- Department of Neurology, Cleveland Clinic, Neurological Institute, Cleveland Clinic, Cleveland, Ohio, USA
- Cerebrovascular Center, Neurological Institute, Cleveland Clinic, Cleveland, Ohio, USA
Correspondence Address:
Muhammad S. Hussain
Cerebrovascular Center, Neurological Institute, Cleveland Clinic, Cleveland, Ohio, USA
DOI:10.4103/sni.sni_2_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Tamara A. Strohm, Seby John, Muhammad S. Hussain. Cerebrospinal fluid drainage and blood pressure elevation to treat acute spinal cord infarct. 21-Sep-2018;9:195
How to cite this URL: Tamara A. Strohm, Seby John, Muhammad S. Hussain. Cerebrospinal fluid drainage and blood pressure elevation to treat acute spinal cord infarct. 21-Sep-2018;9:195. Available from: http://surgicalneurologyint.com/?post_type=surgicalint_articles&p=9014
Abstract
Background:Current management of acute spinal cord infarction (SCI) is limited. Lumbar cerebrospinal fluid drainage (CSFD) with blood pressure augmentation is utilized in the thoracic/thoracoabdominal aortic repair and thoracic endovascular aortic repair (TEVAR) populations to increase spinal perfusion pressure.
Case description:We identified 3 patients who sustained acute SCI and underwent CSFD and maintenance of elevated mean arterial pressure (MAP) within 24 hours of injury. The first patient exhibited delayed-onset ischemia after a TEVAR. The second patient presented with an acute type B aortic intramural hematoma. The third patient developed spinal cord ischemia following bronchial artery embolization. There was significant improvement in the motor examination (e.g., ASIA impairment scale grade B or C) to grade D utilizing both blood pressure augmentation and CSFD.
Conclusions:Lumbar CSFD with MAP elevation benefited 3 patients with acute SCI of varying etiologies.
Keywords: Acute stroke therapy, intervention, ischemic stroke, treatment
INTRODUCTION
Lumbar cerebrospinal fluid drainage (CSFD) helps prevent spinal cord injury for patients undergoing open or endoscopic thoracic or thoracoabdominal aortic aneurysm and thoracic endovascular aortic repair (TAA/TAAA/TEVAR) surgery.[
CASE REPORTS
Three patients from 2013 to 2016 who presented with acute SCI underwent the placement of CSFD combined with the elevation of systemic blood pressure within 24 hours of injury. Relevant demographic data and clinical variables were retrospectively collected. We obtained approval from an Ethical Standards Committee.
CASE DESCRIPTION
Case 1
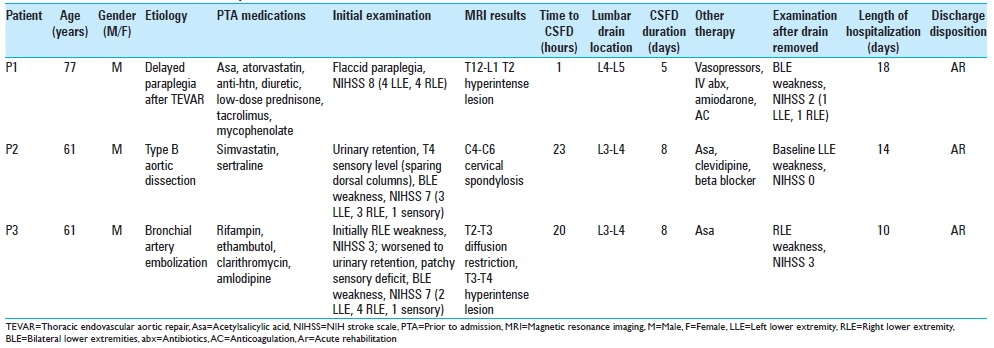
A 77-year-old male with a history of hypertension (HTN), hyperlipidemia (HLD), focal segmental glomerulosclerosis with a kidney transplant, and a 15 pack-year smoking history underwent a TEVAR for TAA. Lumbar CSFD was discontinued after 48 h at which point the neurological examination was normal. Eight days postoperatively, he developed Escherichia coli sepsis with atrial fibrillation/rapid ventricular rate, and acute flaccid paraplegia [
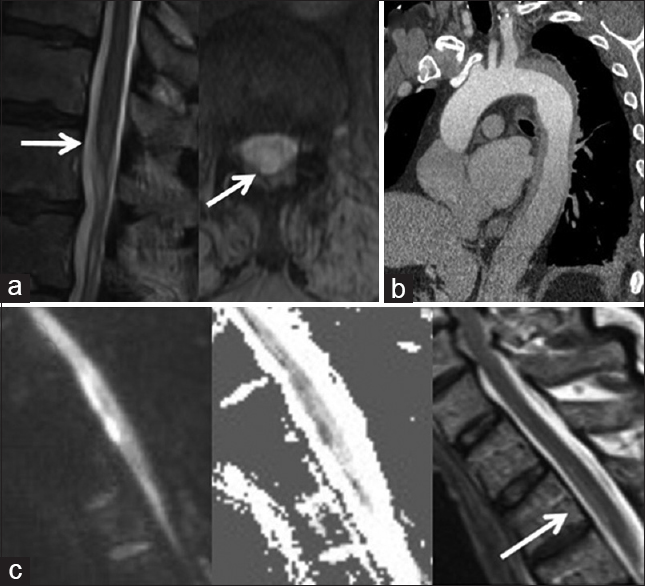
Figure 1
Radiographic findings in acute spinal cord infarction. (a) T2-weighted sagittal and axial MRI of the thoracic spine shows a hyperintense lesion at T12-L1. (b) CT angiogram of the aorta shows an intramural hematoma from the origin of the left subclavian artery to the proximal abdominal aorta. (c) Diffusion-weighted sagittal MRI shows abnormal diffusion restriction at T2-T3 which is confirmed by ADC maps, and is associated with a T2-weighted hyperintense lesion from T2-T4
Case 2
A 61-year-old male with a history of uncontrolled HTN and HLD presented with 6 hours of chest pain, acute bilateral lower extremity weakness, a T4 sensory level, and urinary retention [
Case 3
A 61-year-old male with HTN, diabetes mellitus, and pulmonary Mycobacterium avium intracellulare was admitted for hemoptysis for which he underwent bronchial artery embolization. Immediately following the procedure, he developed acute right lower extremity weakness that exacerbated four days later when he also became hypotensive and tachycardic due to dehydration [
DISCUSSION
For at-risk patients undergoing TAA/TAAA repair or TEVAR, guidelines recommend: (1) elevation of the mean arterial pressure (MAP) from 60 to 90–100 mmHg, and (2) lowering the intrathecal pressure to maintain spinal cord perfusion pressure (MAP – ITP).[
Limitations to this approach include delay to diagnosis, lumbar/cranial (2.9%) hemorrhage in patients with anticoagulation/coagulopathy, infection, and procedure-related complications.[
Here, all three patients improved their AIS grades to D prior to drain removal. In one study, 91% of SCI patients with mild (e.g., ASIA D) impairment achieved ambulation at follow-up.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ackerman LL, Traynelis VC. Treatment of delayed-onset neurological deficit after aortic surgery with lumbar cerebrospinal fluid drainage. Neurosurgery. 2002. 51: 1414-22
2. Blacker DJ, Wijdicks EF, Ramakrishna G. Resolution of severe paraplegia due to aortic dissection after CSF drainage. Neurology. 2003. 61: 142-3
3. Cheung AT, Weiss SJ, McGarvey ML, Stecker MM, Hogan MS, Escherich A. Interventions for reversing delayed-onset postoperative paraplegia after thoracic aortic reconstruction. Ann Thorac Surg. 2002. 74: 413-21
4. Cinà CS, Abouzahr L, Arena GO, Laganà A, Devereaux P, Farrokhyar F. Cerebrospinal fluid drainage to prevent paraplegia during thoracic and thoracoabdominal aortic aneurysm surgery: A systematic review and meta-analysis. J Vasc Surg. 2004. 40: 36-44
5. Coselli JS, LeMaire SA, Köksoy C, Schmittling ZC, Curling PE. Cerebrospinal fluid drainage reduces paraplegia after thoracoabdominal aortic aneurysm repair: Results of a randomized clinical trial. J Vasc Surg. 2002. 35: 631-9
6. Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. J Am Coll Cardiol. 2010. 55: 27-129
7. Lynch K, Oster J, Apetauerova D, Hreib K. Spinal cord stroke: Acute imaging and intervention. Case Rep Neurol Med 2012. 2012. p.
8. Martirosyan NL, Kalani MY, Birchard WD, Baaj AA, Gonzalez LF, Preul MC. Cerebrospinal fluid drainage and induced hypertension improve spinal cord perfusion after acute spinal cord injury in pigs. Neurosurgery. 2015. 76: 461-9
9. Nedeltchev K, Loher TJ, Stepper F, Arnold M, Schroth G, Mattle HP. Long-term outcome of acute spinal cord ischemia syndrome. Stroke. 2004. 35: 560-5
10. Youngblood SC, Tolpin DA, LeMaire SA, Coselli JS, Lee V, Cooper JR. Complications of cerebrospinal fluid drainage after thoracic aortic surgery: A review of 504 patients over 5 years. J Thorac Cardiovasc Surg. 2013. 146: 166-71