- Department of Neurosurgery, Lisie Hospital, Kochi, Kerala, India.
- Department of Neurology, Kovai Medical Centre and Hospital, Coimbatore, Tamil Nadu, India.
- Department of Anaesthesia, Lisie Hospital, Kochi, Kerala, India.
Correspondence Address:
Biji Bahuleyan, Department of Neurosurgery, Lisie Hospital, Kochi, Kerala, India.
DOI:10.25259/SNI_483_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mariette Anto1, Rajesh Shankar Iyer2, Adarsh Manuel1, Akarsh Jayachandran1, Rosmy Jose3, Nisha John3, Puja Shyam3, Anjitha Thankachan1, Santhosh George Thomas1, Biji Bahuleyan1. Ceftriaxone-induced encephalopathy in a patient with multicentric glioma. 15-Jul-2022;13:303
How to cite this URL: Mariette Anto1, Rajesh Shankar Iyer2, Adarsh Manuel1, Akarsh Jayachandran1, Rosmy Jose3, Nisha John3, Puja Shyam3, Anjitha Thankachan1, Santhosh George Thomas1, Biji Bahuleyan1. Ceftriaxone-induced encephalopathy in a patient with multicentric glioma. 15-Jul-2022;13:303. Available from: https://surgicalneurologyint.com/surgicalint-articles/11720/
Abstract
Background: Ceftriaxone is a commonly used antibiotic in a wide range of local and systemic infections. Encephalopathy is a rare complication of ceftriaxone, often seen in older adults and those with renal insufficiency.
Case Description: A 73-year-old lady with prior history of hypertension and dyslipidemia presented with the complaints of slurred speech, gait imbalance, nocturnal vomiting, and progressively worsening headache. A magnetic resonance imaging of the brain revealed two intracerebral lesions involving the right frontal and temporal lobes, suggestive of multicentric glioma. She underwent craniotomy and excision of these lesions. The biopsy was reported as intra-axial tumors with features suggestive of the WHO Grade IV glioma. Postoperatively, she did not wake up. An electroencephalogram demonstrated triphasic waves suggestive of encephalopathy. The probable diagnosis of ceftriaxone-induced encephalopathy was made after ruling out other causes of delayed awakening after surgery. Ceftriaxone was discontinued and the patient improved within 2 days of withdrawal of ceftriaxone.
Conclusion: Drug-induced encephalopathy should be considered in the differential diagnosis of patients with delayed awakening after surgery. Discontinuation of the drug leads to the recovery of these patients.
Keywords: Ceftriaxone, Encephalopathy, Glioma, Surgery
INTRODUCTION
On account of their broad microbial spectrum and excellent tissue penetration, cephalosporins are frequently used to treat a wide variety of local and systemic infections.[
Ceftriaxone is rarely known to cause central nervous system (CNS) complications.[
Encephalopathy is an uncommon complication of the third- and fourth-generation cephalosporins.[
In this report, we present a case of ceftriaxone-induced encephalopathy (CIE) in a patient following craniotomy for glioma, who was given ceftriaxone as perioperative antibiotic prophylaxis.
CASE REPORT
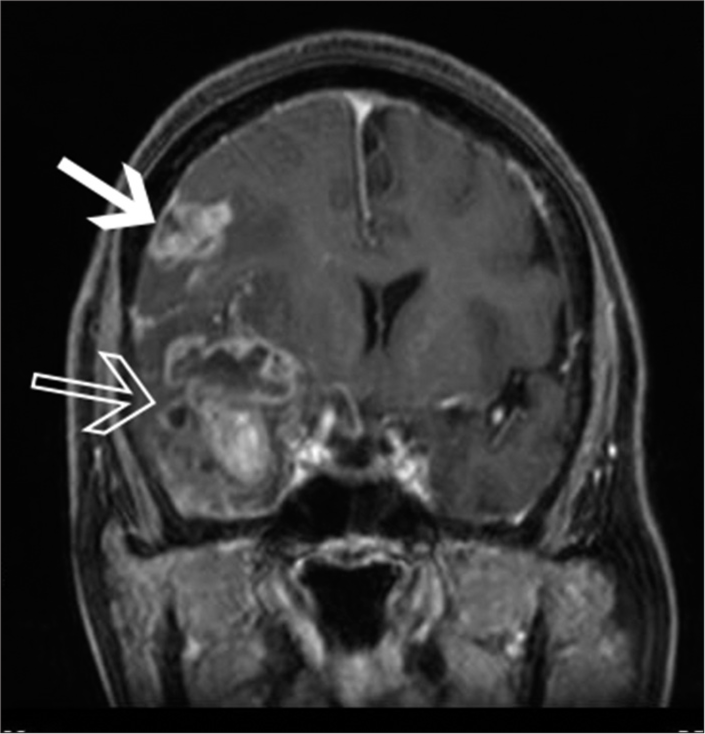
A 73-year-old female patient with prior history of hypertension and dyslipidemia was admitted with a 2-week history of dysarthria, gait imbalance, nocturnal vomiting, and progressively worsening headache. She gave a history of recent weight loss. She had no history of chronic cough, breast lump, or blackish discoloration of stools. General physical examination was normal. There was no breast lump. Abdominal and chest examinations were normal. On neurological examination, she was conscious and oriented. Cranial nerve examination was normal. She had a power of Grade 5 in all limbs. She had gait instability with a slight tendency to sway toward the left. Soft pyramidal signs were absent. Sensory examination was normal. Reflexes were normal bilaterally. Magnetic resonance imaging (MRI) of the brain [
Our preoperative radiological diagnosis was multicentric glioma. She was started on phenytoin sodium as a preoperative antiepileptic. Injection ceftriaxone 2 g was given intravenously as perioperative antibiotic prophylaxis. With neuronavigation guidance, she underwent right frontotemporal craniotomy, right anterior temporal lobectomy, amygdalohippocampectomy, and excision of the right frontal lesion. At surgery, the temporal lesion was found to be firmly attached to the dura with infiltration of the neocortex, hippocampus, and amygdala. The lesions were moderately vascular, suckable, and had cystic change, evidence of necrosis, and thrombosed veins within it. The surgery was uneventful with no intraoperative complications such as hypoxia or hypotension. The entire lesion in the frontal region, temporal neocortex, and hippocampus was removed. The lesion in the amygdala was only partially removed. The patient did not wake up fully after surgery. However, since her breathing was normal, she was extubated.
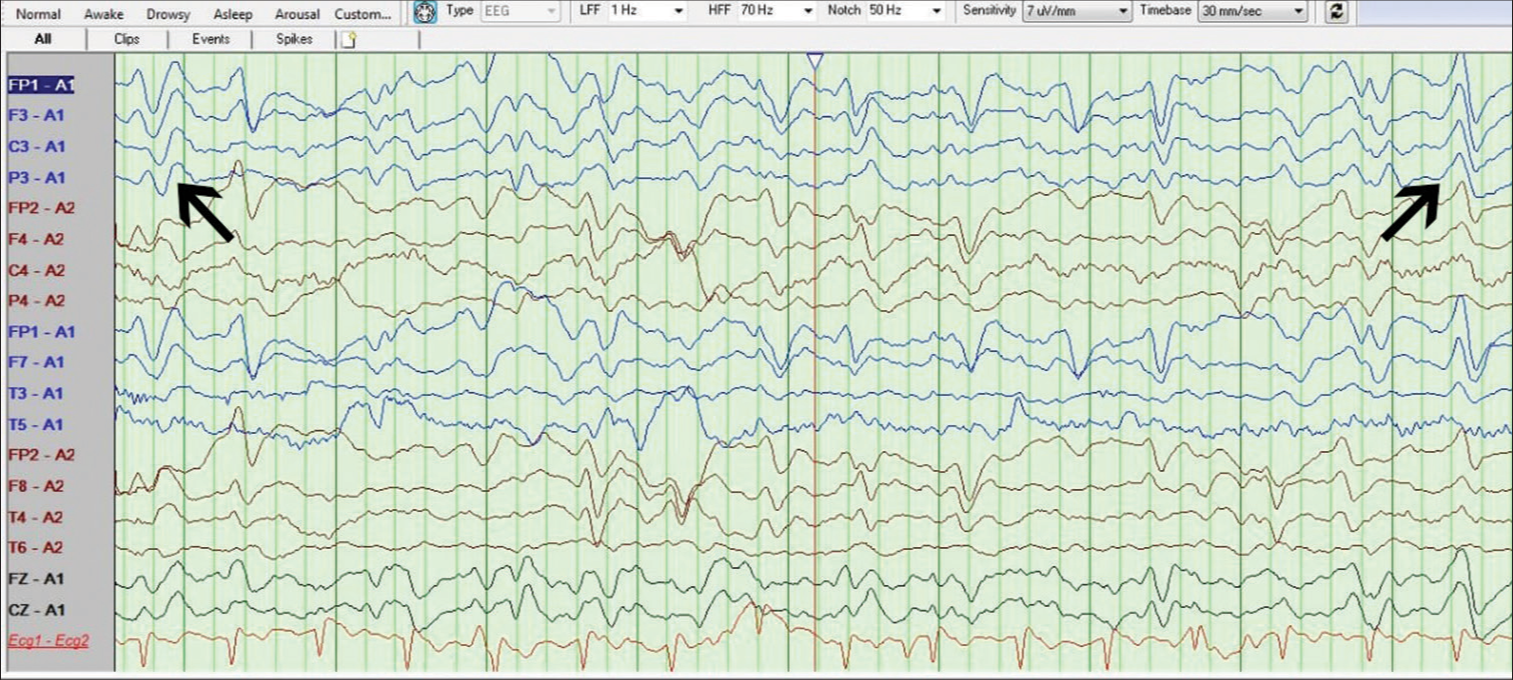
The following causes of delayed awakening after surgery were considered: (i) NCSE, ii) hypoglycemia, (iii) operative site hematoma, (iv) thromboembolic cerebral infarcts, (v) electrolyte imbalance, (vi) metabolic encephalopathy, and (vii) extensive brain tissue resection. Considering NCSE as a probable cause for the delayed awakening, we administered an additional loading dose of phenytoin sodium in the immediate postoperative period in the operating room. We also added levetiracetam as an add-on antiepileptic. An emergency MRI brain done in the immediate postoperative period confirmed total excision of the right frontal and temporal lesions with no postoperative hematoma or infarcts that would explain her altered sensorium. Blood tests were done to rule out all possible causes of encephalopathy including liver function tests, renal function tests, and serum electrolyte panel, all of which were normal. A bedside electroencephalogram (EEG) showed a background activity of 4–5 Hz over posterior head regions. Triphasic waves with anteroposterior lag were seen [
DISCUSSION
The exact pathophysiology by which ceftriaxone causes encephalopathy remains unidentified.[
Renal impairment[
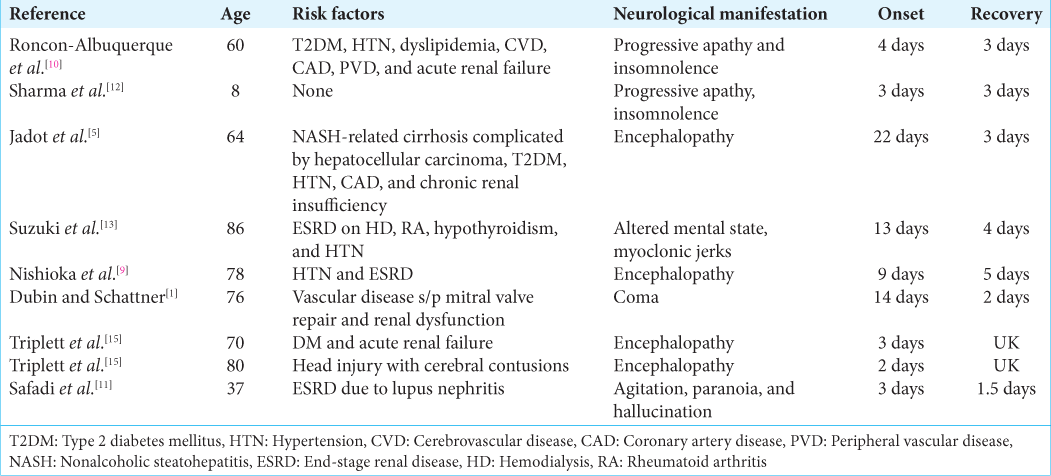
In the literature, the onset of ceftriaxone-induced neurotoxicity (CIN) is between 1 and 10 days after starting the drug.[
Diagnosis of this complication is often difficult as ceftriaxone is an underrecognized cause of neurotoxicity.[
An important differential diagnosis to consider in delayed awakening after surgery is NCSE. As seen in our case, CIE should also be considered in a similar scenario. The presence of triphasic waves, as seen in our case, clearly suggests metabolic encephalopathy than NCSE.[
In CIN, spontaneous improvement in patients’ clinical status is observed within 1–12 days of withholding ceftriaxone.[
In 2021, Lacroix et al.[
Renal dysfunction was the most common risk factor. Renal dysfunction is seen in all the published articles except in the case reported by Sharma et al. Our patient was also similar to the one referred to by Sharma et al.[
CIE is an underdiagnosed and underreported clinical entity. Considering the risk of neurotoxicity, the use of ceftriaxone as perioperative antibiotic prophylaxis should not be considered in older adults and/or in patients with renal dysfunction. Instead, antibiotics such as cefoperazone or amoxiclav that are very rarely reported to cause neurotoxicity should be contemplated as an alternative for perioperative antibiotic prophylaxis in such cases.
A limitation of our case report is that we were unable to measure the CSF level of ceftriaxone.
Our case is novel in that; (i) it is the first reported case of CIE in a neurosurgical patient diagnosed with multicentric glioma and (ii) the onset of encephalopathy was observed in less than a day.
CONCLUSION
CIE is a rare complication most commonly seen in older adults with renal failure. Ceftriaxone should be considered a cause of encephalopathy in patients who were administered the drug with delayed awakening after surgery. Since this complication is underdiagnosed and altered mental status has multiple differentials, the diagnosis of this condition remains clinically challenging. Clinical vigilance of the condition, EEG findings, and when possible, measurement of ceftriaxone concentration in serum and CSF can aid in diagnosing this condition. Neurological conditions as a risk factor need further exploration to help us better understand and prevent this complication. Prompt diagnosis and cessation of the drug can revert this condition. Clinicians should be more aware of this iatrogenic complication.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Dubin I, Schattner A. Iatrogenic coma: Ceftriaxone-associated encephalopathy. Postgrad Med J. 2018. 94: 357-8
2. Grill MF, Maganti R. Cephalosporin-induced neurotoxicity: Clinical manifestations, potential pathogenic mechanisms, and the role of electroencephalographic monitoring. Ann Pharmacother. 2008. 42: 1843-50
3. Hagiya H, Miyawaki K, Yamamoto N, Yoshida H, Kitagawa A, Asaoka T. Ceftriaxone-induced neurotoxicity in a patient after pancreas-kidney transplantation. Intern Med. 2017. 56: 3103-7
4. Inoue Y, Doi Y, Arisato T, Sugioka S, Koga K, Nishioka K. Three cases of hemodialysis patients receiving high-dose ceftriaxone: Serum concentrations and its neurotoxicity. Kidney Int Rep. 2017. 2: 984-7
5. Jadot L, Judong A, Canivet JL, Lorenzo-Villalba N, Damas P. Ceftriaxone-induced encephalopathy: A pharmacokinetic approach. Eur J Case Rep Intern Med. 2021. 8: 003011
6. Kim KB, Kim SM, Park W, Kim JS, Kwon SK, Kim HY. Ceftiaxone-induced neurotoxicity: Case report, pharmacokinetic considerations, and literature review. J Korean Med Sci. 2012. 27: 1120-3
7. Kotani A, Hirai J, Hamada Y, Fujita J, Hakamata H. Determination of ceftriaxone concentration in human cerebrospinal fluid by high-performance liquid chromatography with UV detection. J Chromatogr B Analyt Technol Biomed Life Sci. 2019. 1124: 161-4
8. Lacroix C, Bera-Jonville AP, Montastruc F, Velly L, Micallef J, Guilhaumou R. Serious neurological adverse events of ceftriaxone. Antibiotics (Basel). 2021. 10: 540
9. Nishioka H, Cho Y, Irie K, Kanamori M. Ceftriaxone-associated encephalopathy in a patient with high levels of ceftriaxone in blood and cerebrospinal fluid. Int J Infect Dis. 2022. 116: 223-5
10. Roncon-Albuquerque R, Pires I, Martins R, Real R, Sousa G. Ceftriaxone-induced acute reversible encephalopathy in a patient treated for a urinary tract infection. 2009. 67: 72-5
11. Safadi S, Mao M, Dillon JJ. Ceftriaxone-induced acute encephalopathy in a peritoneal dialysis patient. Case Rep Nephrol. 2014. 2014: 108185
12. Sharma N, Batish S, Gupta A. Ceftriaxone-induced acute reversible encephalopathy in a patient with enteric fever. Indian J Pharmacol. 2012. 44: 124-5
13. Suzuki S, Naito S, Numasawa Y, Asada M, Shoji N, Zeniya M. encephalopathy induced by high plasma and cerebrospinal fluid ceftriaxone concentrations in a hemodialysis patient. Intern Med. 2019. 58: 1775-9
14. Tan ML, Tun WW. Reversible choreoathetosis in a patient with end-stage renal disease from administration of ceftriaxone. Cureus. 2019. 11: e5764
15. Triplett JD, Lawn ND, Chan J, Dunne JW. Cephalosporin-related neurotoxicity: Metabolic encephalopathy or nonconvulsive status epilepticus?. J Clin Neurosci. 2019. 67: 163-6






Johnson Cheenath
Posted July 22, 2022, 10:37 am
Excellent paper. Well written and an eye opener.
It will be really helpful to all neurosurgeons as this is one of the most commonly used antibiotics in neurosurgery