Inanami H. Successful treatment of lumbar ligamentum flavum hematoma using full-endoscopic system. J Spine Surg. 2018. 4: 744-9
6. Mizuno J, Nakagawa H, Inoue T, Hashizume Y. Ligamentum flavum hematoma in the lumbar spine. Case report. Neurol Med Chir (Tokyo). 2005. 45: 212-5
7. Miyakoshi N, Kasukawa Y, Ando S, Shimada Y. Two-level ligamentum flavum hematoma in the lumbar spine. Case report. Neurol Med Chir (Tokyo). 2008. 48: 179-82
8. Park JH, Im SB, Kim HK, Hwang SC, Shin DS, Shin WH. Histopathological findings of hemorrhagic ganglion cyst causing acute radicular pain: A case report. Korean J Spine. 2013. 10: 242-5
9. Thron AK, editors. Vascular Anatomy of the Spinal Cors. Radioanatomy as the Key to Diangnosis and Treatment. Switzerland: Springer International Publishing; 2016. p. 10-4
10. Yamaguchi S, Hida K, Akino M, Seki T, Yano S, Iwasaki T. Ligamentum flavum hematoma in the lumbar spine. Neurol Med Chir (Tokyo). 2005. 45: 272-6