- Chief of Neurosurgical Spine and Education, Department of Neurosurgery, Winthrop University Hospital, Mineola, New York – 11501, USA
Correspondence Address:
Nancy E. Epstein
Chief of Neurosurgical Spine and Education, Department of Neurosurgery, Winthrop University Hospital, Mineola, New York – 11501, USA
DOI:10.4103/2152-7806.191078
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Epstein NE. Cervical spine surgery performed in ambulatory surgical centers: Are patients being put at increased risk?. Surg Neurol Int 22-Sep-2016;7:
How to cite this URL: Epstein NE. Cervical spine surgery performed in ambulatory surgical centers: Are patients being put at increased risk?. Surg Neurol Int 22-Sep-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/cervical-spine-surgery-performed-ambulatory-surgical-centers-patients-put-increased-risk/
Abstract
Background:Spine surgeons are being increasingly encouraged to perform cervical operations in outpatient ambulatory surgical centers (ASC). However, some studies/data coming out of these centers are provided by spine surgeons who are part or full owners/shareholders. In Florida, for example, there was a 50% increase in ASC (5349) established between 2000–2007; physicians had a stake (invested) in 83%, and outright owned 43% of ASC. Data regarding “excessive” surgery by ASC surgeon-owners from Idaho followed shortly thereafter.
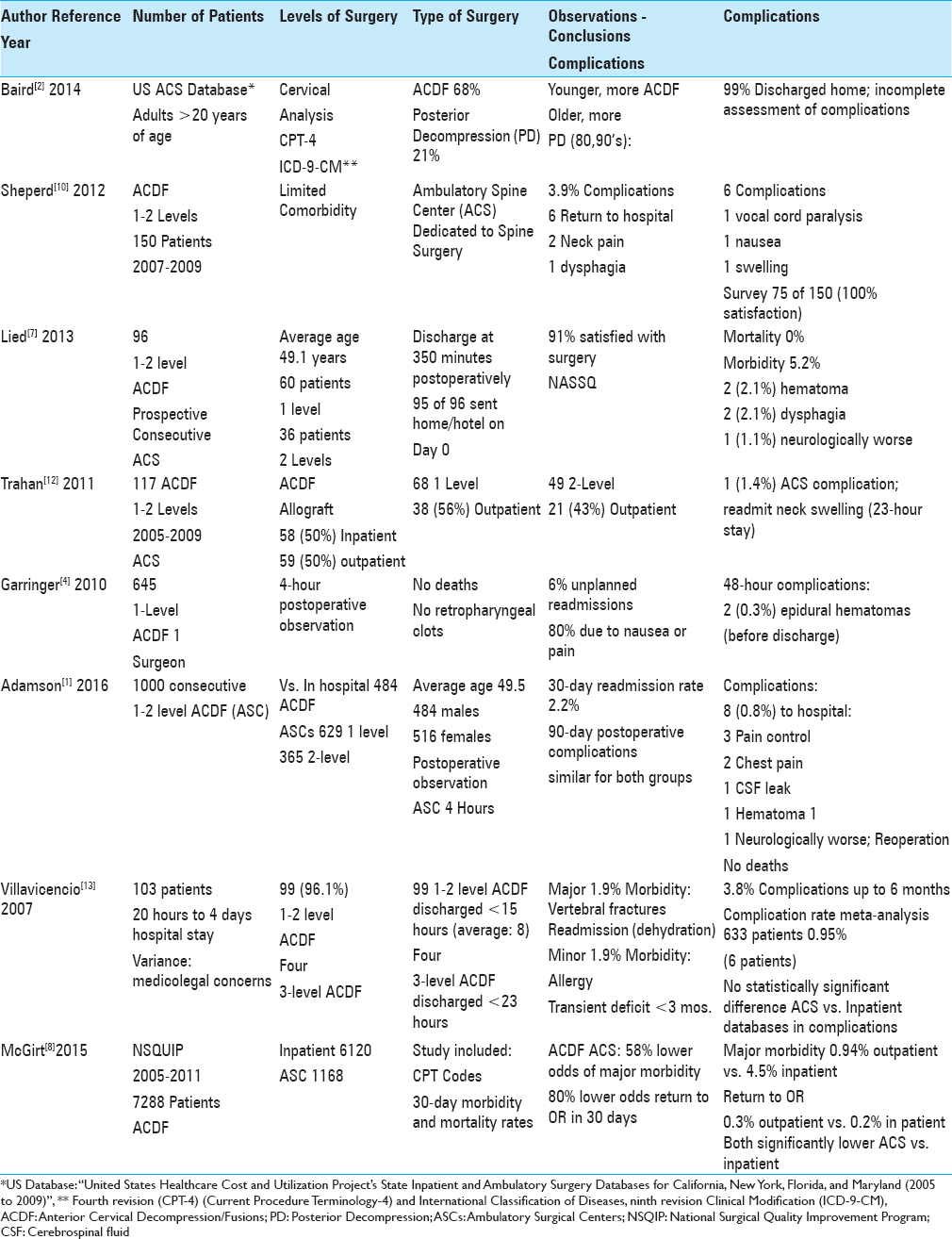
Methods:The risks/complications attributed to 3279 cervical spine operations performed in 6 ASC studies were reviewed. Several studies claimed 99% discharge rates the day of the surgery. They also claimed major complications were “picked up” within the average postoperative observation window (e.g., varying from 4–23 hours), allowing for appropriate treatment without further sequelae.
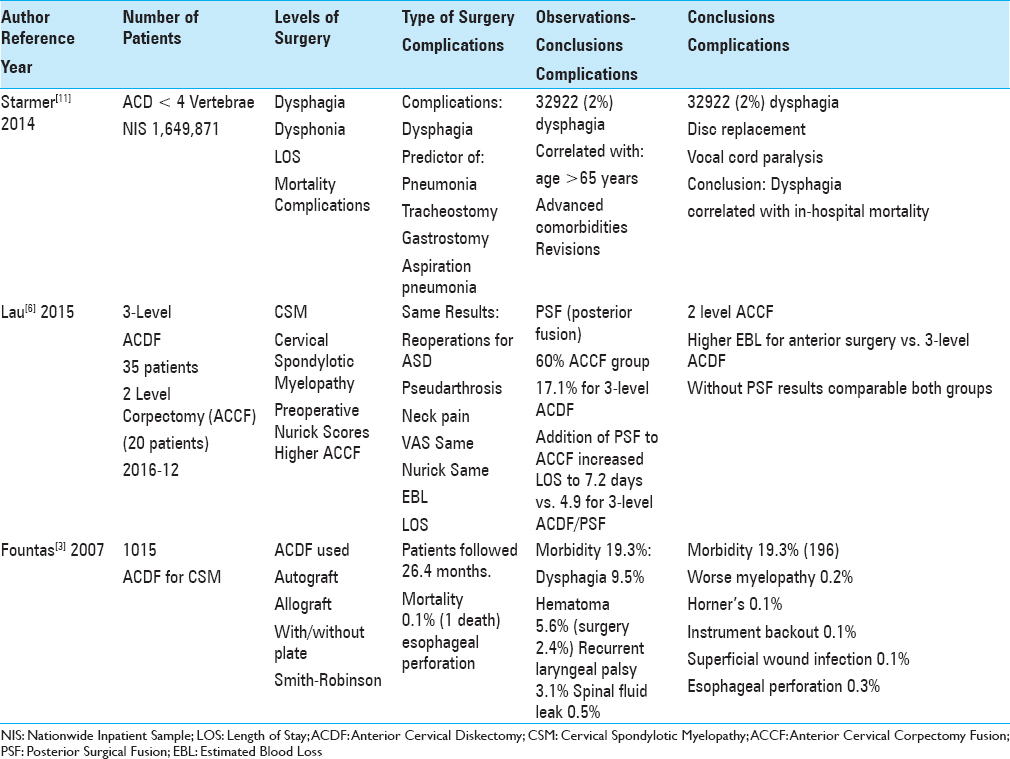
Results:Morbidity rates for outpatient cervical spine ASC studies (e.g. some with conflicts of interest) varied up to 0.8–6%, whereas morbidity rates for 3 inpatient cervical studies ranged up to 19.3%. For both groups, morbidity included postoperative dysphagia, epidural hematomas, neck swelling, vocal cord paralysis, and neurological deterioration.
Conclusions:Although we have no clear documentation as to their safety, “excessive” and progressively complex cervical surgical procedures are increasingly being performed in ASC. Furthermore, we cannot rely upon ASC-based data. At least some demonstrate an inherent conflict of interest and do not veridically report major morbidity/mortality rates for outpatient procedures. For now, cervical spine surgery performed in ASC would appear to be putting patients at increased risk for the benefit of their surgeon-owners.
Keywords: Ambulatory surgical center, cervical spine surgery, complications, increased risks, outpatient
INTRODUCTION
Although there is no clear documentation as to their safety, spine surgeons are increasingly performing more and increasingly complex cervical spine operations in ambulatory surgical centers (ASC). Data from Florida (acquired from 2000–2007, but published in 2010) demonstrated that physicians were invested in 83% of ASCs, and outright owned 43% of these facilities.[
PHYSICIAN OWNERSHIP OF AMBULATORY SURGICAL CENTERS’ RESULTS IN THEIR PERFORMING “EXCESSIVE” OPERATIONS
Multiple studies on outpatient cervical spine surgery point to the “potential cost-savings” of utilizing ASCs (e.g., avoiding hospitalization and the higher hospital facility fee); but cost-savings for whom? The insurance companies pay lower facility fees to ASCs, but those who are part/full owners of ASCs, often spine surgeon themselves with a vested self-interest, are not “saving” anybody anything, but are, rather, financially benefitting. As surgeons’ incomes have decreased across multiple specialties, more have bought into or own ASCs where some now perform “excessive” operations when compared with their nonowner counterparts.[
CERVIVAL SPINE SURGERY IN AMBULATORY SURGICAL CENTER
Between 2007 and 2016, multiple authors concluded that ACDF could be safely performed in outpatient ASCs with lower morbidity rates (e.g., 0.8–6% morbidity; some likely reported by surgeon-owners of ASCs) vs. those reported from inpatient studies (e.g., up to 19.3%, reported by authors without a conflict of interest) [
LARGE-SCALE EVALUATION OF CERVICAL SURGERY IN AMBULATORY SURGICAL CENTERS
Two large database analyses of cervical spine surgery performed in ambulatory surgical centers
In 2014, Baird et al. utilized the “United States Healthcare Cost and Utilization Project's State Inpatient and Ambulatory Surgery Databases for California, New York, Florida, and Maryland (2005 to 2009),” combined with the Current Procedure Terminology fourth revision (CPT-4), and International Classification of Diseases ninth revision Clinical Modification (ICD-9-CM) codes to identify adults (e.g., over the age of 20) undergoing cervical spine procedures in ASCs [
Large clinical series of cervical spine surgery performed in a surgeon-owned ambulatory surgical centers
In 2016, Adamson et al. retrospectively analyzed the safety/efficacy of 1000 consecutive 1 (629 cases; 62.9%) or 2-level (365 cases: 36.5%) ACDF performed in the “authors” ASC (2006 to 2013) vs. 484 comparable ACDF performed inpatient at the Vanderbilt University Hospital [
HOSPITAL-BASED INPATIENT CERVICAL SURGERY STUDIES REPORT HIGHER PERIOPERATIVE MORBIDITY AND MORTALITY
Articles on inpatient cervical spine surgery likely more accurately report perioperative morbidity/mortality as they do not have the “conflict of interest” (e.g., do not own the hospitals) noted for ASC (e.g. at least some of whom have surgeon owners). At least some of whom have surgeon-owners of ASC.[
CONCLUSION
Spine surgeons are performing more frequent and increasingly complex cervical spine operations in ASCs.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adamson T, Godil SS, Mehrlich M, Mendenhall S, Asher AL, McGirt MJ. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: Analysis of 1000 consecutive cases. J Neurosurg Spine. 2016. 24: 878-84
2. Baird EO, Egorova NN, McAnany SJ, Qureshi SA, Hecht AC, Cho SK. National trends in outpatient surgical treatment of degenerative cervical spine disease. Global Spine J. 2014. 4: 143-50
3. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA. Anterior cervical discectomy and fusion associated complications. Spine. 2007. 32: 2310-7
4. Garringer SM, Sasso RC. Safety of anterior cervical discectomy and fusion performed as outpatient surgery. J Spinal Disord Tech. 2010. 23: 439-43
5. Hollingsworth JM, Ye Z, Strope SA, Krein SL, Hollenbeck AT, Hollenbeck BK. Physician-ownership of ambulatory surgery centers linked to higher volume of surgeries. Health Aff. 2010. 29: 683-9
6. Lau D, Chou D, Mummaneni PV. Two-level corpectomy versus three-level discectomy for cervical spondylotic myelopathy: A comparison of perioperative, radiographic, and clinical outcomes. J Neurosurg Spine. 2015. 23: 280-9
7. Lied B, Rønning PA, Halvorsen CM, Ekseth K, Helseth E. Outpatient anterior cervical discectomy and fusion for cervical disk disease: A prospective consecutive series of 96 patients. Acta Neurol Scand. 2013. 127: 31-7
8. McGirt MJ, Godil SS, Asher AL, Parker SL, Devin CJ. Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: Analysis of 7288 patients from the NSQIP database. Neurosurg Focus. 2015. 39: E9-
9. Mitchell JM. Effect of physician ownership of specialty hospitals and ambulatory surgery centers on frequency of use of outpatient orthopedic surgery. Arch Surg. 2010. 145: 732-8
10. Sheperd CS, Young WF. Instrumented outpatient anterior cervical discectomy and fusion: Is it safe?. Int Surg. 2012. 97: 86-9
11. Starmer HM, Riley LH 3 r rd, Hillel AT, Akst LM, Best SR, Gourin CG. Dysphagia, short-term outcomes, and cost of care after anterior cervical disc surgery. Dysphagia. 2014. 29: 68-77
12. Trahan J, Abramova MV, Richter EO, Steck JC. Feasibility of anterior cervical discectomy and fusion as an outpatient procedure. World Neurosurg. 2011. 75: 145-8
13. Villavicencio AT, Pushchak E, Burneikiene S, Thramann JJ. The safety of instrumented outpatient anterior cervical discectomy and fusion. Spine J. 2007. 7: 148-53