- Department of Anesthesiology, Westchester Medical Center, Valhalla, United States
- Department of Orthopaedic Surgery and Sports Medicine, Temple University, Philadelphia, Pennsylvania, United States
- Harvard Combined Orthopaedic Residency Program, Harvard Medical School/Mass General Hospital, Boston, United States
- Department of Orthopaedics, Medstar Orthopaedic Institute/Georgetown University School of Medicine, Washington, United States.
Correspondence Address:
Addisu Mesfin, MD Department of Orthopaedics, Medstar Orthopaedic Institute/ Georgetown University School of Medicine, Washington, United States.
DOI:10.25259/SNI_506_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Aron Sulovari1, Etka Kurucan2, David Nathan Bernstein3, Addisu Mesfin4. Characteristics, comorbidities, and complications in multiple sclerosis (MS) and non-MS patients undergoing lumbar fusion for deformity. 14-Jul-2023;14:247
How to cite this URL: Aron Sulovari1, Etka Kurucan2, David Nathan Bernstein3, Addisu Mesfin4. Characteristics, comorbidities, and complications in multiple sclerosis (MS) and non-MS patients undergoing lumbar fusion for deformity. 14-Jul-2023;14:247. Available from: https://surgicalneurologyint.com/surgicalint-articles/12426/
Abstract
Background: We compared the characteristics, comorbidities, and complications in spinal deformity patients with and without multiple sclerosis (MS) undergoing primary lumbar spine fusion.
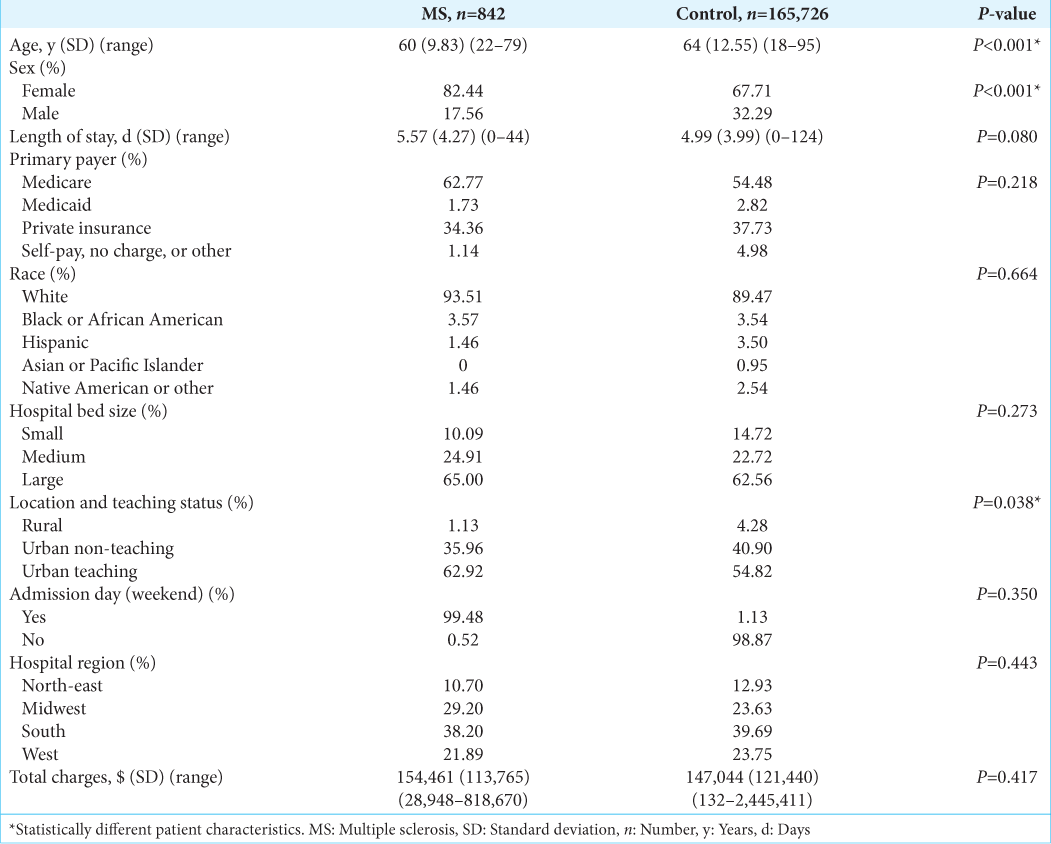
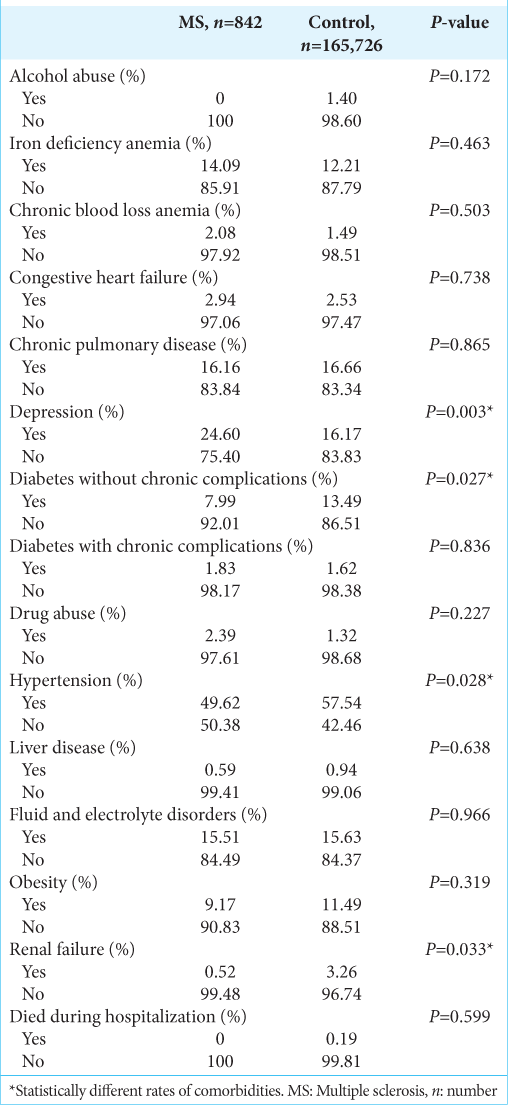
Methods: We used the Nationwide Inpatient Sample (NIS) from 2003 to 2014, International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis and procedure codes to create experimental MS (842 patients) and non-MS control (165,726 patients) cohorts undergoing primary lumbar spine fusion. Characteristics, comorbidities, and complications in spinal deformity patients with and without MS were evaluated using univariate and bivariate analysis.
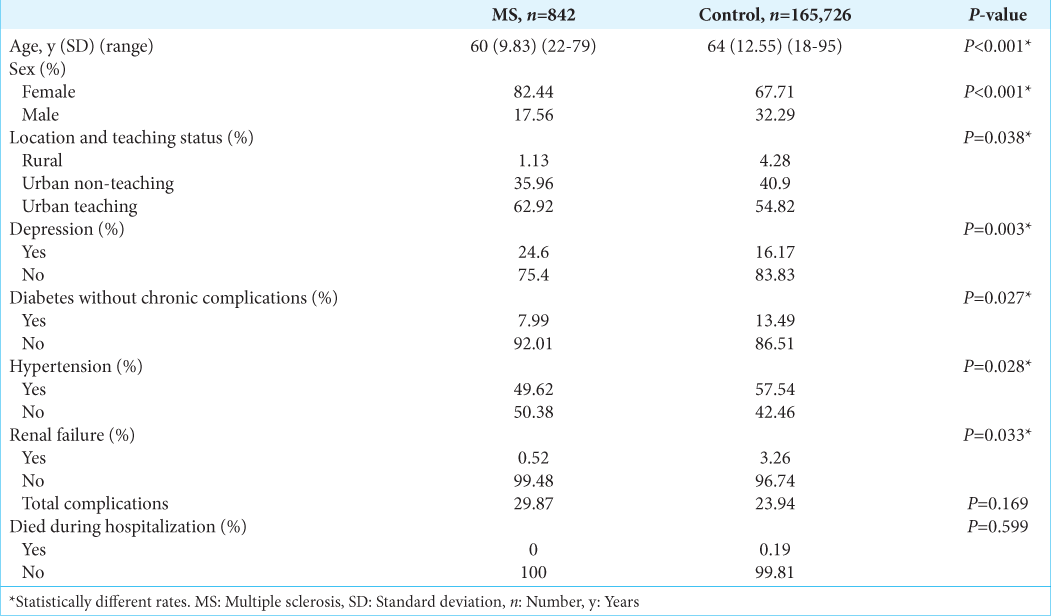
Results: MS spinal deformity patients undergoing primary lumbar spine fusion were younger, more likely to be female and more likely to undergo surgery at urban teaching hospitals. They also exhibited higher rates of depression and lower rates of diabetes without chronic complications, hypertension, and renal failure. However, no significant differences were found in mortality or total perioperative complication rates between MS and nonMS patients.
Conclusion: We found that MS versus non-MS patients undergoing primary lumbar fusion for spinal deformity were younger, more likely to be female and had higher rates of depression but lower rates of diabetes, hypertension, and renal failure. Notably, both groups experienced comparable mortality and perioperative complication rates.
Keywords: Lumbar spine fusion, Multiple sclerosis, Nationwide outcomes, Patient characteristics, Spinal deformity, Surgical complications
INTRODUCTION
Multiple sclerosis (MS) is an autoimmune inflammatory disorder of the central nervous system that is characterized by demyelination and axonal loss. It is the second most common cause of disability in the United States (US), affecting about 400,000 people.[
MATERIALS AND METHODS
Surgical procedure data source
We utilized the Nationwide Inpatient Sample (NIS) database, the largest all-payer database of inpatient admissions in the United States. It contains an approximately 20% stratified sample of discharges from US hospitals, representing around 96% of the population. A total of 34,502 (166,568 weighted) patients meeting the inclusion and exclusion criteria were identified, with 842 weighted in the experimental group with MS and 165,726 weighted in the control group without MS. NIS data are publicly available and de-identified; therefore, the study was exempt from institutional review board approval.
Surgical inclusion and exclusion criteria
Patients ≥18-years-old were included in the study. From 2003 to 2014, the nationwide inpatient sample (NIS) database was queried for multiple International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes for patients undergoing lumbar spine fusion (81.06–81.08); those having revisions (81.30–81.39) were excluded from the study. All patients with MS were included in the experimental group and removed from the non-MS control group for the statistical analysis.
Statistical analysis
National estimates were created for each variable by applying stratified sampling weights. Univariate analysis was conducted to determine patient characteristics as described in
RESULTS
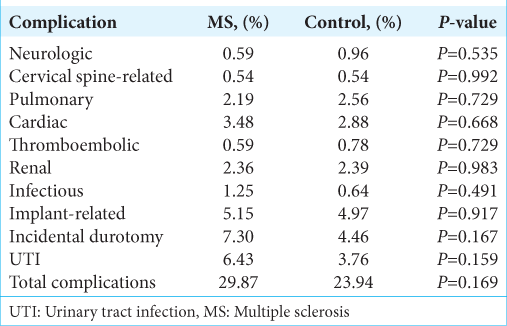
We found that MS patients undergoing lumbar spine fusion were younger, more likely to be female and more likely to have surgery at urban teaching hospitals, had higher rates of depression and lower rates of diabetes without chronic complications, hypertension, and renal failure. There were no significant differences between the MS patients and non-MS control group for other comorbidities including complications and total perioperative complications rate [
DISCUSSION
Our study used the large NIS administrative database to identify patient characteristics and rates of comorbidities and complications in MS spinal deformity patients undergoing primary lumbar spine fusion compared to a non-MS control group. MS patients undergoing primary lumbar spine fusion were younger, more likely to be female and undergo surgery at urban teaching hospitals and had higher rates of depression and lower rates of diabetes without chronic complications, hypertension and renal failure. Nevertheless, postoperative complication rates and mortality were similar for both groups [
Higher rates of depression negatively impact outcomes of lumbar fusion in MS versus non-MS patients undergoing lumbar fusion
Depression was shown to decrease quality of life and impair postoperative rehabilitation in MS patients.[
Comparable complication and mortality rates for MS versus non-MS patients undergoing lumbar fusion
Our MS versus non-MS patients undergoing primary lumbar spine fusion had comparable total complication and mortality rates.
CONCLUSION
Our review of the large NIS database revealed that MS patients undergoing primary lumbar spine fusion were younger, more likely to be female and undergo surgery at urban teaching hospitals and had higher rates of depression and lower rates of diabetes without chronic complications, hypertension, and renal failure versus non-MS patients. Interestingly, both groups demonstrated comparable total complication and mortality rates.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chen AY, Chonghasawat AO, Leadholm KL. Multiple sclerosis: Frequency, cost, and economic burden in the United States. J Clin Neurosci. 2017. 45: 180-6
2. Fominykh V, Shevtsova T, Arzumanian N, Brylev L. Coexistence of multiple sclerosis and ankylosing spondylitis: Report of four cases from Russia and review of the literature. J Clin Neurosci. 2017. 44: 230-3
3. Garg N, Smith TW. An update on immunopathogenesis, diagnosis, and treatment of multiple sclerosis. Brain Behav. 2015. 5: e00362
4. Milinis K, Tennant A, Young CA. Spasticity in multiple sclerosis: Associations with impairments and overall quality of life. Mult Scler Relat Disord. 2016. 5: 34-9
5. Schoell K, Wang C, D’Oro A, Heindel P, Lee L, Wang JC. Depression increases the rates of neurological complications and failed back surgery syndrome in patients undergoing lumbar spine surgery. Clin Spine Surg. 2019. 32: E78-85
6. Stevenson VL, Gras A, Bardos JI, Broughton J. The high cost of spasticity in multiple sclerosis to individuals and society. Mult Scler. 2015. 21: 1583-92
7. Xydis VG, Zikou AK, Kostadima V, Astrakas LG, Kosta P, Argyropoulou MI. The association between multiple sclerosis and spondylosis: When and why. Eur J Radiol. 2017. 91: 47-51