- Department of Neurosurgery, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia
- College of Medicine, Almothana Bin Haretha, Ar Rass, Saudi Arabia
- Department of Medicine, Qu, Alqassim, Saudi Arabia
- College of Medicine, King Abdulaziz University,Jeddah, Saudi Arabia
- Department of Pathology, King Abdul-Aziz Medical City, National Guard Health Affairs, Jeddah, Saudi Arabia
- Department of Neurosurgery, King Abdulaziz Medical City, Jeddah, Saudi Arabia.
Correspondence Address:
Khalid Talal Alghamdi, Department of Neurosurgery, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia.
DOI:10.25259/SNI_414_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Khalid Talal Alghamdi1, Ghaida Abdullah Albattah2, Shoug Saleh Alnasyan3, Ali Zaki Alhabib4, Alaa Mohammed Noor Samkari5, Hussam Yousef Kutub6. Central nervous system metastasis in a young female patient with primary mediastinal large B-cell lymphoma: A case report and literature review. 28-Jul-2023;14:270
How to cite this URL: Khalid Talal Alghamdi1, Ghaida Abdullah Albattah2, Shoug Saleh Alnasyan3, Ali Zaki Alhabib4, Alaa Mohammed Noor Samkari5, Hussam Yousef Kutub6. Central nervous system metastasis in a young female patient with primary mediastinal large B-cell lymphoma: A case report and literature review. 28-Jul-2023;14:270. Available from: https://surgicalneurologyint.com/surgicalint-articles/12460/
Abstract
Background: Primary mediastinal B-cell lymphoma (PMBCL) is a subtype of diffuse large B-cell lymphoma that originates from a B cell in the thymus. It usually affects young female.
Case description: A 30-year-old woman presented with mediastinal mass with history of shortness of breath and chest pain. blood analysis showed low levels of hemoglobin, hematocrit, and mean corpuscular volume and high red cell distribution width. A computed tomography (CT)-guided mediastinal core biopsy disclosed primary mediastinal large B-cell lymphoma (PMLBL) with a nongerminal center phenotype and lung tissue infiltrate. Moreover, after undergoing six cycles of rituximab, cyclophosphamide, hydroxydaunomycin, Oncovin, and prednisone (R-CHOP) chemotherapy and mediastinal radiotherapy, the patient presented with headache and visual disturbance due to multiple supratentorial lesions.
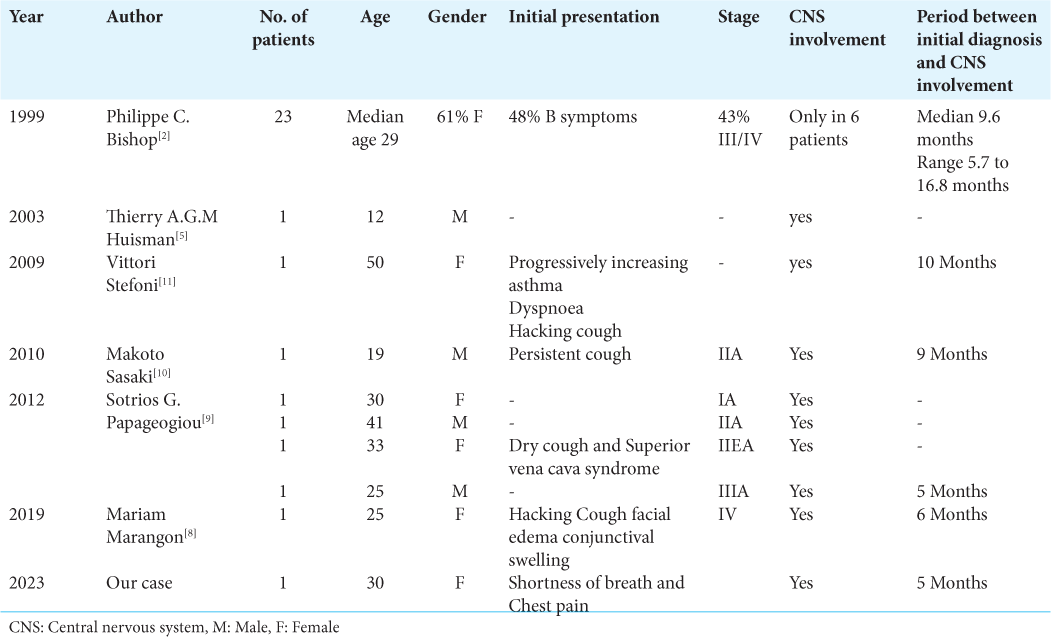
Conclusion: Till date, only a few cases of central nervous system (CNS) metastasis have been reported in the literature. Moreover, CNS metastasis of refractory PMBCL is an uncommon event with a poor prognosis. Brain metastases are often the ultimate fatal consequence of many aggressive cancers, so early detection and treatment are important.
Keywords: Central nervous system metastasis, Primary mediastinal B-cell lymphoma, Radiotherapy, R-CHOP regimen
INTRODUCTION
Primary mediastinal B-cell lymphoma (PMBCL) is characterized by a diffuse proliferation of medium- to large-sized B cells and is accompanied by sclerosis and some degree of compartmentalization.[
Brain metastases are often the ultimate fatal consequence of many aggressive cancers.[
CASE DESCRIPTION
A 30-year-old woman presented at our institution with a mediastinal mass. She had a history of shortness of breath and chest pain. The physical examination was normal. Further investigations started with blood analysis, which showed low levels of hemoglobin, hematocrit, and mean corpuscular volume and high red cell distribution width. A peripheral blood smear report indicated moderate microcytic hypochromic anemia. A computed tomography (CT)-guided mediastinal core biopsy disclosed primary mediastinal large B-cell lymphoma (PMLBL) with a nongerminal center phenotype and lung tissue infiltrate. Immunohistochemistry showed the following target cells: CD20, CD23 (with focal weak positivity), CD30 (present in a subset of cells), BcI2 (with focal positive staining), Bcl6++, and MUM1++. Further analysis included a bone marrow aspiration, which revealed no signs of infiltration or abnormal cells. The final diagnosis was PMLBL located in the anterior mediastinum. The patient received six cycles of R-CHOP chemotherapy and 18 sessions of radiotherapy. The only remarkable event was stomatitis, which was promptly treated with an oral doxycycline gargle and fluconazole.
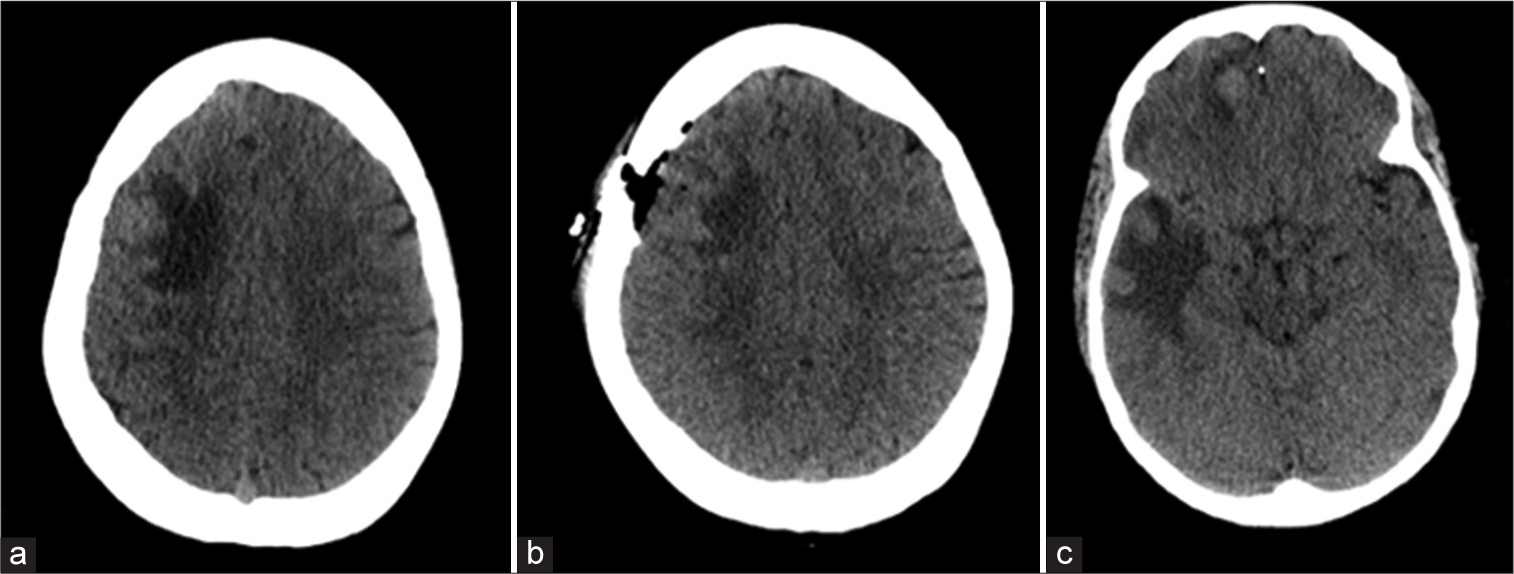
Five months later, she presented at the emergency department with a headache and episodes of vision changes lasting seconds for the past 4 days. A cranial CT scan was performed, which indicated multiple supratentorial lesions [
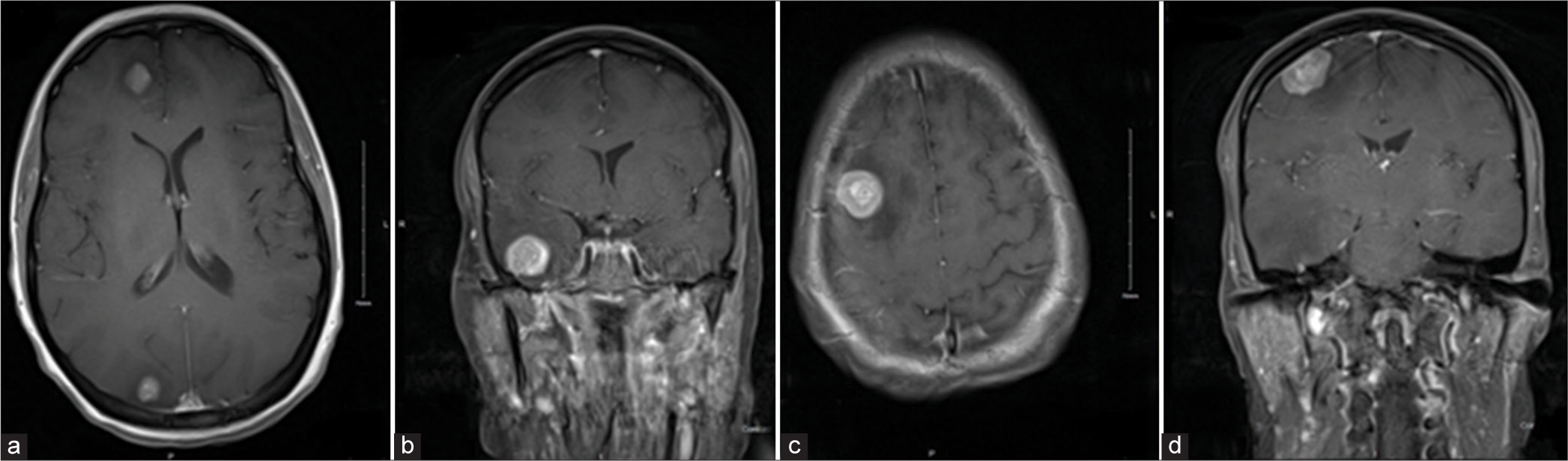
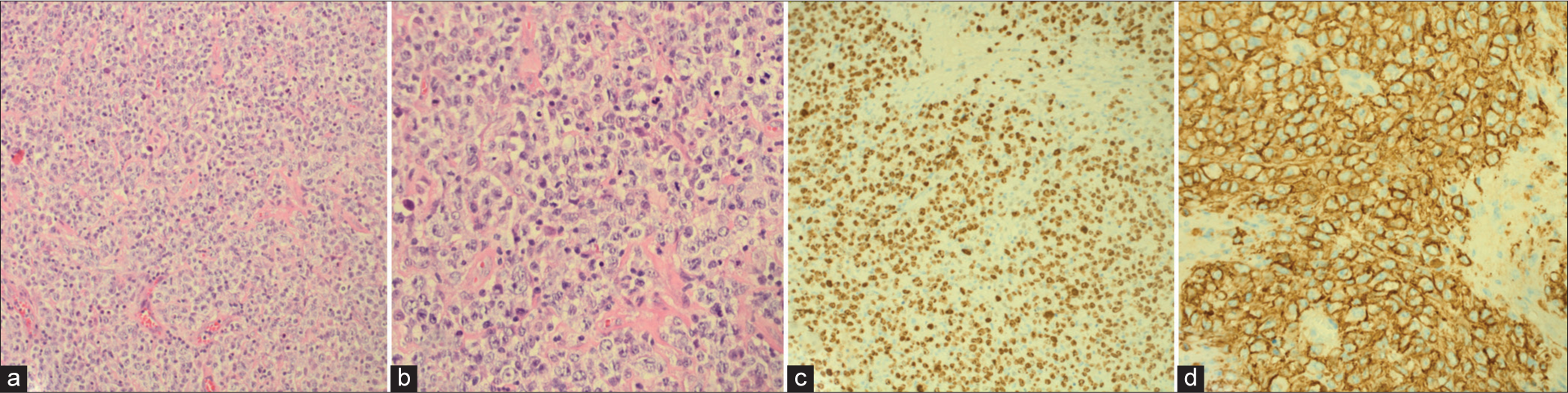
An excisional biopsy was performed through a right frontoparietal mini-craniotomy. During the surgery, a bulging layer of the cortex covered the tumor. The tumor was firm and yellow, with a clear plane identified, and histopathology confirmed the presence of lymphoma cells. The biopsy showed diffuse sheets of large neoplastic cells with round nuclei. These cells exhibited vesicular chromatin and prominent central nucleoli, as well as membrane-bound multiple nucleoli. Mitotic figures were observed [
Figure 3:
(a and b) H&E stained sections show diffuse sheets of large neoplastic cells with round nuclei that exhibit vesicular chromatin and prominent central nucleoli to membrane bound multiple nucleoli. Mitotic figures are seen. (c) Immunohistochemistry shows large cells with positive for CD20, CD30, BCL6, MUM1, and C-MYC (40%), while negative for BCL2 and CD23. (d) Immunohistochemistry shows Ki67 proliferative index that is positive in 80% of tumor cells.
Immunohistochemistry indicated the presence of large cells with positive staining for CD20, CD30, BCL6, MUM1, and C-MYC (40%) and negative staining for BCL2 and CD23. The Ki67 Proliferative Index was found to be positive in 80% of tumor cells. Based on these findings, the final diagnosis was progressive secondary CNS large B-cell lymphoma. After the diagnosis, the patient underwent salvage chemotherapy MATRIX/RISE for two cycles, followed by an auto-stem cell transplant.
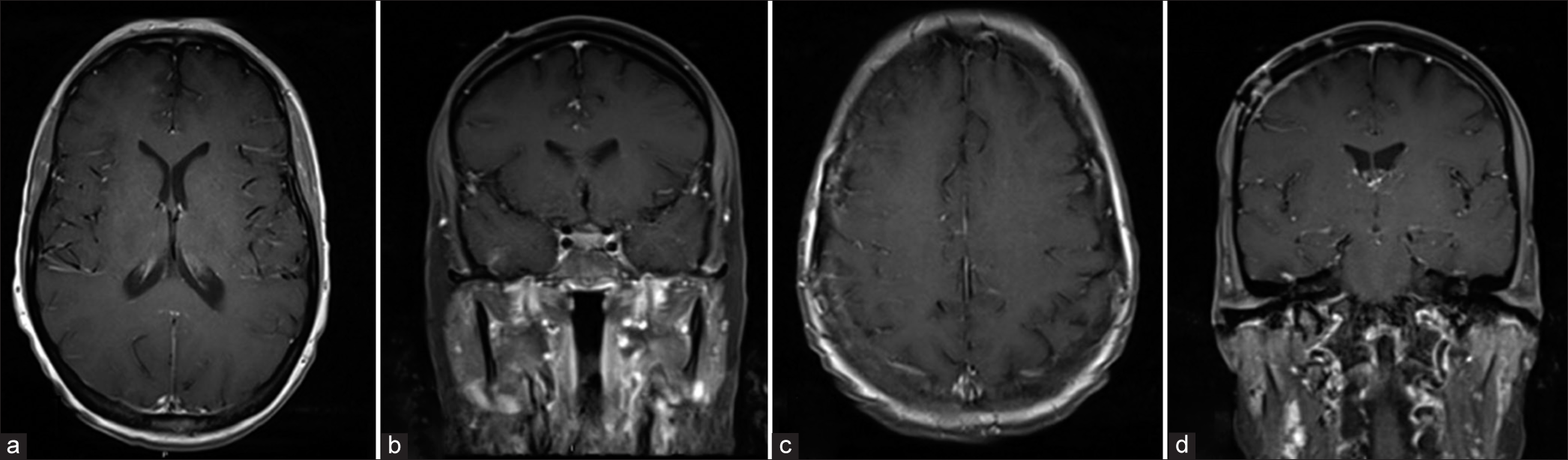
Seven weeks after surgical resection, the patient was observed to be recovering well. The MRI scan indicated that the right frontal lymphomatous lesions had resolved and that there had been a reduction in the size of the other lesions [
DISCUSSION
PMBCL is characterized by a diffuse proliferation of medium- to large-sized B cells and is accompanied by sclerosis and some degree of compartmentalization.[
The previous studies have identified some potential risk factors for CNS involvement, which include two or more extranodal involvements, especially if there is bone marrow involvement and elevated lactate dehydrogenase (LDH).[
CONCLUSION
Brain metastases are often the ultimate fatal consequence of numerous aggressive cancers. Therefore, we encourage physicians to maintain a high level of suspicion for early detection and treatment of PMBCL so that the disease progression can be managed. We also recommend conducting further investigation and performing an MRI for any patient with PMBCL as part of the initial assessment and when they present with neurological symptoms. Furthermore, it is important to educate patients about the symptoms so that they can seek help and visit the hospital if they develop any of them.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Beaumont TL, Kupsky WJ, Barger GR, Sloan AE. Gliosarcoma with multiple extracranial metastases: Case report and review of the literature. J Neurooncol. 2007. 83: 39-46
2. Bishop PC, Wilson WH, Pearson D, Janik J, Jaffe ES, Elwood PC. CNS involvement in primary mediastinal large B-cell lymphoma. J Clin Oncol. 1999. 17: 2479-85
3. Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML. A revised European-American classification of lymphoid neoplasms: A proposal from the International Lymphoma Study Group. Blood. 1994. 84: 1361-92
4. Hill QA, Owen RG. CNS prophylaxis in lymphoma: Who to target and what therapy to use. Blood Rev. 2006. 20: 319-32
5. Huisman TA, Tschirch F, Schneider JF, Niggli F, MartinFiori E, Willi UV. Burkitt’s lymphoma with bilateral cavernous sinus and mediastinal involvement in a child. Pediatr Radiol. 2003. 33: 719-21
6. Jiao C, Zvonkov E, Lai X, Zhang R, Liu Y, Qin Y. 4SCAR2, 0 A multi-CAR-T therapy regimen for the treatment of relapsed/refractory B cell lymphomas. Blood Cancer J. 2021. 11: 59
7. Lazzarino M, Orlandi E, Paulli M, Boveri E, Morra E, Brusamolino E. Primary mediastinal B-cell lymphoma with sclerosis: An aggressive tumor with distinctive clinical and pathologic features. J Clin Oncol. 1993. 11: 2306-13
8. Marangon M, Casadei B, Broccoli A, Argnani L, Cavo M, Zinzani PL. Management of central nervous system relapse in a young patient affected by primary mediastinal large B-cell lymphoma: A case report. Clin Case Rep. 2020. 8: 933-7
9. Papageorgiou SG, Diamantopoulos P, Levidou G, Angelopoulou MK, Economopoulou P, Efthimiou A. Isolated central nervous system relapses in primary mediastinal large B-cell lymphoma after CHOP-like chemotherapy with or without Rituximab. Hematol Oncol. 2013. 31: 10-7
10. Sasaki M, Sugimoto K, Masuda A, Tsukune Y, Yahata Y, Komatsu N. Early CNS relapse in a good-risk primary mediastinal large B-cell lymphoma after combined chemo-and radio-therapy. J Neurooncol. 2010. 99: 295-6
11. Stefoni V, Broccoli A, Pellegrini C, Derenzini E, Fina M, Zinzani PL. CNS recurrence of primary mediastinal large b-cell lymphoma after complete remission. J Neurooncol. 2009. 95: 135-9
12. Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016. 127: 2375-90