- Department of Neurosurgery, Saiseikai Shiga Hospital, Ritto, Shiga, Japan.
Correspondence Address:
Shigeomi Yokoya, Department of Neurosurgery, Saiseikai Shiga Hospital, Ritto, Shiga, Japan.
DOI:10.25259/SNI_546_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shigeomi Yokoya, Hideki Oka, Akihiko Hino. Cerebral venous thrombosis following spontaneous intracranial hypotension diagnosed by craniotomy: A case report and diagnostic pitfalls. 27-Jul-2021;12:367
How to cite this URL: Shigeomi Yokoya, Hideki Oka, Akihiko Hino. Cerebral venous thrombosis following spontaneous intracranial hypotension diagnosed by craniotomy: A case report and diagnostic pitfalls. 27-Jul-2021;12:367. Available from: https://surgicalneurologyint.com/surgicalint-articles/11006/
Abstract
Background: Cerebral vein and dural sinus thrombosis (CVT) is a rare but important complication of spontaneous intracranial hypotension (SIH). The diagnosis is difficult in cases lacking typical symptoms and typical imaging findings.
Case Description: A 29-year-old male patient with a seizure attack was admitted to our hospital. Based on the head imaging findings, we misdiagnosed the patient with primary cerebral parenchymal lesion and performed an open biopsy. However, during the procedure, the patient was diagnosed with low cerebrospinal fluid pressure and cerebral cortical vein thrombosis.
Conclusion: Thus, CVT due to SIH should be considered as a probable cause of secondary parenchymal lesions.
Keywords: Cerebral vein and dural sinus thrombosis, Isolated cortical venous thrombosis, Parenchymal lesion, Spontaneous intracranial hypotension
INTRODUCTION
Spontaneous intracranial hypotension (SIH) is an unusual neurological situation caused by low cerebrospinal fluid (CSF) volume, and the symptoms are characterized by an orthostatic headache. The neurological imaging findings useful for its diagnosis include subdural hematoma or effusion, diffuse pachymeningeal enhancement, and engorgement of the venous structure.[
SIH is rarely known to cause cerebral vein and dural sinus thrombosis (CVT). The prevalence of CVT followed by SIH is approximately 2.1%,[
Herein, we present a case of brain parenchymal lesions due to CVT caused by SIH. We confirmed low CSF pressure and thrombosis of the cortical vein during the craniotomy procedure and made a final diagnosis.
CASE DESCRIPTION
A 29-year-old male with no relevant medical history was transported to our hospital twice for tonic–clonic seizures. Although he had no history of head/spinal trauma or surgery, he reported a 1-week history of generalized dull headache that was not orthostatic. On arrival at the hospital, his consciousness level was E4V5M6 on the Glasgow Coma Scale, with no abnormal neurological findings. Laboratory test results were negative for autoantibodies, coagulation disorders, infectious diseases, and tumor markers, and the possibility of a hypercoagulable state was excluded.
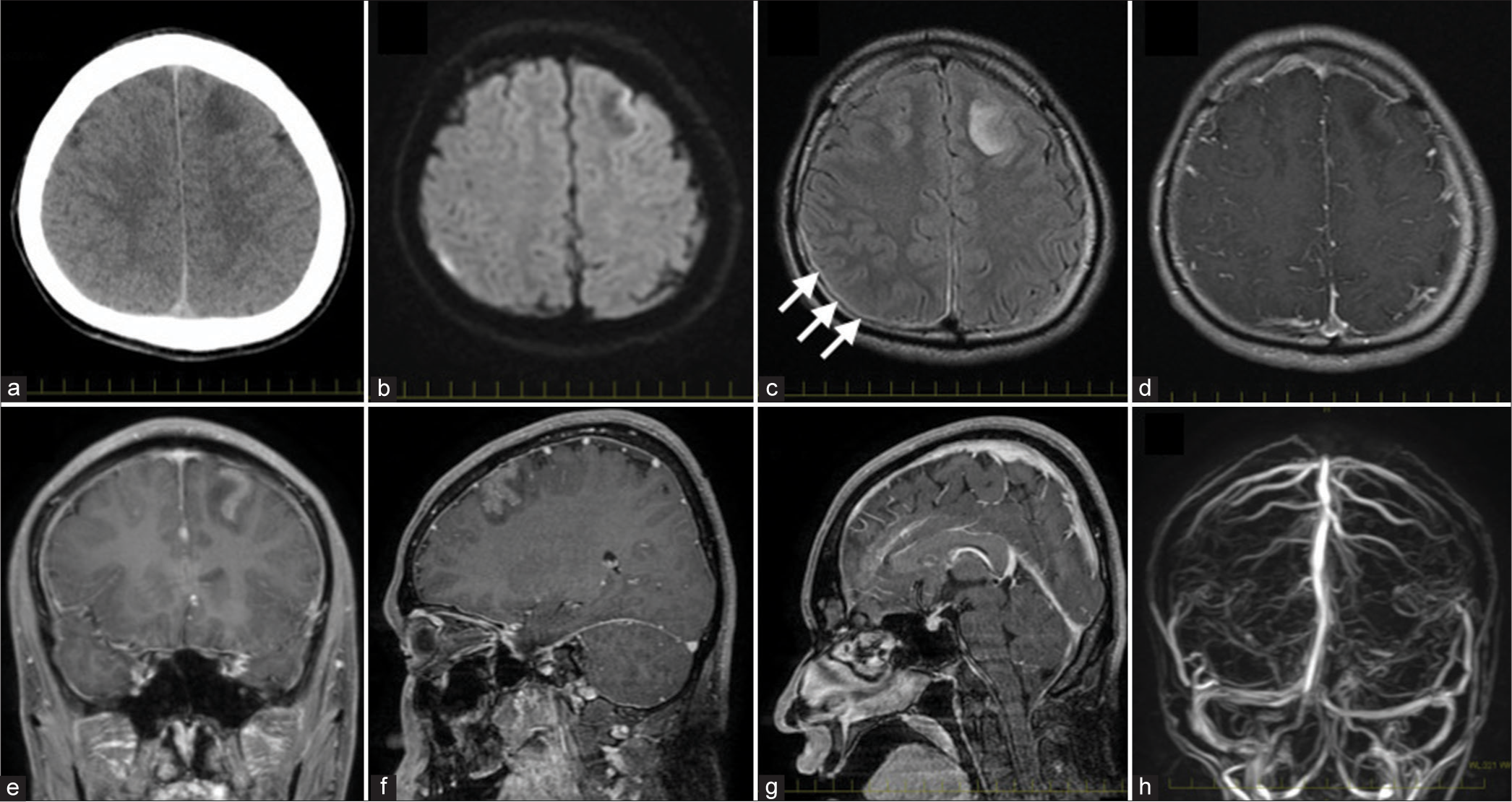
A head computed tomography scan performed after arrival at the hospital showed a low-density area in the left frontal lobe [
Figure 1:
Neuroimaging findings of the patient. Head computed tomography performed on admission reveals a low-density area in the left frontal cortex (a). Axial image from diffusion-weighted magnetic resonance imaging (MRI) reveals no abnormalities that indicate acute cerebral ischemia (b). Fluid-attenuated inversion recovery (FLAIR) shows high-intensity lesions in the left frontal cortex and very thin subdural hematoma (arrows) (c). Gadolinium-enhanced MRI shows leptomeningeal enhancement along the superior frontal gyrus, which is involved in focal cortical hyperintensity in the left frontal lobe of FLAIR imaging (d-f). Note that dural thickening, pituitary swelling, and tonsil herniation are not observed (e and g). Magnetic resonance venography shows patency of the intracranial main venous system (h).
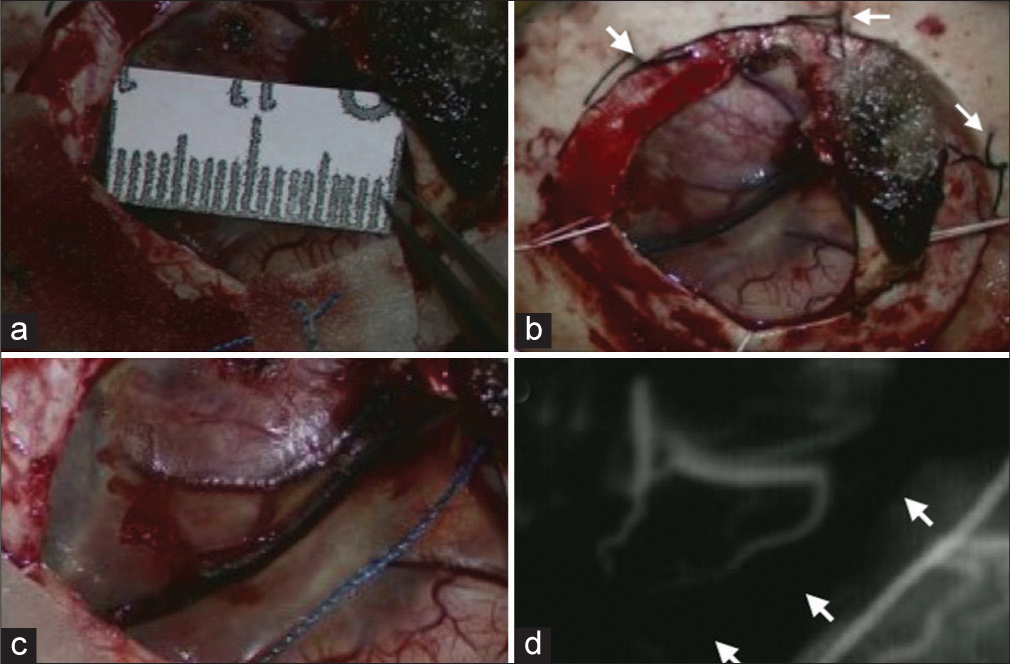
The patient underwent open biopsy on the 5th day of admission because the imaging findings were suggestive of malignant brain tumors. After craniotomy, we had to change his head position from 15 to 20 cm above the heart to 0 cm and perform a tack-up suture in a hurry because we noticed that the dura mater separated away from the skull spontaneously and steadily because of low intracranial pressure [
Figure 2:
Intraoperative photographs of the patient. The fluid-attenuated inversion recovery high-intensity lesion is exposed through small craniotomy (a). Note that a tack-up suture is placed (arrows) since the dura mater separates away from the skull spontaneously (a and b), although the brain does not look sunken in the photographs because we lowered the patient’s head position to increase the intracranial pressure. Magnified intraoperative photo shows that the cortical vein is discolored (black) (c), and indocyanine green video angiography shows the absence of flow that signifies thrombosis of the vein (d).
Hydration and bed rest gradually improved his headache. A lumbar puncture performed 20 days after admission demonstrated an opening pressure of 170 mmH2O, and he was discharged on the 33rd day of hospitalization with no neurological deficits.
DISCUSSION
This case brings to light some important clinical issues. First, atypical clinical symptoms and imaging findings could make SIH diagnosis difficult, especially with brain parenchymal lesions. In the present case, it was difficult to suspect low CSF pressure during admission, because the patient presented atypical clinical (the onset was not an orthostatic headache but a seizure attack) and imaging findings (subdural hematoma or effusion was not clear, dura thickening was not obvious, pituitary swelling was not observed), and the parenchymal lesion was observed.
It should be noted that SIH should be considered even when orthostatic headache is absent or unknown. Moreover, seizures are quite common as the first symptom of CVT onset. According to past literature in which 42 case reports were reviewed,[
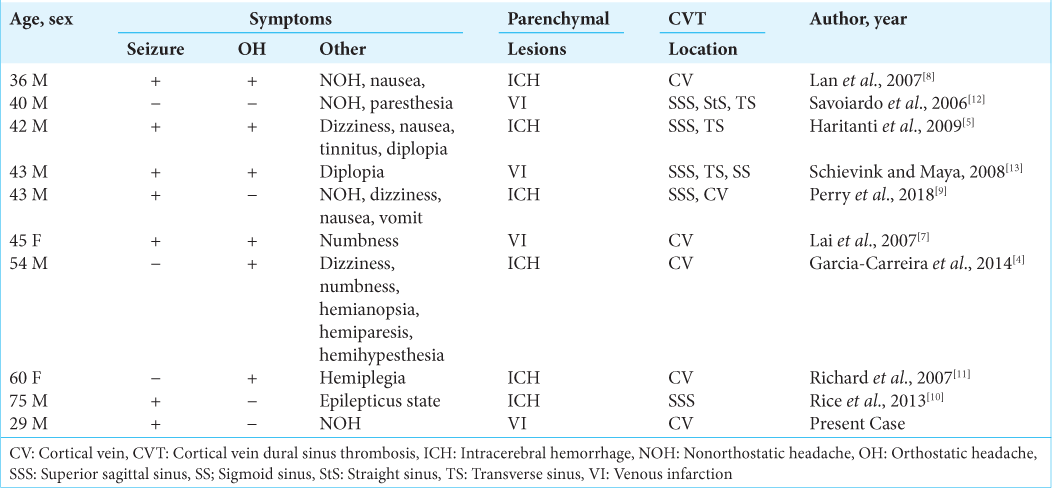
Although it is known that SIH can lead to CVT, CVT is uncommon, and there are only few cases of concurrent cerebral parenchymal lesions. This is because anastomosis develops in the cerebral vein, and the anastomosis portion acts as collateral blood circulation when venous return is impaired. To the best of our knowledge, there have been only nine cases of secondary cerebral parenchymal lesions [
The second clinical issue to bear in mind is that “isolated” cortical venous thrombosis could be complicated by SIH. However, in the past reports, most CVT caused by SIH often has widespread thrombosis mainly in the superior sagittal sinus, transverse sinus, and sigmoid sinuses. In addition, most cases of cortical venous thrombosis were reported to cooccur with superior sagittal sinus thrombosis.[
The third important clinical issue suggested by our case is that the diagnosis of SIH and CVT can be made with craniotomy. To the best of our knowledge, the present case is the first in which low CSF pressure and CVT were confirmed by intraoperative findings, regardless of the imaging findings. In our case, cerebral parenchymal lesion with leptomeningeal enhancement raised suspicion of neoplastic diseases, and open biopsy was performed. Pathological diagnosis was negative for tumors, but intraoperative findings confirmed coexisting low CSF pressure and venous thrombosis. CVT that does not occur with SIH is reported to cause high intracranial pressure levels.[
CONCLUSION
Initial misdiagnosis of CVT following SIH is quite common, especially when the patient presents atypical neurological manifestations and/or atypical image findings. It is important to note that SIH could cause CVT and secondary changes in the brain parenchyma.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ferrante E, Rubino F, Beretta F, Regna-Gladin C, Ferrante MM. Treatment and outcome of subdural hematoma in patients with spontaneous intracranial hypotension: A report of 35 cases. Acta Neurol Belg. 2018. 118: 61-70
2. Ferro JM, Canhão P, Bousser MG, Stam J, Barinagarrementeria F. Early seizures in cerebral vein and dural sinus thrombosis: Risk factors and role of antiepileptics. Stroke. 2008. 39: 1152-8
3. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F. Prognosis of cerebral vein and dural sinus thrombosis: Results of the international study on cerebral vein and Dural sinus thrombosis (ISCVT). Stroke. 2004. 35: 664-70
4. Garcia-Carreira MC, Verge DC, Branera J, Zauner M, Herrero JE, Tio E. Cerebral venous thrombosis in two patients with spontaneous intracranial hypotension. Case Rep Neurol Med. 2014. 2014: 528268
5. Haritanti A, Karacostas D, Drevelengas A, Kanellopoulos V, Paraskevopoulou E, Lefkopoulos A. Spontaneous intracranial hypotension: Clinical and neuroimaging findings in six cases with literature review. Eur J Radiol. 2009. 69: 253-9
6. Kimber J. Cerebral venous sinus thrombosis. QJM. 2002. 95: 137-42
7. Lai PH, Li JY, Lo YK, Wu MT, Liang HL, Chen CK. A case of spontaneous intracranial hypotension complicated by isolated cortical vein thrombosis and cerebral venous infarction. Cephalalgia. 2007. 27: 87-90
8. Lan MY, Chang YY, Liu JS. Delayed cerebral venous thrombosis in a patient with spontaneous intracranial hypotension. Cephalalgia. 2007. 27: 1176-8
9. Perry A, Graffeo CS, Brinjikji W, Copeland WR, Rabinstein AA, Link MJ. Spontaneous occult intracranial hypotension precipitating life-threatening cerebral venous thrombosis: Case report. J Neurosurg Spine. 2018. 28: 669-78
10. Rice CM, Renowden SA, Sandeman DR, Cottrell DA. Spontaneous intracranial hypotension and venous sinus thrombosis. Pract Neurol. 2013. 13: 120-4
11. Richard S, Kremer S, Lacour JC, Vespignani H, Boyer P, Ducrocq X. Cerebral venous thrombosis caused by spontaneous intracranial hypotension: Two cases. Eur J. 2007. 14: 1296-8
12. Savoiardo M, Armenise S, Spagnolo P, de Simone T, Mandelli ML, Marcone A. Dural sinus thrombosis in spontaneous intracranial hypotension: Hypotheses on possible mechanisms. J Neurol. 2006. 253: 1197-202
13. Schievink WI, Maya MM. Cerebral venous thrombosis in spontaneous intracranial hypotension. Headache. 2008. 48: 1511-9
14. Yamamoto A, Hattammaru Y, Uezono S. Spontaneous intracranial hypotension associated with cerebral venous thrombosis detected by a sudden seizure: A case report. JA Clin Rep. 2020. 6: 59
15. Zhang D, Wang J, Zhang Q, He F, Hu X. Cerebral venous thrombosis in spontaneous intracranial hypotension: A report on 4 cases and a review of the literature. Headache. 2018. 58: 1244-55