- Department of Neurosurgery, Saiseikai Noe Hospital, Osaka, Japan
- Department of Neurosurgery, Hyogo Medical University, Nishinomiya, Japan
- Department of Neurology, Saiseikai Noe Hospital, Osaka, Japan.
Correspondence Address:
Takuto Kuwajima, Department of Neurosurgery, Saiseikai Noe Hospital, Osaka, Japan.
DOI:10.25259/SNI_455_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Takuto Kuwajima1,2, Mikiya Beppu1,2, Kazuhiko Maeda3, Yoichiro Okada3, Ryuichi Kohno3, Shinichi Yoshimura2. Cavernous sinus dural arteriovenous fistula treated with transvenous embolization through facial vein: A case report. 07-Jul-2023;14:232
How to cite this URL: Takuto Kuwajima1,2, Mikiya Beppu1,2, Kazuhiko Maeda3, Yoichiro Okada3, Ryuichi Kohno3, Shinichi Yoshimura2. Cavernous sinus dural arteriovenous fistula treated with transvenous embolization through facial vein: A case report. 07-Jul-2023;14:232. Available from: https://surgicalneurologyint.com/surgicalint-articles/12398/
Abstract
Background: Although the inferior petrosal sinus (IPS) is the most common approach route for transvenous embolization (TVE) of cavernous sinus dural arteriovenous fistulas (CSDAVFs), other routes should be chosen in cases which the IPS is occluded. We report a case in which the superior ophthalmic vein (SOV) approach through the facial vein (FV) was the first choice to achieve radical cure of a hemorrhage-onset CSDAVF.
Case Description: An 81-year-old female presented with a history of transarterial embolization (TAE) and TVE for the left CSDAVF 27 years ago. She was transported to us with a chief complaint of consciousness disturbance, and head computed tomography (CT) showed subcortical hemorrhage in the right frontal lobe. Cerebral angiography revealed CSDAVF with draining into the right SOV and right superficial middle cerebral vein (SMCV). Angiography, computed tomography venography, and contrast-enhanced magnetic resonance imaging did not show IPS, but the outflow pathways to the SOV, FV, and internal jugular vein were confirmed, so an approach through the FV was selected.
Conclusion: The FV was selected through the right femoral vein and thanks to the distal access catheter (DAC) being guided to the SOV, the microcatheter could be easily guided to the SMCV through the cavernous sinus (CS). TVE was performed, complete occlusion was confirmed. When preoperative occlusion of the IPS was confirmed, the FV was useful for the first choice of route, and the use of DAC allowed us to complete the treatment accurately and quickly.
Keywords: Cavernous sinus, Dural arteriovenous fistula, Endovascular treatment, Facial vein, Transvenous embolization
INTRODUCTION
The inferior petrosal sinus (IPS) is the preferred approach route for transvenous embolization (TVE) of cavernous sinus dural arteriovenous fistula (CSDAVF).[
CASE DESCRIPTION
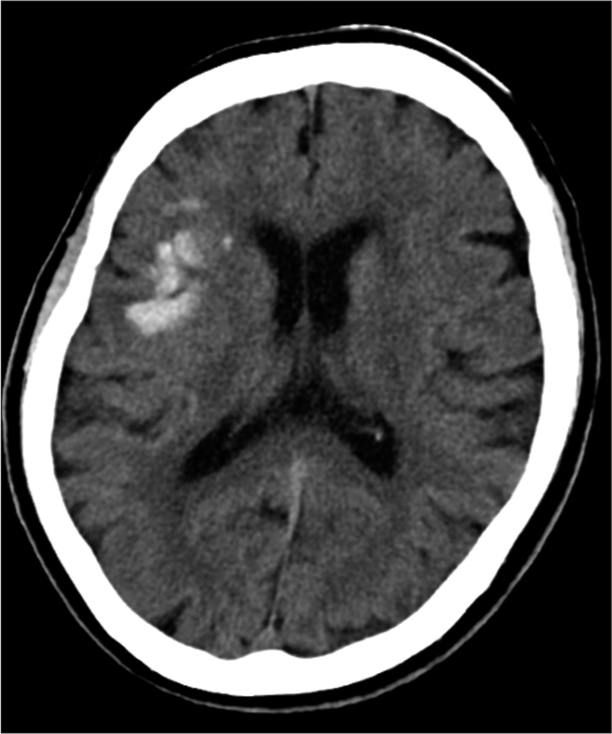
An 81-year-old female who received had undergone transarterial embolization (TAE) and TVE for the left CSDAVF 27 years ago. Postoperatively, her modified Rankin Scale (mRS) was 0. However, she had been experiencing tinnitus and ocular symptoms on the right side for several months. She was transported with consciousness disturbance (Glasgow Coma Scale: E1V1M4) and seizure, and head computed tomography (CT) [
Figure 2:
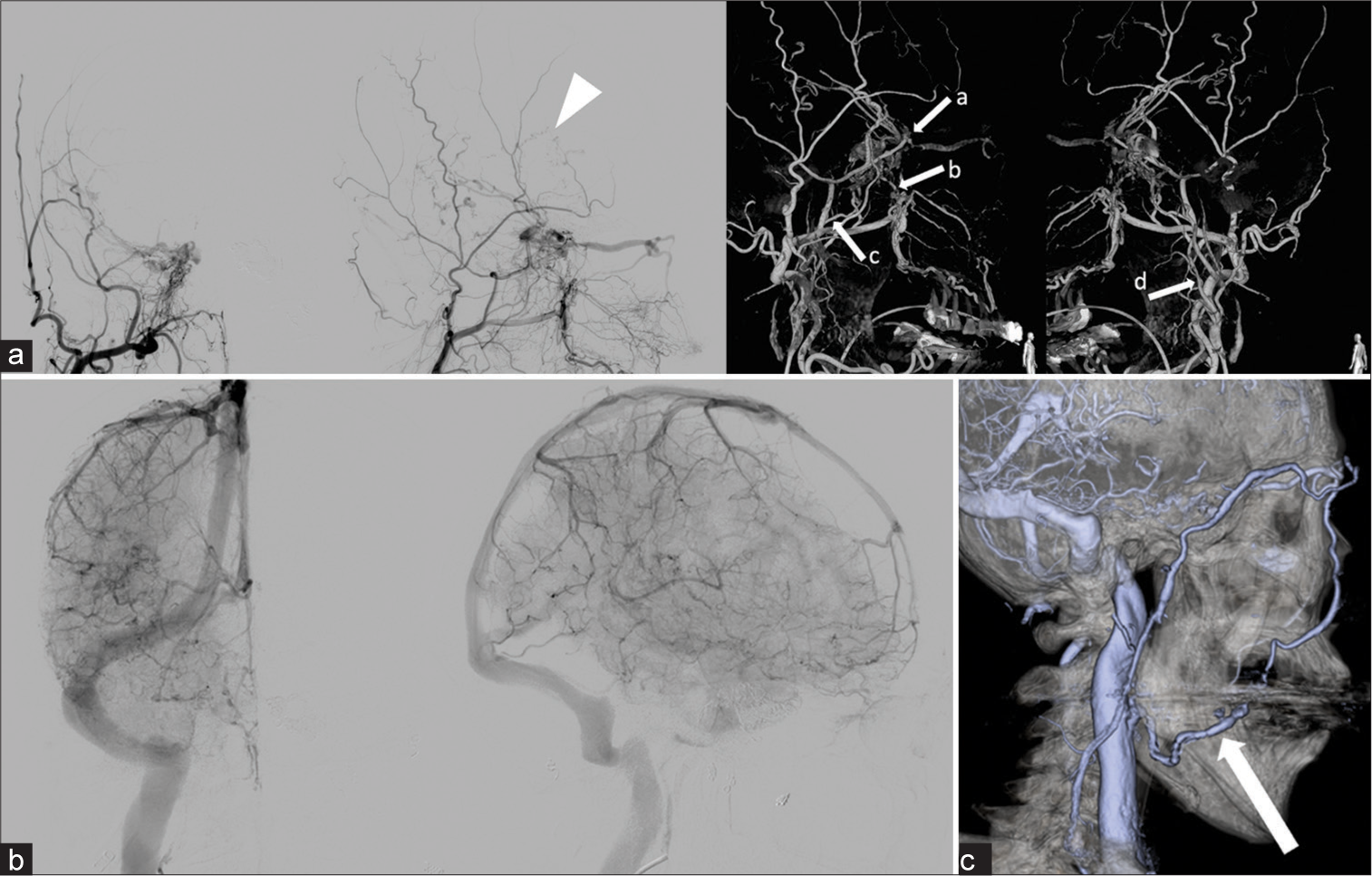
Digital subtraction angiography (DSA) and 3D-DSA (a). On external carotid angiography, the patient was diagnosed as cavernous sinus dural arteriovenous fistula, and the arrow head shows pseudo phlebitic pattern. The arrows show feeders; a: Middle meningeal artery, b: Artery of foramen rotundum, c: Accessory meningeal artery, and d: Ascending pharyngeal artery. DSA (b). On internal carotid angiography, inferior petrosal sinus was not visualized on venous phase. (c) CT venography. Inferior petrosal vein was not detected, and the arrow shows that facial vein was well visualized.
Figure 3:
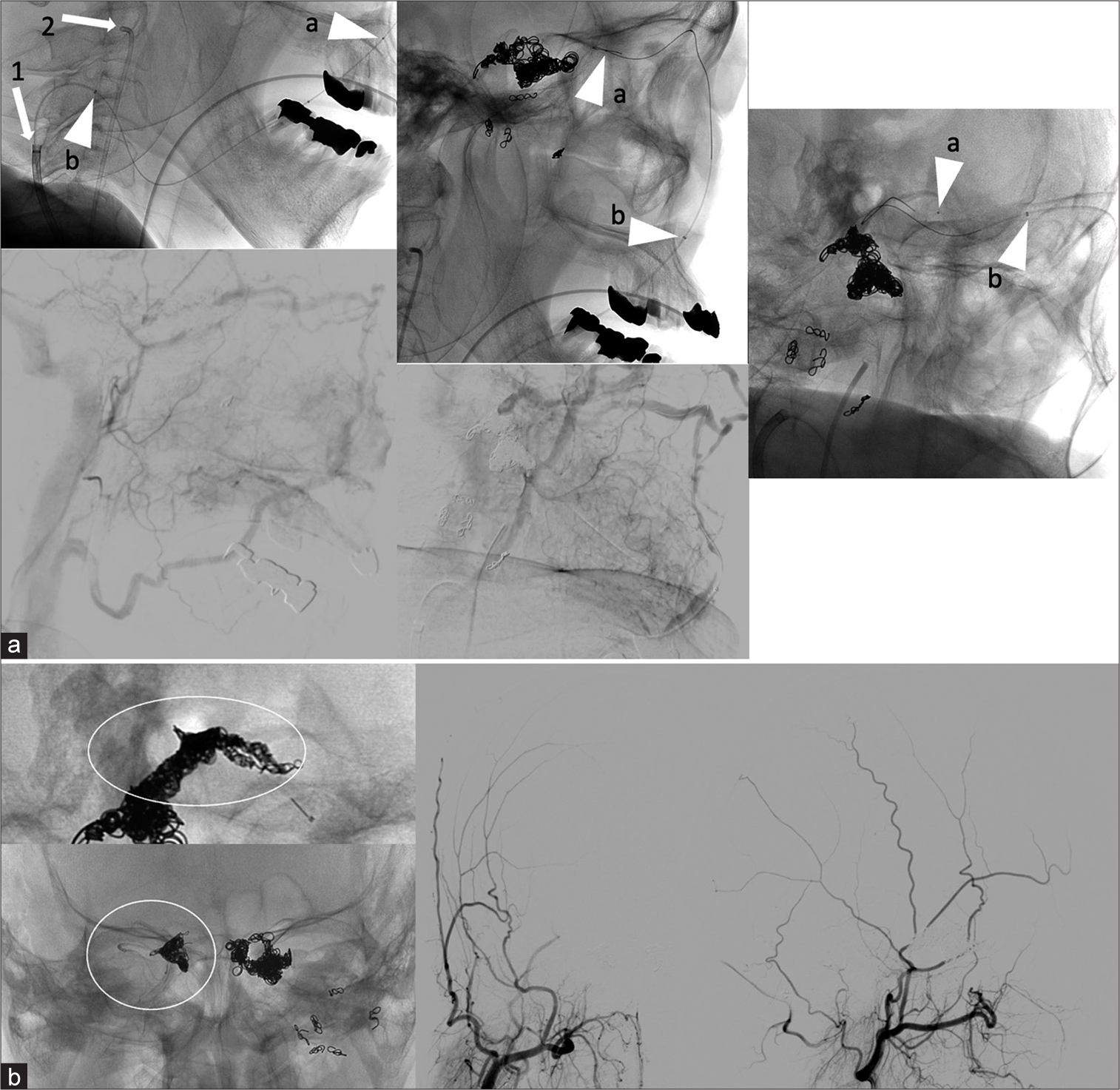
Operative X-ray and digital subtraction angiography (DSA) (a). 7 Fr guiding catheter (arrow 1) was navigated to right internal jugular vein, and 4 Fr diagnostic catheter (arrow 2) was in right external carotid artery. Micro catheter (MC; arrow head a) and distal access catheter (DAC; arrow head b) was navigated to facial vein. MC (arrow head a) was navigated to superior middle cerebral vein superior ophthalmic vein (SOV) through, and DAC (arrow head b) was placed into SOV. DSA shows approach route, facial vein. (b) Coils which were showed in the circle were inserted, and cavernous sinus dural arteriovenous fistula was completely occluded.
DISCUSSION
IPS is the preferred approach in TVE for CSDAVF.[
One problem with this approach is that the FV is a long vessel with strong tortuosity, so it is necessary to select a catheter and connector appropriately. It has been reported that about 9% of cases drain into the external jugular vein,[
Hirayama et al.[
The draining veins of CSDAVF include SOV, SMCV, SPS, IPS, uncal vein (UV), and prepontine bridging vein (PPBV). If the FV is selected as the approach route, there is concern that if the SOV is wedged with a microcatheter during treatment, venous blood that has no outflow pathway will be drained into cortical veins such as SMCV, UV, and PPBV, or into the brainstem. If the SOV is wedged by a microcatheter during treatment, venous blood flow may drain into cortical veins such as the SMCV, UV, or PPBV, or into the brainstem. In this case, the patient had PPP due to regurgitation into the SMCV, which was the source of hemorrhage, and the first step was to embolize this outflow tract. As with all AVFs, it is very important to check for the appearance of new outflow tracts with appropriate contrast. In this case, the patient was aware of tinnitus on the affected side several months before he was sent to the emergency department, so it is possible that the tinnitus originally flowed back into the transverse or sigmoid sinus. As it gradually occluded, the IPS also occluded, and the shunt blood flow probably went to the SMCV.
Hemorrhagic CSDAVF is a very rare condition, with 6 cases (1%) out of 469 cases in JR-NET 2.[
CONCLUSION
We experienced a case of TVE through FV for CSDAVF with hemorrhage onset. If IPS obstruction is identified preoperatively, it is useful to use the FV as the first choice of route. Furthermore, the use of Guidepost for DAC in this approach is very useful for accurate treatment.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agid R, Willinsky RA, Haw C, Souza MP, Vanek IJ, TerBrugge KG. Targeted compartmental embolization of cavernous sinus dural arteriovenous fistulae using transfemoral medial and lateral facial vein approaches. Neuroradiology. 2004. 46: 156-60
2. Alexandre AM, Sturiale AL, Bartolo A, Romi A, Scerrati A, Flacco ME. Endovascular treatment of cavernous sinus dural arteriovenous fistulas, Institutional series, systematic review and meta-analysis. Clin Neuroradiol. 2022. 32: 761-71
3. Biondi A, Milea D, Cognard C, Ricciardi GK, Bonneville F, van Effenterre R. Cavernous sinus dural fistulae treated by transvenous approach through the facial vein: Report of seven cases and review of the literature. AJNR Am J Neuroradiol. 2003. 24: 1240-6
4. Cho YD, Rhim JK, Yoo DH, Kang HS, Kim JE, Cho WS. Transvenous microguidewire looping technique for breach of ipsilateral inferior petrosal sinus occlusions en route to cavernous sinus dural arteriovenous fistulas. Interv Neuroradiol. 2016. 22: 590-5
5. Gupta V, Tuli A, Choudhry R, Agarwal S, Mangal A. Facial vein draining into external jugular vein in humans: Its variations, phylogenetic retention and clinical relevance. Surg Radiol Anat. 2003. 25: 36-41
6. Hiramatsu M, Sugiu K, Hishikawa T, Haruma J, Tokunaga K, Date I. Epidemiology of dural arteriovenous fistula in Japan: Analysis of Japanese registry of neuroendovascular therapy (JR-NET2). Neurol Med Chir (Tokyo). 2014. 54: 63-71
7. Hiramatsu M, Sugiu K, Hishikawa T, Nishihiro S, Kidani N, Takahashi Y. Results of 1940 embolizations for dural arteriovenous fistulas: Japanese registry of neuroendovascular therapy (JR-NET3). J Neurosurg. 2019. 28: 1-8
8. Hirayama K, Masuo O, Yako R, Matsumoto H, Nakao N. A case of cavernous sinus dural arteriovenous fistula treated with superior ophthalmic vein approach via the facial vein: Usefulness of triple coaxial catheter system. J Neuroendovasc Ther. 2014. 8: 201-6
9. Hou K, Li G, Luan T, Xu K, Yu J. Endovascular treatment of the cavernous sinus dural arteriovenous fistula: Current status and considerations. Int J Med Sci. 2020. 17: 1121-30
10. Kim MJ, Shin YS, Ihn YK, Kim BM, Yoon PH, Oh SY. Transvenous embolization of cavernous and paracavernous dural arteriovenous fistula through the facial vein: Report of 12 cases. Neurointervention. 2013. 8: 15-22
11. Kiyosue H, Hori Y, Okahara M, Tanoue S, Sagara Y, Matsumoto S. Treatment of intracranial dural arteriovenous fistulas: Current strategies based on location and hemodynamics, and alternative techniques of transcatheter embolization. Radiographics. 2004. 24: 1637-53
12. Reis CV, Gonzalez FL, Zabramski JM, Hassan A, Deshmukh P, Albuquerque FC. Anatomy of the superior ophthalmic vein approach for direct endovascular access to vascular lesions of the orbit and cavernous sinus. Neurosurgery. 2009. 5: 318-23
13. Rhim JK, Cho YD, Park JJ, Jeon JP, Kang HS, Kim JE. Endovascular treatment of cavernous sinus dural arteriovenous fistula with ipsilateral inferior petrosal sinus occlusion: A single-center experience. Neurosurgery. 2015. 77: 192-9
14. Yu SC, Cheng KM, Wong GK, Chan CM, Cheung JY, Poon WS. Transvenous embolization of dural carotid-cavernous fistulae with transfacial catheterization through the superior ophthalmic vein. Neurosurgery. 2007. 60: 1032-8 discussion 1037-8
15. Zhou Z, Xu K, Yu J. Transfemoral trans-facial vein-superior ophthalmic vein to embolize cavernous sinus dural arteriovenous fistulas. Front Neurol. 2022. 13: 1078185