- Department of Neurological Surgery, Northwestern University Feinberg School of Medicine, Chicago, Illinois,
- Department of Neurological Surgery, University of Southern California Keck School of Medicine, Los Angeles, California,
- Department of Neurological Surgery, University of California San Francisco, San Francisco, California, United States.
Correspondence Address:
Lee A. Tan, MD, Department of Neurological Surgery, University of California San Francisco, San Francisco, CA, USA, 400 Parnassus Ave, Room 311A, San Francisco, CA 94143,
DOI:10.25259/SNI_599_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nathan A. Shlobin1, Shane Shahrestani2, Saman Shabani3, Nitin Agarwal3, Lee Tan3. Cerebrospinal fluid venous fistula: Illustrative case. 19-Aug-2022;13:374
How to cite this URL: Nathan A. Shlobin1, Shane Shahrestani2, Saman Shabani3, Nitin Agarwal3, Lee Tan3. Cerebrospinal fluid venous fistula: Illustrative case. 19-Aug-2022;13:374. Available from: https://surgicalneurologyint.com/surgicalint-articles/11802/
Abstract
Background: Spinal cerebrospinal fluid (CSF) venous fistulas are an under-recognized cause for spontaneous intracranial hypotension (SIH) which may result in postural headaches.
Case Description: A 60-year-old-male presented with 6 years of a persistent headache. The initial brain and spine MRIs and conventional CT myelogram (CTM) showed no CSF venous fistula. However, the lateral decubitus dynamic CTM demonstrated a hyperdense paraspinal vein on the right at the T10-11 level consistent with a CSF venous fistula. It was subsequently successfully treated with surgical ligation. Temporary CSF diversion with lumbar drain was required to treat transient rebound intracranial hypertension.
Conclusion: The diagnosis of a CSF venous fistulas is often missed on standard brain and spine MRI imaging, and conventional CTM. Dynamic CTM is a more effective modality to detect CSF venous fistulas. Surgical ligation is a safe and effective treatment option. Patients with long-standing SIH may encounter rebound intracranial hypertension after CSF venous fistula ligation and may require temporary CSF diversion.
Keywords: Cerebrospinal fluid leak, CSF leak, CSF venous fistula, CSF-venous fistula, Spontaneous intracranial hypotension
INTRODUCTION
Cerebrospinal fluid (CSF) leaks, variously attributed to dural/nerve root sleeve defects, meningeal diverticuli, tears in the ventral dura, and CSF venous fistulas are etiologies for spontaneous intracranial hypotension (SIH) and positional headaches. As many as, 25% of patients with SIH may have CSF venous fistulas.[
MATERIALS AND METHODS
A 60-year-old male presented with a 6-year history of persistent postural headaches. Initial MR, CT studies, and conventional CTM studies showed no evidence of a CSF leak. The repeated lateral decubitus CTM documented multiple T10/T11 dilated nerve root sleeve cysts but no active leak. The brain MRI obtained 4 years after demonstrated stigmata of SIH (i.e., cerebellar tonsillar herniation, sagging of midbrain, diffuse patchy meningeal thickening and enhancement, venous engorgement of sella, and prominent dural venous sinuses). He underwent two nontargeted epidural blood patches (EBPs). After the EBP, he experienced rebound intracranial hypertension symptoms including headaches were relieved by standing but worsened in the supine position, as well as bilateral papilledema confirmed on fundoscopic examination.
He was treated with a combination of acetazolamide and a short course of dexamethasone with symptom improvement. One month later, he again underwent a dynamic CTM that demonstrated a hyperdense paraspinal vein on the right at the T10-11 level indicative of a focal CSF venous fistula.
Surgery and postoperative course
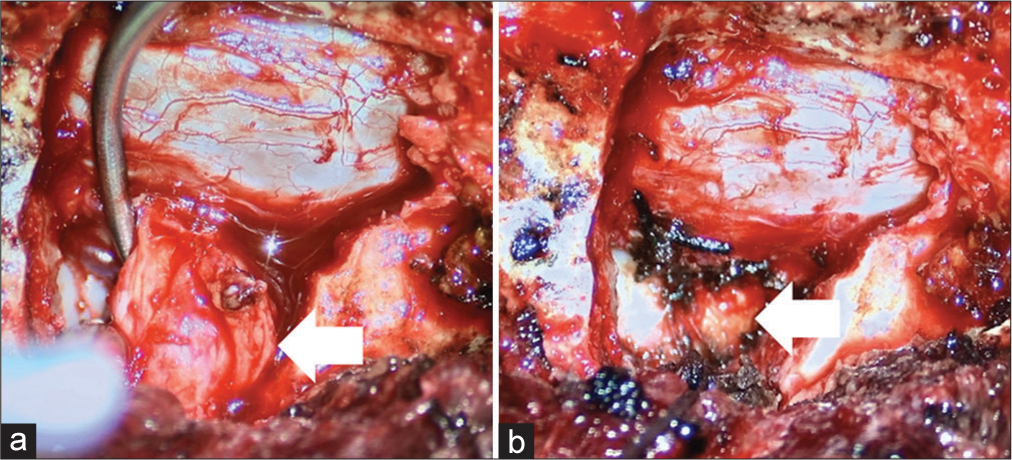
Her underwent a right T10 hemi-laminectomy with complete facetectomy to expose the right T10 nerve root. Dilated epidural veins along with a bulbous nerve root sleeve were clearly visualized. The right T10 nerve root sleeve was temporarily clamped and then fully ligated as there were no changes in neuromonitoring over 10 min [
Figure 1:
Intraoperative photographs demonstrating (a) the cerebrospinal fluid (CSF) venous fistula within the associated bulbous thoracic nerve root and (b) ligation of the CSF venous fistula with associated nerve roots. Arrow is pointing to the location of the CSFvenous fistula in (a), where the CSF-venous fistula was ligated in (b).
DISCUSSION
Diagnosis of CSF venous fistulas
Diagnosis of CSF venous fistula can be challenging; since in most cases, there is no focal extradural CSF collection to indicate the presence of a spinal CSF leak (i.e., on conventional MR and CT) [
Treatment options
Surgical ligation and endovascular embolization are both effective treatment options.[
CONCLUSION
CSF venous fistula is increasingly recognized as a cause for SIH. Dynamic CTM is a more effective modality to detect CSF venous fistulas. Surgical ligation is a safe and effective treatment option. Patients with long-standing SIH may encounter rebound intracranial hypertension after CSF venous fistula ligation and may require temporary CSF diversion.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
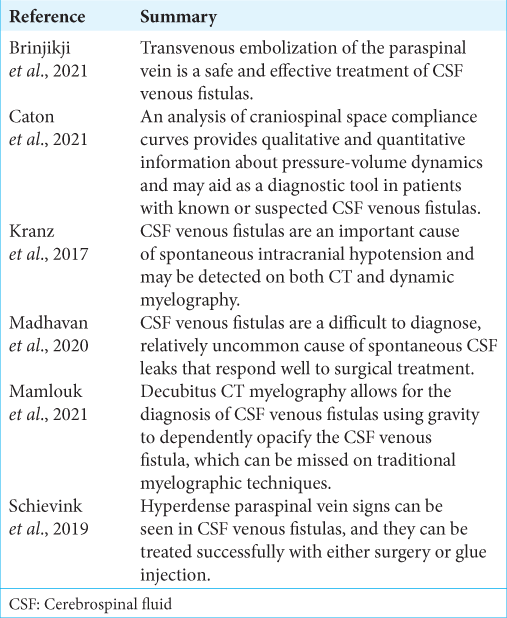
References
1. Brinjikji W, Savastano LE, Atkinson JL, Garza I, Farb R, Cutsforth-Gregory JK. A novel endovascular therapy for CSF hypotension secondary to CSF-venous fistulas. AJNR Am J Neuroradiol. 2021. 42: 882-7
2. Caton MT, Laguna B, Soderlund KA, Dillon WP, Shah VN. Spinal compliance curves: Preliminary experience with a new tool for evaluating suspected CSF venous fistulas on CT myelography in patients with spontaneous intracranial hypotension. AJNR Am J Neuroradiol. 2021. 42: 986-92
3. Kranz PG, Amrhein TJ, Gray L. CSF venous fistulas in spontaneous intracranial hypotension: Imaging characteristics on dynamic and CT myelography. AJR Am J Roentgenol. 2017. 209: 1360-6
4. Madhavan AA, Kim DK, Brinjikji W, Atkinson J, Carr CM. Diagnosis of a cerebrospinal fluid-venous fistula associated with a venous malformation using digital subtraction and computed tomography myelography. World Neurosurg. 2020. 135: 262-6
5. Mamlouk MD, Ochi RP, Jun P, Shen PY. Decubitus CT myelography for CSF-venous fistulas: A procedural approach. AJNR Am J Neuroradiol. 2021. 42: 32-6
6. Schievink WI, Maya MM, Moser FG. False localizing signs of spinal CSF-venous fistulas in spontaneous intracranial hypotension: Report of 2 cases. J Neurosurg Spine. 2019. 31: 764-7