- Department of Neurosurgery, University of California Los Angeles (UCLA), Los Angeles, California, United States
- Department of Neurosurgery, University of Texas Southwestern Medical Center, Dallas, Texas, United States
- Department of Neurosurgery, Harbor UCLA Medical Center, Torrance, United States
- Department of Pathology, Harbor UCLA Medical Center, Torrance, United States
- Department of Radiology, Harbor UCLA Medical Center, Torrance, United States
- Department of Pathology, UCLA, Los Angeles, California, United States.
Correspondence Address:
Won Kim, MD, Department of Neurosurgery, UCLA, Los Angeles, CA, USA.
DOI:10.25259/SNI_633_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sophie M. Peeters1, Lauren Uhr1, Srinivas Chivukula2, Duncan McBride1, Richard Everson1, Duc Duong3, Isaac Yang1, Marcia Cornford4, Anton Mlikotic5, William Yong6, Won Kim1. Cervicomedullary junction mature teratoma with pulmonary differentiation and diastematomyelia in an adult – A rare case. 15-Sep-2023;14:334
How to cite this URL: Sophie M. Peeters1, Lauren Uhr1, Srinivas Chivukula2, Duncan McBride1, Richard Everson1, Duc Duong3, Isaac Yang1, Marcia Cornford4, Anton Mlikotic5, William Yong6, Won Kim1. Cervicomedullary junction mature teratoma with pulmonary differentiation and diastematomyelia in an adult – A rare case. 15-Sep-2023;14:334. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12553
Abstract
Background: Intradural extramedullary teratomas in the cervical or cervicomedullary region are rare in adults.
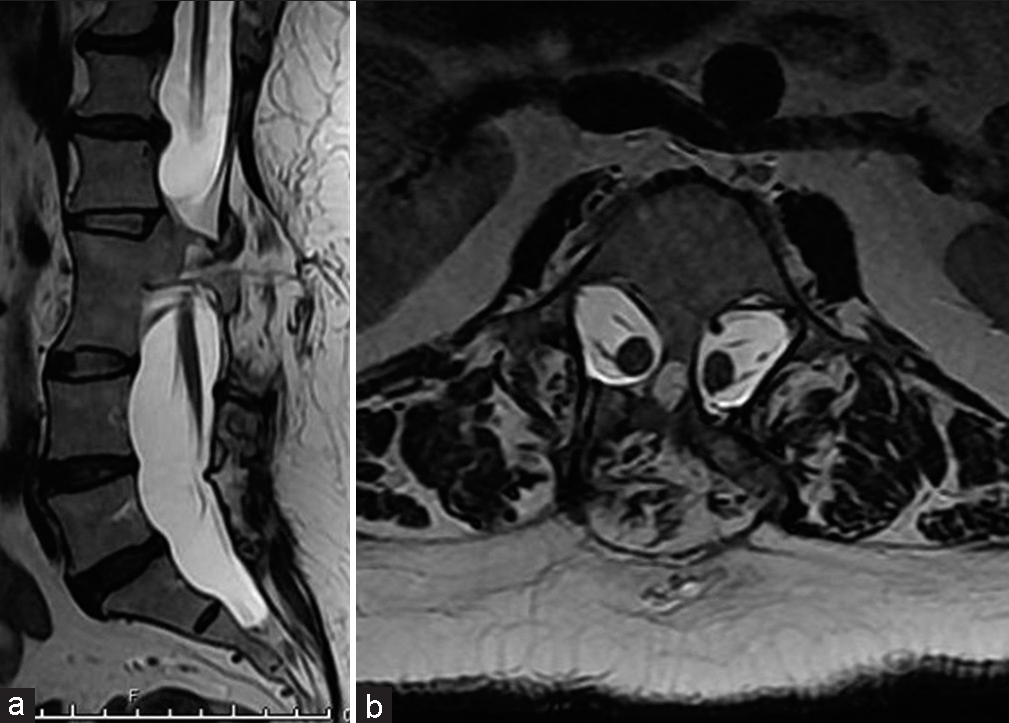
Case Description: We report a symptomatic, mature teratoma at the cervicomedullary junction in a 52-year-old Hispanic female who also has a type I diastematomyelia in the thoracolumbar spine. The patient underwent surgical resection of the lesion with the resolution of presenting symptoms. Histopathology of the lesion revealed a mature cystic teratoma with pulmonary differentiation.
Conclusion: We discuss the case along with a review of pertinent literature and considerations with regard to the diagnosis, etiology, prognosis, and management of this unusual pathology.
Keywords: Cervicomedullary, Diastematomyelia, Mature, Teratoma
INTRODUCTION
Spinal teratomas are rare in adults (i.e., incidence is between 0.2% and 0.5% of all spinal tumors) and typically occur in the thoracolumbar region.[
CASE DESCRIPTION
Clinical presentation
A 52-year-old Hispanic female with a history of type II diabetes mellitus presented with 2 months of occipital headaches, left upper extremity pain, and progressive left hemiparesis. There was no history of recent illnesses, trauma, or an underlying malignancy, but she had undergone posterior cervical surgery for a “mass” in Mexico at age 14. On examination, she demonstrated 4−/5 strength in both the left upper and left lower extremities along with a tender palpable soft-tissue mobile midline mass in the lumbar spine (i.e., consistent with a lipoma), and a well-healed 6 cm posterior transverse incision at the C2 level.
Computed tomography/Magnetic resonance (CT/MR) studies and differential diagnoses
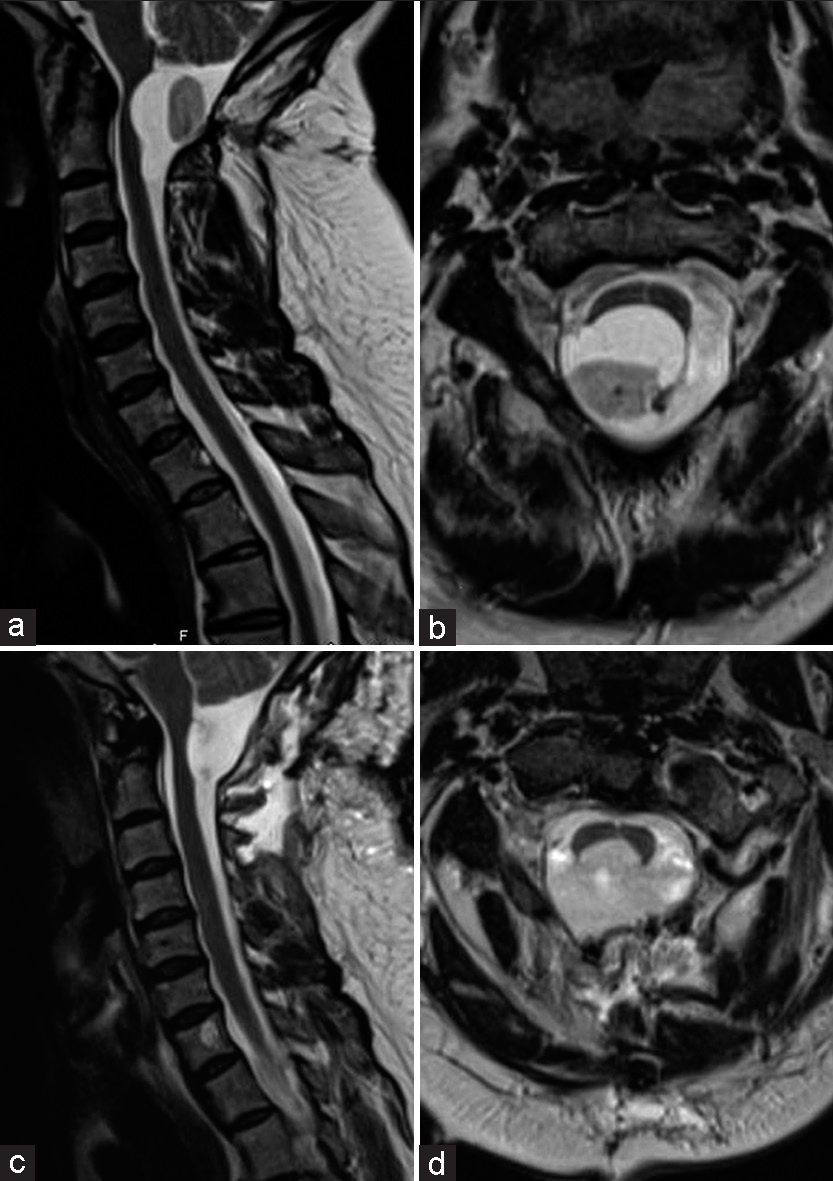
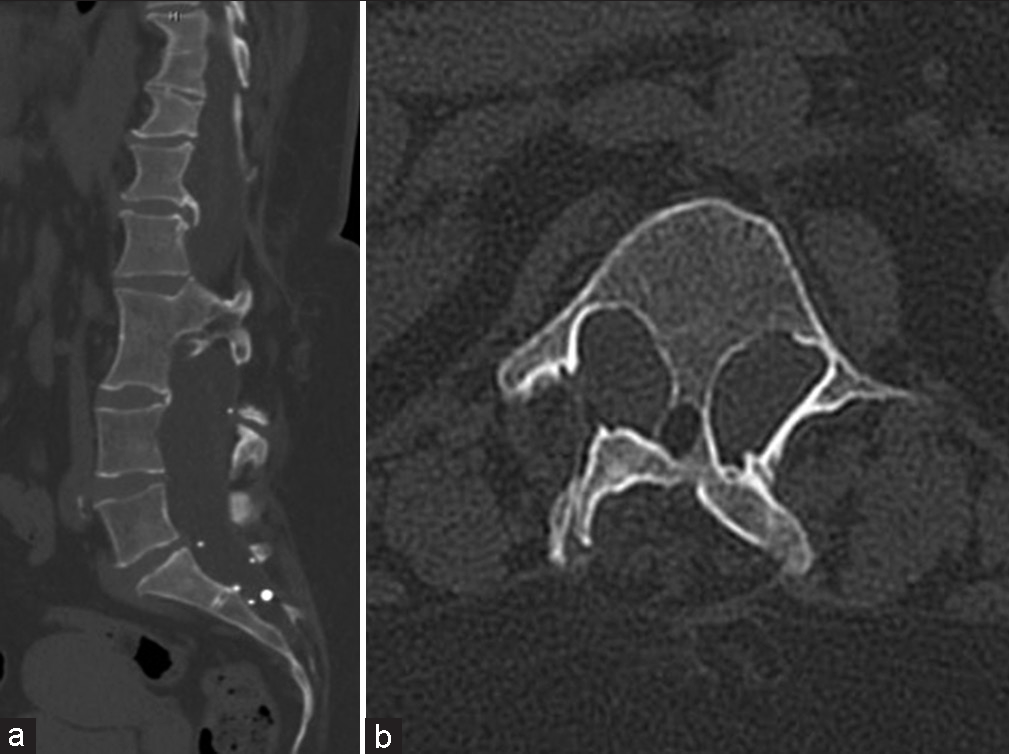
The brain/cervical CT revealed a 2.0 cm lesion at the CMJ. The brain/cervical MR showed an intradural, extramedullary, and posterior mass (2.3 × 2.5 × 2.8 cm) with a cystic component located at the CMJ [
Surgery
A suboccipital craniectomy provided exposure of the cranial/ CMJ allowing for the identification of a plane to expose the tumor [
Pathological diagnosis
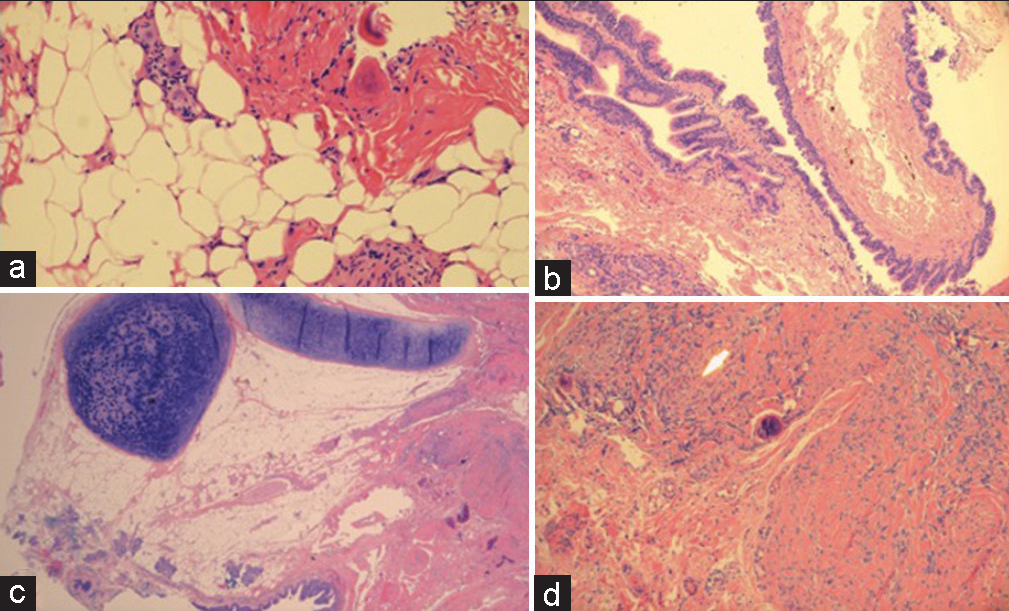
Histopathology of the solid lesion demonstrated a mature teratoma comprised of islands of cartilage, skeletal muscle, adipose tissue, respiratory epithelium, underlying mucous glands, and collagenous septae with rare psammoma bodies [
Video 1
Postoperative outcome and follow-up
The immediate postoperative brain MRI demonstrated significant decompression of the central canal at the C2 level with subtotal resection of the mass [
DISCUSSION
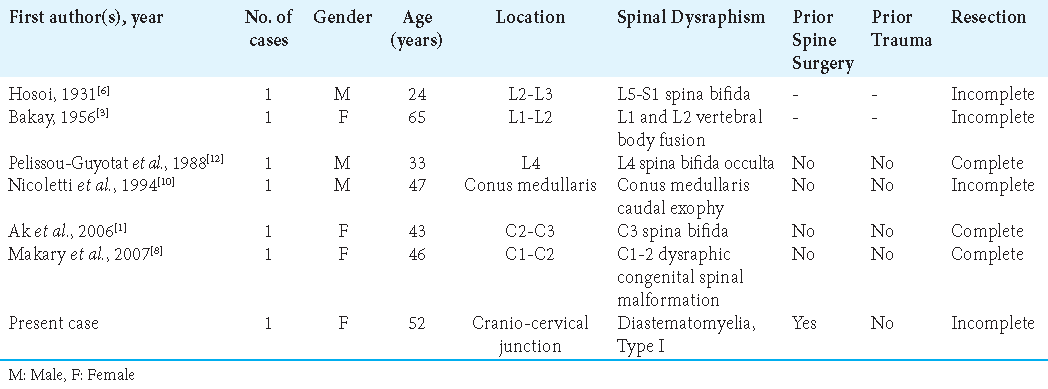
In the pediatric population, intradural teratomas are often associated with a variety of spinal anomalies at the same site, particularly dysraphism. However, in adults, they are most often isolated findings.[
Surgery
Surgical excision of symptomatic lesions remains the first line of treatment, although the recurrence rate of mature spinal teratomas is low, with comparable recurrence rates for gross total (i.e., 9–10%) versus subtotal resection (i.e., 10–11%).[
Lack of efficacy of adjunctive therapies for teratomas
Due to the slow-growing nature of mature teratomas, radiotherapy is typically not considered unless there is a concern for malignancy on histology, while the efficacy of chemotherapy has not been explored.[
CONCLUSION
Intraspinal teratomas in adults are exceedingly rare. Here, we report a 52-year-old Hispanic female who at age 14 had undergone posterior C2 cervical surgery for a “mass,” and now presented with a cervicomedullary intradural extramedullary mature teratoma that was successfully partially resected.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
Videos available on:
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ak H, Ulu MO, Sar M, Albayram S, Aydin S, Uzan M. Adult intramedullary mature teratoma of the spinal cord: Review of the literature illustrated with an unusual example. Acta Neurochir (Wien). 2006. 148: 663-9
2. Allsopp G, Sgouros S, Barber P, Walsh AR. Spinal teratoma: Is there a place for adjuvant treatment? Two cases and a review of the literature. Br J Neurosurg. 2000. 14: 482-8
3. Bakay L. Case reports of the Massachusetts general hospital; weekly clinicopathological exercises: Case 42502. N Engl J Med. 1956. 255: 1153-7
4. Bouaziz M, Haouam K, Laouar O, Lankar A. A case of cervical intradural extramedullary mature cystic teratoma: Diagnosis and management. Neurochirurgie. 2011. 57: 88-91
5. Danison AP, Ramanathan D, Matin M, Kim K, Panchal RR. Adult thoracic intradural exophytic mature teratoma: Case report and literature review. Asian J Neurosurg. 2018. 13: 1182-5
6. Hosoi K. Multiple neurofibromatosis disease. Arch Surg. 1931. 22: 258-81
7. Li Y, Yang B, Song L, Yan D. Mature teratoma of the spinal cord in adults: An unusual case. Oncol Lett. 2013. 6: 942-6
8. Makary R, Wolfson D, Dasilva V, Mohammadi A, Shuja S. Intramedullary mature teratoma of the cervical spinal cord at C1-2 associated with occult spinal dysraphism in an adult. Case report and review of the literature. J Neurosurg Spine. 2007. 6: 579-84
9. Naik V, Mahapatra AK, Gupta C, Suri V. Complex split cord malformation with mediastinal extension of a teratoma and simultaneous ventral and dorsal bony spur splitting the cord. Pediatr Neurosurg. 2010. 46: 368-72
10. Nicoletti GF, Passanisi M, Platania N, Lanzafame S, Albanese V. Intramedullary spinal cystic teratoma of the conus medullaris with caudal exophytic development: Case report. Surg Neurol. 1994. 41: 106-11
11. Prasad GL, Divya S. A comprehensive review of adult onset spinal teratomas: Analysis of factors related to outcomes and recurrences. Eur Spine J. 2020. 29: 221-37
12. Pelissou-Guyotat I, Sindou M, Pialat J, Goutelle A. Apropos of a surgically treated case. Review of the literature. Neurochirurgie. 1988. 34: 205-9 (Article in French)
13. Ramdial PK, Nadvi SS, Mallett R. Cervical spine dysraphism with teratoma exhibiting pulmonary differentiation: Case report and review of the literature. Pediatr Dev Pathol. 1998. 1: 528-33
14. Suri A, Ahmad FU, Mahapatra AK, Mehta VS, Sharma MC, Gupta V. Mediastinal extension of an intradural teratoma in a patient with split cord malformation: Case report and review of literature. Childs Nerv Syst. 2006. 22: 444-9
15. Wan W, Yang C, Yan W, Liu T, Yang X, Song D. Adult-onset intradural spinal teratoma: Report of 18 consecutive cases and outcomes in a single center. Eur Spine J. 2017. 26: 1917-28