- Department of Neurosurgery,University of Rochester, Strong Memorial Hospital, Rochester, New York, United States.
- Department of Radiology, University of Rochester, Strong Memorial Hospital, Rochester, New York, United States.
Correspondence Address:
Gabrielle Santangelo, Department of Neurosurgery, University of Rochester, Strong Memorial Hospital, Rochester, New York, United States.
DOI:10.25259/SNI_306_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gabrielle Santangelo1, Aman Singh1, Redi Rahmani1, Alexander Kessler2, Matthew Bender1. Cervical extradural arteriovenous fistula with radiculopathy managed endovascularly. 28-Jul-2023;14:265
How to cite this URL: Gabrielle Santangelo1, Aman Singh1, Redi Rahmani1, Alexander Kessler2, Matthew Bender1. Cervical extradural arteriovenous fistula with radiculopathy managed endovascularly. 28-Jul-2023;14:265. Available from: https://surgicalneurologyint.com/surgicalint-articles/12465/
Abstract
Background: Extradural arteriovenous fistulas (AVFs) of the cervical spine are extremely rare, and typically manifest as slowly progressive myelopathy caused by mass effect. This is a unique case of extradural AVF of the cervical spine manifesting with purely radicular symptoms and treated endovascularly with coil and liquid embolization.
Case Description: A 55-year-old woman presented with neck pain and right upper extremity radiculopathy persisting for 9 months. Imaging studies demonstrated an AVF spanning from C4–C6 with extension into the C5–C6 foramen supplied primarily from the deep cervical branch of the costocervical trunk. The patient underwent successful coil and liquid (Onyx) embolization. Six-week postoperatively, the patient’s symptoms completely resolved and magnetic resonance imaging and angiographic imaging confirmed complete obliteration of the fistula.
Conclusion: While extradural AVFs typically present with myelopathic symptoms, they may present with solely radicular symptoms and can be successfully treated endovascularly.
Keywords: Arteriovenous fistula, Cervical, Extradural, Radiculopathy, Therapeutic embolization
INTRODUCTION
Spinal arteriovenous fistula (AVF) is a rare vascular malformation with direct anastomoses between the radicular arteries and the venous plexus of the spine without intervening capillaries.[
CASE REPORT
Preoperative evaluation
A 55-year-old female with no significant medical history was initially evaluated because of the right-sided radiculopathy in a C6 distribution. She complained of constant mild neck pain. Her symptoms had been persistent for approximately 9 months. She had no neurological deficits on physical examination and had no signs of myelopathy. Before evaluation, she had tried physical therapy, acupuncture, oral steroids, chiropractic care, gabapentin, and topical analgesics without relief. In addition, she underwent C7–T1 interlaminar injection of steroids with no change in symptoms.
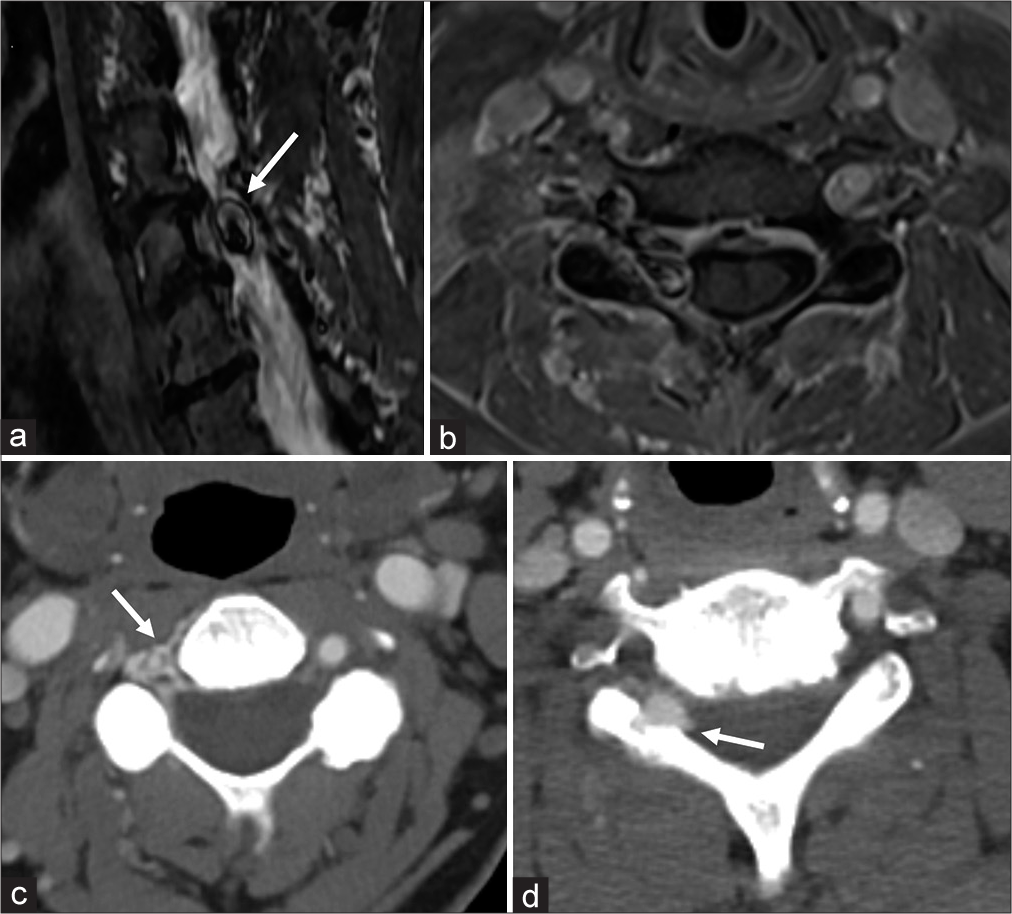
Initial noncontrast computed tomography (CT) image demonstrated a bony destructive process involving the right C5 pedicle and superior facet, concerning for an aggressive neoplastic process. Follow-up contrast-enhanced magnetic resonance imaging (MRI) demonstrated extradural enhancement along the right side at C4–C6, within the right C5–C6 neuroforamen partially insinuating into the bone. Several MRI sequences also demonstrated flow related artifact within the area of extradural enhancement [
Figure 1:
(a) Sagittal short T1 inversion recovery (STIR)magnetic resonance (MR) image demonstrates flow related artifact along the right lateral aspect of the spinal canal at the C5–C6 level producing a lamellated chemical shift appearance (arrow). (b) Axial volumetric T1 fat suppressed post contrast MR image at the level of the C5–C6 foramen demonstrating asymmetric extradural enhancement throughout the right C5–C6 neuroforamen and right lateral epidural space with local mass effect. Flow related artifact is also demonstrated, similar to what was seen on the sagittal STIR. (c) Axial contrast-enhanced computed tomography angiography (CTA) image at the C3–C4 level demonstrates asymmetric enhancement of the venous epidural enhancement surrounding the vertebral artery in the transverse foramen as well as along the right lateral aspect of the spinal canal (arrow). (d) Axial CTA image at the C5–C6 level demonstrates a focal extradural venous pouch, partially insinuating into the adjacent bone (arrow).
At this time, she had been evaluated by an orthopedic surgeon who initially planned C4–C7 anterior cervical discectomy and fusion. However, because the MRI suggested vascular lesion, neurovascular consultation and further imaging studies were instead pursued. CT angiography (CTA) was then obtained demonstrating multilevel asymmetric venous epidural enhancement spanning C4–C6 with a focal extradural venous pouch at the C5–C6 level [
Endovascular angiography and intervention
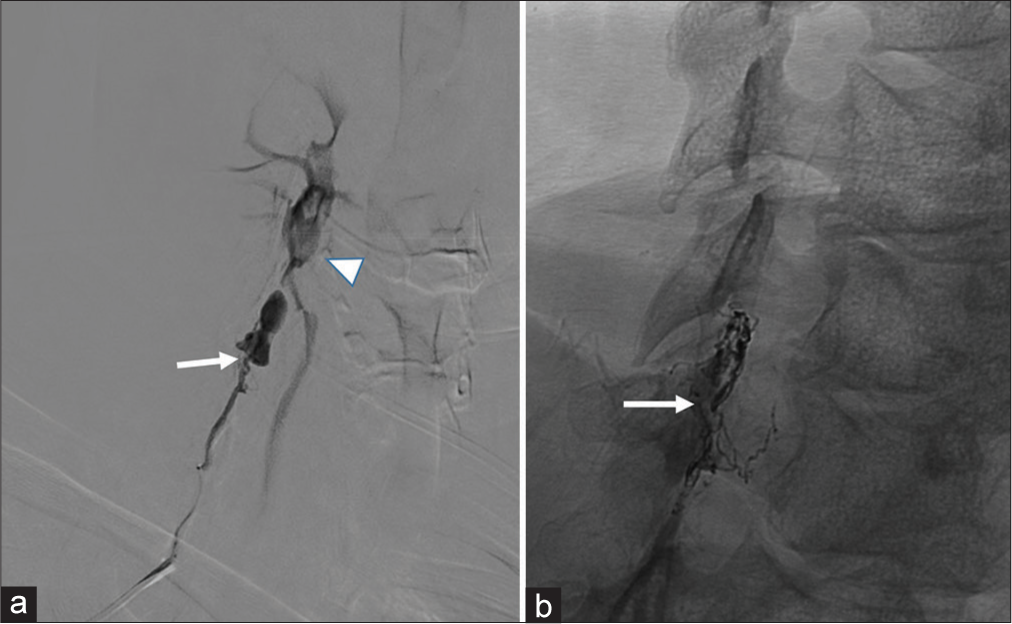
The digital subtraction angiography (DSA) revealed an AVF supplied from the deep cervical branch of the costocervical trunk. There was a smaller contributor from the inferior thyroid branch of the thyrocervical trunk [
One week after DSA, she underwent embolization of the fistula. A transradial approach was used with a Bernstein select catheter and a 256 cm 027 Headway microcatheter. The microcatheter was wedged in the distal most part of the deep cervical branch. A single coil was deployed at the neck of the venous varix (distal to the fistula) to prevent filling densely packing the varix with embolic material and preserving its mass effect. Onyx 18 was then infused upstream of the coil and allowed to disperse throughout the fistulous network in the typical fashion of “lava flow.” At the conclusion of the embolization, the fistula appears completely obliterated [
Figure 2:
(a) Selective catheter angiography of the deep cervical branch of the costocervical trunk. This early/mid arterial phase shows a fistulous point (arrow) leading to two large dilated venous pouches draining early to the deep cervical venous plexus (arrowhead). (b) Native oblique image at the end of treatment showing both coil and onyx cast (arrow). Notice in this mid arterial phase, the fistula and venous pouches are no longer evident.
Postoperative course
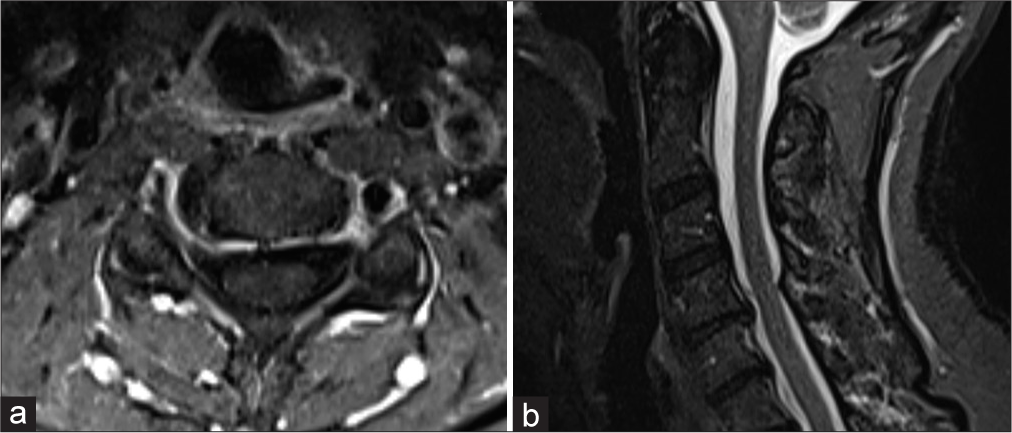
Postoperatively, she was started on a short decadron taper over 5-day course. She was discharged to home the following day having met all expected postoperative milestones. At 1-week postoperatively, she had no change in her radicular pain and remained full strength. She continued to take gabapentin for pain relief but was weaning off. An MRI and CTA were repeated at 6-week postoperatively which demonstrated complete obliteration of the C6 AVF [
DISCUSSION
Spinal AVFs are a rare disease that is direct anastomoses between the radicular arteries and venous plexus of the spine without intervening capillaries.[
Spinal AVFs have undergone several classification schemes since they were first described in the literature in 1967 by Di Chiro et al.[
Management of cervical AVFs has primarily been endovascular with a radiographic goal of complete obliteration of the fistula given the risk of recruitment of new feeding vessels with incomplete treatment. When the embolic material fills the proximal draining vein, the lesion is considered obliterated. A recent case report by Park et al. describes the difficulty in treating Type B fistulas that typically have a large venous pouch with endovascular therapy due to the risk of incomplete obliteration.[
The present case is unique in its extradural and cervical location, the associated presenting symptoms being radicular versus myelopathic, and highlights another viable endovascular approach to these rare lesions. It is of clinical interest for vascular neurosurgeons and interventional radiologists to define these lesions and continue to add to the literature of successful treatment using endovascular approaches. In addition, general neurosurgeons and spine surgeons should also be aware of this clinical entity given that a clinical radiculopathy can indicate an underlying AVF and if imaging findings on CT/MRI suggest asymmetric extradural enhancement with flow related artifact, additional imaging studies are warranted before undertaking any decompressive efforts.
CONCLUSION
We describe a rare case of extradural AVF of the cervical spine, manifesting with purely radicular symptoms, treated with endovascular coil and Onyx embolization. Our case provides evidence of the benefits of endovascular approaches to treating extradural AVFs and highlights the potential for such cases to present with radicular symptoms as opposed to the more commonly seen myelopathic symptoms. This is of significance to both neurosurgeons and orthopedic surgeons, as extradural AVF should be included in the differential diagnosis for patients present with radicular symptoms in their upper or lower extremities.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Asai J, Hayashi T, Fujimoto T, Suzuki R. Exclusively epidural arteriovenous fistula in the cervical spine with spinal cord symptoms: Case report. Neurosurgery. 2001. 48: 1372-5 discussion 1375-6
2. Behzadi F, Heiferman DM, Wozniak A, Africk B, Ballard M, Chazaro J. Comparison of transarterial n-BCA and Onyx embolization of brain arteriovenous malformations: A single-center 18-year retrospective analysis. J Cerebrovasc Endovasc Neurosurg. 2022. 24: 144-53
3. Bao Y, Ling F. Classification and Therapeutic Modalities of Spinal Vascular Malformations in 80 Patients. Neurosurgery. 1997. 40: 75-81
4. Brinjikji W, Colombo E, Lanzino G. Clinical and angioarchitectural characteristics of spinal vascular malformations of the cervical spine. J Neurosurg Spine. 2020. 32: 755-62
5. Brinjikji W, Lanzino G. Endovascular treatment of spinal arteriovenous malformations. Handb Clin Neurol. 2017. 143: 161-74
6. di Chiro G, Doppman J, Ommaya AK. Selective arteriography of arteriovenous aneurysms of spinal cord. Radiology. 1967. 88: 1065-77
7. Kawabori M, Hida K, Yano S, Asano T, Iwasaki Y. Cervical epidural arteriovenous fistula with radiculopathy mimicking cervical spondylosis. Neurol Med Chir (Tokyo). 2009. 49: 108-113
8. Kohno M, Takahashi H, Ide K, Ishijima B, Yamada K, Nemoto S. A cervical dural arteriovenous fistula in a patient presenting with radiculopathy. Case report. J Neurosurg. 1996. 84: 119-23
9. Loh Y, Duckwiler GR. A prospective, multicenter, randomized trial of the Onyx liquid embolic system and N-butyl cyanoacrylate embolization of cerebral arteriovenous malformations. Clinical article. J Neurosurg. 2010. 113: 733-41
10. Park D, Kim D, Kang DH, Lee S, Cho DC. Cervical radiculopathy caused by spinal epidural arteriovenous fistula (SEDAVF) without intradural drainage: A case report and literature review. Korean J Neurotrauma. 2022. 18: 145-9
11. Pirouzmand F, Wallace MC, Willinsky R. Spinal epidural arteriovenous fistula with intramedullary reflux: Case report. J Neurosurg. 1997. 87: 633-5
12. Rangel-Castilla L, Holman PJ, Krishna C, Trask TW, Klucznik RP, Diaz OM. Spinal extradural arteriovenous fistulas: A clinical and radiological description of different types and their novel treatment with Onyx: Clinical article. J Neurosurg Spine. 2011. 15: 541-9
13. Spetzler RF, Detwiler PW, Riina HA, Porter RW. Modified classification of spinal cord vascular lesions. J Neurosurg Spine. 2002. 96: 145-56
14. Takai K, Taniguchi M. Comparative analysis of spinal extradural arteriovenous fistulas with or without intradural venous drainage: A systematic literature review. Neurosurg Focus. 2012. 32: E8
15. Teramoto S, Oishi H, Yoshida K, Yamamoto M, Ohara Y, Arai H. Paravertebral arteriovenous fistula treated by endovascular coil embolization. Neurol Med Chir (Tokyo). 2012. 52: 510-512