- Department of Neurology, Weill Cornell Medicine, New York City, New York, United States.
Correspondence Address:
Melvin Parasram, Department of Neurology, Weill Cornell Medicine, New York City, New York, United States.
DOI:10.25259/SNI_605_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Melvin Parasram, Shamelia Y. Loiseau. Cerebral microhemorrhages in severe COVID-19 pneumonia. 26-Aug-2022;13:380
How to cite this URL: Melvin Parasram, Shamelia Y. Loiseau. Cerebral microhemorrhages in severe COVID-19 pneumonia. 26-Aug-2022;13:380. Available from: https://surgicalneurologyint.com/surgicalint-articles/11831/
Abstract
Background: Cerebral microhemorrhages are a complication in patients with severe COVID-19 pneumonia.
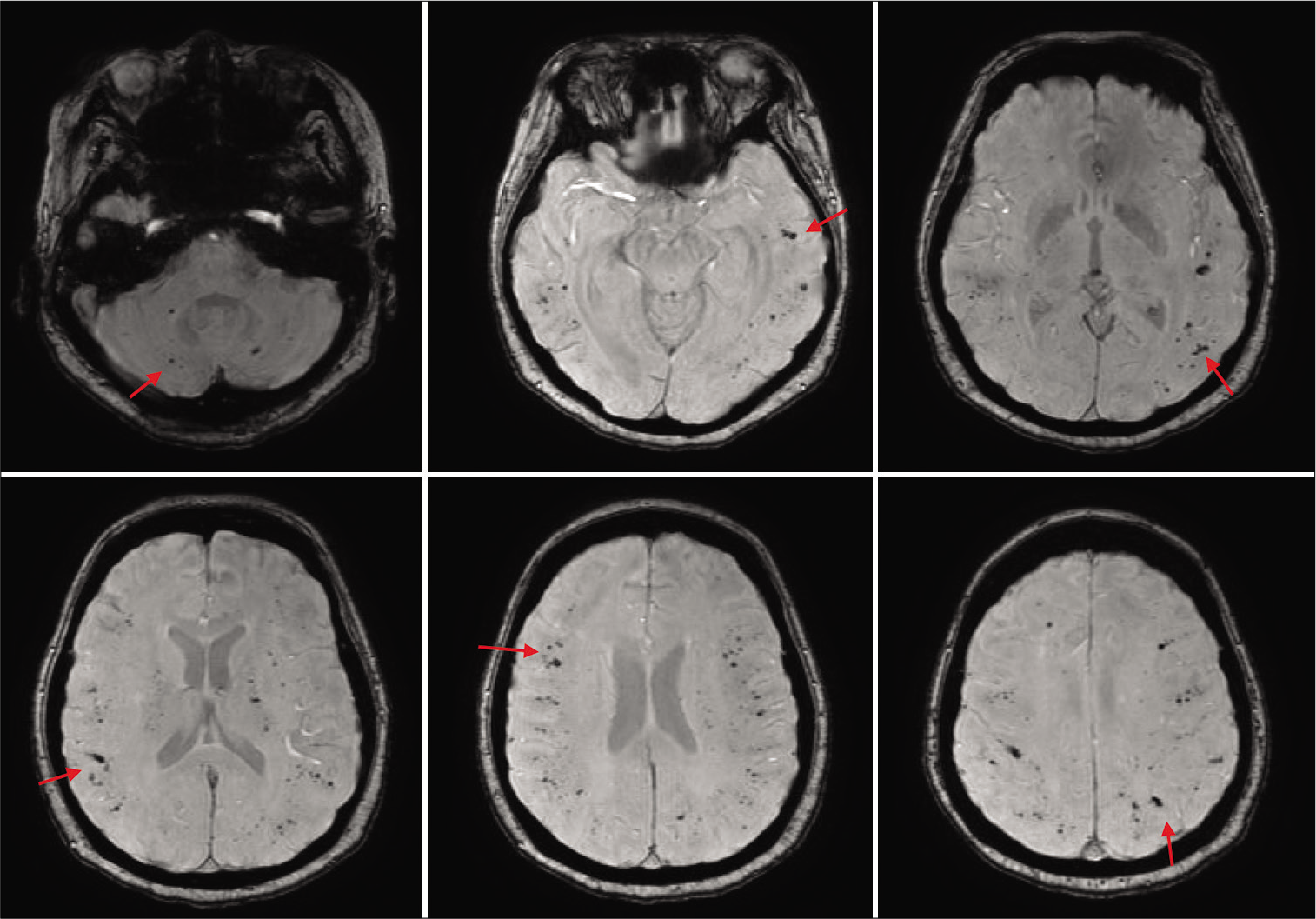
Case Description: A 50-year-old woman presented to the hospital with shortness of breath due COVID-19 (SARS-CoV-2, alpha variant) pneumonia. Her hospital course was complicated by hypoxic respiratory failure requiring intubation and severe acute respiratory distress syndrome. She received a tracheostomy for ongoing ventilator support after prolonged intubation. Her mental status was notable for disorientation and severe agitation for which a magnetic resonance imaging (MRI) of the brain was obtained. MRI revealed numerous microhemorrhages predominantly at the gray-white matter junctions.
Conclusion: Cerebral microhemorrhages in severe COVID-19 pneumonia are associated with critical illness, increased mortality, and worse functional outcome. The pathophysiology of cerebral microhemorrhages in COVID-19 is unknown.
Keywords: Cerebral microhemorrhages, COVID-19, Endotheliopathy, Hypoxia, SARS-CoV-2
IMAGE REPORT
A 50-year-old woman with medical history of hypertension presented to the hospital with shortness of breath due COVID-19 (SARS-CoV-2, alpha variant) pneumonia. Her hospital course was complicated by hypoxic respiratory failure requiring intubation. She was treated with convalescent plasma and remdesivir. The intensive care course was notable for severe acute respiratory distress syndrome requiring proning. She received a tracheostomy for ongoing ventilator support after prolonged intubation. Her mental status was notable for disorientation and severe agitation for which a magnetic resonance imaging (MRI) of the brain was obtained. MRI revealed numerous microhemorrhages predominantly at the gray-white matter junctions [
Cerebral microhemorrhages in COVID-19 have been associated with critical illness, increased mortality, and worse functional outcome.[
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agarwal S, Jain R, Dogra S, Krieger P, Lewis A, Nguyen V. Cerebral microbleeds and leukoencephalopathy in critically Ill patients with COVID-19. Stroke. 2020. 51: 2649-55
2. Radmanesh A, Derman A, Lui YW, Raz E, Loh JP, Hagiwara M. COVID-19-associated diffuse leukoencephalopathy and microhemorrhages. Radiology. 2020. 297: E223-7
3. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020. 395: 1417-8