- Department of Neurosurgery, International University of Health and Welfare Mita Hospital, Tokyo, Japan
- Department of Neurosurgery, Mejiro 2nd Hospital, Tokyo, Japan
- Department of Neurosurgery, International University of Health and Welfare, Narita Hospital, Narita City, Japan.
Correspondence Address:
Ichiro Nakazato, Department of Neurosurgery, International University of Health and Welfare Mita Hospital, Tokyo, Japan.
DOI:10.25259/SNI_956_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ichiro Nakazato1, Hideki Tanaka2, Kenichi Oyama1, Keisuke Onoda3, Akira Matsuno3. Chronic epidural hematoma with frontal skull-base destruction mimicking osteogenic tumor, associated with coagulopathy due to chronic hepatitis C. 17-Feb-2023;14:58
How to cite this URL: Ichiro Nakazato1, Hideki Tanaka2, Kenichi Oyama1, Keisuke Onoda3, Akira Matsuno3. Chronic epidural hematoma with frontal skull-base destruction mimicking osteogenic tumor, associated with coagulopathy due to chronic hepatitis C. 17-Feb-2023;14:58. Available from: https://surgicalneurologyint.com/surgicalint-articles/12157/
Abstract
Background: Intracranial epidural hematoma is generally evoked by acute coup-injury. Though rare, it has a chronic clinical course and can be a non-traumatic event.
Case Description: The patient was A thirty-five-year-old man with a complaint of one-year history of hand tremor. He was suspected diagnosis of osteogenic tumor with differential diagnosis of epidural tumor, or abscess in the right frontal skull base bone, associated with chronic type C hepatitis because of his plain CT and MRI.
Results: Results of examinations and surgery, the extradural mass was chronic epidural hematoma without skull fracture. We diagnosis he is the rare case of chronic epidural hematoma caused by coagulopathy due to chronic hepatitis C.
Conclusion: We reported a rare case of chronic epidural hematoma caused by coagulopathy due to chronic hepatitis C. The repeated spontaneous hemorrhage in the epidural space formed the capsule and destruction of skull base bone, just mimicking skull base tumor.
Keywords: Chronic hepatitis C, Coagulopathy, Intracranial chronic epidural hematoma, Skull-base tumor
INTRODUCTION
Intracranial epidural hematoma is generally evoked by acute coup-injury. Although rare, it has a chronic clinical course[
CASE PRESENTATION
A 35-year-old man visited our affiliated hospital with a complaint of 1-year history of hand tremor. He had the right exophthalmos and deviated eye position. Plain craniogram showed the destruction of the upper rim of the right orbit and the right sphenoid wing [
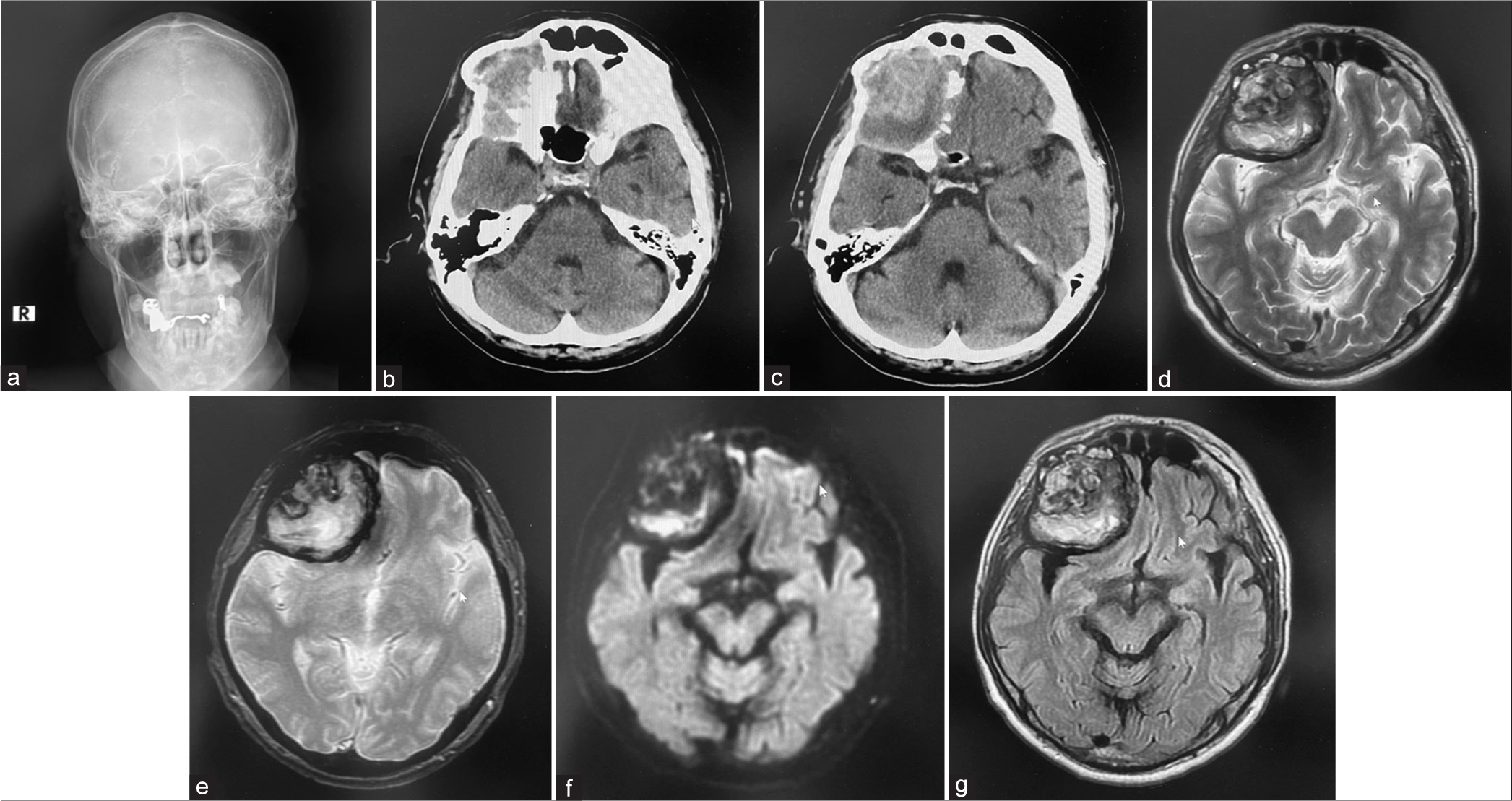
Figure 1:
(a) Plain craniogram showed the destruction of the upper rim of the right orbit and the right sphenoid wing. (b and c) Brain plain CT examined in outpatient clinic revealed the mixed density lesion with partial high density and the right frontal skull-base destruction. (d) Brain plain magnetic resonance imaging (MRI) disclosed well-demarcated tumor-like lesion with heterogeneous mixed intensity in T2-weighted image, (e) Brain plain MRI disclosed well demarcated tumor-like lesion with heterogeneous mixed intensity in peripheral low intensity in T2 star image. (f) Brain plain MRI disclosed well-demarcated tumor-like lesion with heterogeneous mixed intensity partially high intensity in diffusion-weighted image. (g) Brain plain MRI disclosed well-demarcated tumor-like lesion with heterogeneous mixed intensity heterogeneous mixed intensity in fluid-attenuated inversion recovery image.
Hematological examination on admission showed the elevation of serum aspartate aminotransferase 99 IU/L (normal range: 13–33), gamma-glutamyl transpeptidase 360 IU/L (10–47), total bilirubin 3.2 mg/dL (0.2–1.2), direct bilirubin 0.9 mg/dL (0.0–0.6), alanine aminotransferase 25 IU/L (6–30), lowered platelet 77,000/μL (150,000–330,000), elongated prothrombin time (PT) 12.8 s (69.0%), and PT-international ratio 1.30 (0.85–1.15) with activated partial thrombin time 33.7 s. Type C hepatitis virus core protein was 8783.0 fmol/L (<3.0). Serum carcinoembryonic antigen and α-fetoprotein were elevated to 5.9 ng/mL (<5.0) and 20.5 ng/mL (<10.0), respectively.
He was hospitalized under suspected diagnosis of osteogenic tumor with differential diagnosis of epidural tumor, or abscess in the right frontal skull-base bone, associated with chronic type C hepatitis.
The right frontotemporal craniotomy revealed tumor capsule in the epidural space. After cut-opening the tumor capsule, soy pulp-like material was noted and removed extensively. No skull fracture was noted. Bacterial culture was negative, and pathological diagnosis was obsolete hematoma with cholesterol crystals, hemosiderin deposits, granulation tissue, and vascular endothelial proliferation. Neither tumorous tissues nor inflammatory cells were noted. Thus, the extradural mass was diagnosed as chronic epidural hematoma without skull fracture, maybe caused by repeated spontaneous hemorrhage in the epidural space due to coagulopathy induced by chronic hepatitis C. The repeated spontaneous hemorrhage in the epidural space formed the capsule and destruction of skull-base bone, just mimicking skull-base tumor.
DISCUSSION
Chronic epidural hematomas, which are a rare clinical entity as intracranial hematoma, usually occur spontaneously without head trauma. In a literature reviewed of 77 cases of spontaneous epidural hematoma,[
The cause of the chronic accumulation of blood clots in the epidural space is not understood in patients who suffered from coagulopathy. It is known that epidural hematoma can occur even with minor trauma.[
Chronic epidural hematoma usually is encapsulated, as shown the previous reports,[
Noticeable in the present case is that chronic epidural hematoma destroyed the surrounding skull-base bone and radiologically mimicked osteoclastic tumor. Thus, epidural lesion destroying the skull base includes chronic epidural hematoma as differential diagnosis.
CONCLUSION
We reported a rare case of chronic epidural hematoma caused by coagulopathy due to chronic hepatitis C. The repeated spontaneous hemorrhage in the epidural space formed the capsule and destruction of skull-base bone, just mimicking skull-base tumor.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of Interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cordobes F, Lobato RD, Amor T, Lamas E. Epidural haematoma of the posterior fossa with delayed operation. Report of a “chronic” case. Acta Neurochir (Wien). 1980. 53: 275-81
2. Iwakuma T, Brunnbraber CV. Chronic extradural hematomas. A study of 21 cases. J Neurosurg. 1973. 38: 488-93
3. Jackson IJ, Speakman TJ. Chronic extradural hematoma. J Neurosurg. 1950. 7: 444-7
4. Khan KA, Chhabra S, Sharma S, Purohit D. Spontaneous extradural hematoma: A rare entity. Br J Neurosurg. 2020. 34: 86-8
5. Koketsu Y, Tanei T, Kato T, Naito T, Okada K, Ito R. Intracranial idiopathic acute epidural hematoma presenting with a stroke-like attack and rapid neurological deterioration: A case report. NMC Case Rep J. 2022. 9: 25-30
6. Moran SG, McCarthy MC, Uddin DE, Poelstra RJ. Predictors of positive CT scans in the trauma patient with minor head injury. Am Surg. 1994. 60: 533-6
7. Pozzati E, Frank F, Frank G, Gaist G. Subacute and chronic extradural hematomas. A study of 30 cases. J Trauma. 1980. 20: 795-9
8. Rowbotham GF, Whalley N. Prolonged compression of the brain resulting extradural haemorrhage. J Neurol Neurosurg Psychiatry. 1952. 15: 64-5
9. Sparacio RR, Khatib R, Chiu J, Cook AW. Chronic epidural hematoma. J Trauma. 1972. 12: 435-9
10. Zheng FX, Chao Y. Spontaneous intracranial extradural hematoma: Case report and literature review. Neurol India. 2009. 57: 324-6