- Department of Neurosurgery, Kathmandu University, Kathmandu Medical College and Teaching Hospital, Kathmandu, Nepal,
- Department of Neurosurgery, Salford Royal NHS Foundation Trust, Salford, United Kingdom.
Correspondence Address:
Sneha Bisht
Department of Neurosurgery, Salford Royal NHS Foundation Trust, Salford, United Kingdom.
DOI:10.25259/SNI_869_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sneha Bisht1, Raphael Laurente2, K Joshi George2. Circumferential intradural meningioma of the thoracic spine: Case report and literature review. 24-Mar-2021;12:120
How to cite this URL: Sneha Bisht1, Raphael Laurente2, K Joshi George2. Circumferential intradural meningioma of the thoracic spine: Case report and literature review. 24-Mar-2021;12:120. Available from: https://surgicalneurologyint.com/surgicalint-articles/circumferential-intradural-meningioma-of-the-thoracic-spine-case-report-and-literature-review/
Abstract
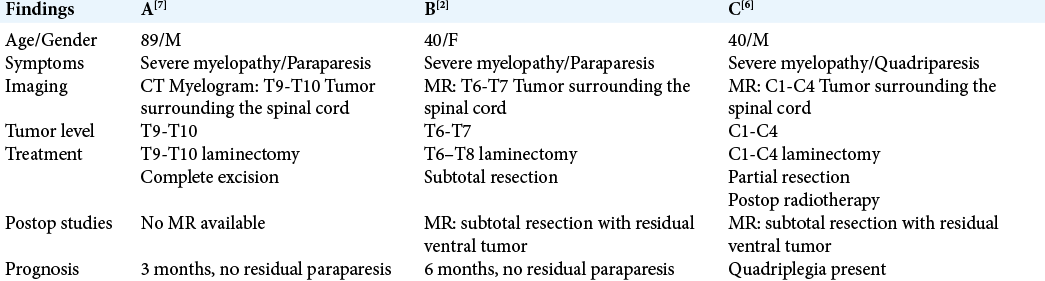
Background: Meningiomas are common intradural extramedullary spinal tumors with a predilection for the thoracic spine. They are mostly benign (90%), with only a few showing malignant potential. However, circumferential intradural meningiomas surrounding the spinal cord are exceptionally rare. Here, we present a 40-year-old patient with a T6-T7 circumferential lesion who underwent surgery. In addition, we reviewed three similar cases previously reported in the literature.
Case Description: A 40-year-old female presented with paraparesis. Imaging demonstrated a T6-T7 thoracic circumferential intradural lesion, considered to most likely be a meningioma. At surgery, the posterolateral portion of the tumor was removed, but there was residual ventral disease. The tumor recurred several years later, and was again partially removed, now leaving her with a residual neurological deficit. Three similar cases of circumferential meningiomas, one cervical and two thoracic, were reported from the literature.
Conclusion: Circumferential meningiomas pose unique and significant surgical challenges, particularly since resection of the posterolateral components is feasible, but some tumor may have to be left ventrally to avoid injury to the anterior spinal artery, that may recur.
Keywords: Circumferential, Excision, Meningioma, Spine, Thoracic
INTRODUCTION
Meningiomas are common intradural extramedullary spinal lesions most often seen in the thoracic spine. Most lesions are benign (90%), and only rarely do they undergo malignant transformation.[
CASE REPORT
Presentation
A 40-year-old female presented with an 18-month history of intermittent pelvic/lower extremity numbness, and 4 months of loss of balance and urinary/fecal incontinence. She was known to have Systemic Lupus Erythematosus and had been maintained on hydroxychloroquine. On neurological examination, she exhibited a sensory level at T10 with clonus and hyperreflexia in both lower extremities.
Diagnostic testing
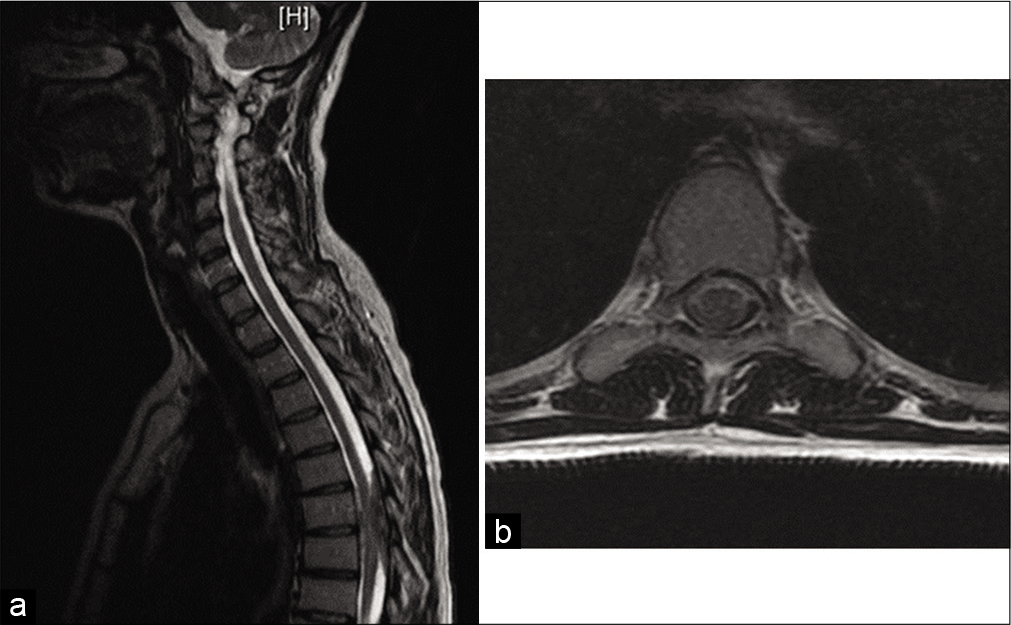
The magnetic resonance imaging (MRI) findings demonstrate an intradural lesion at T6-7 that circumferentially encased the spinal cord [
Intervention done and follow-up
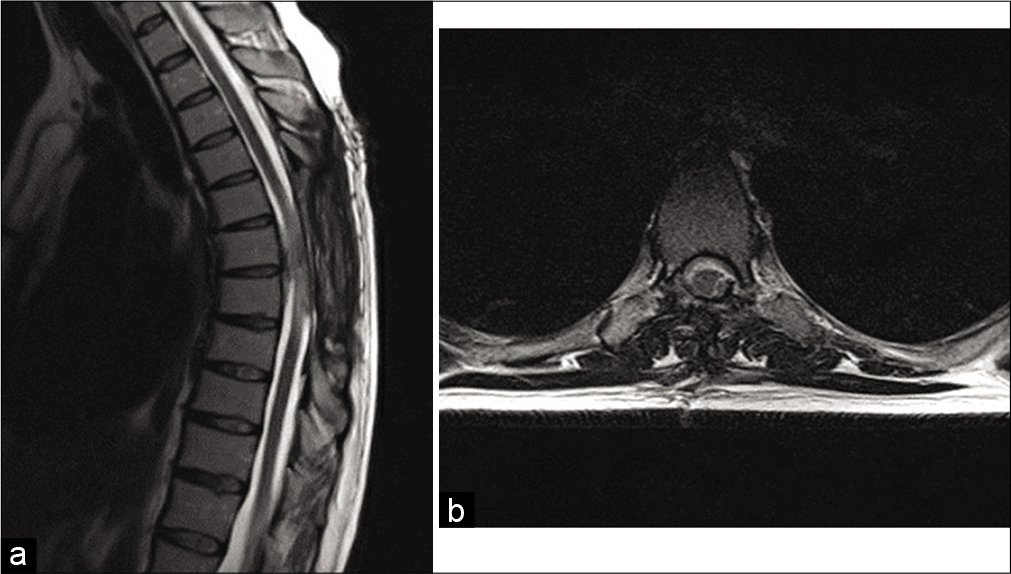
The patient underwent a T6-T8 laminectomy for resection of the intradural lesion. Intraoperative neurophysiology monitoring was used. The tumor was found to be very adherent to the spinal cord. Although the lateral/dorsal segments of tumor were removed, the ventral portion was left behind to protect the anterior spinal artery. The histology confirmed a psammomatous meningioma (WHO Grade I). Postoperative recovery was unremarkable and the patient regained her mobility. Postoperative scans were satisfactory, and the patient was later discharged uneventfully [
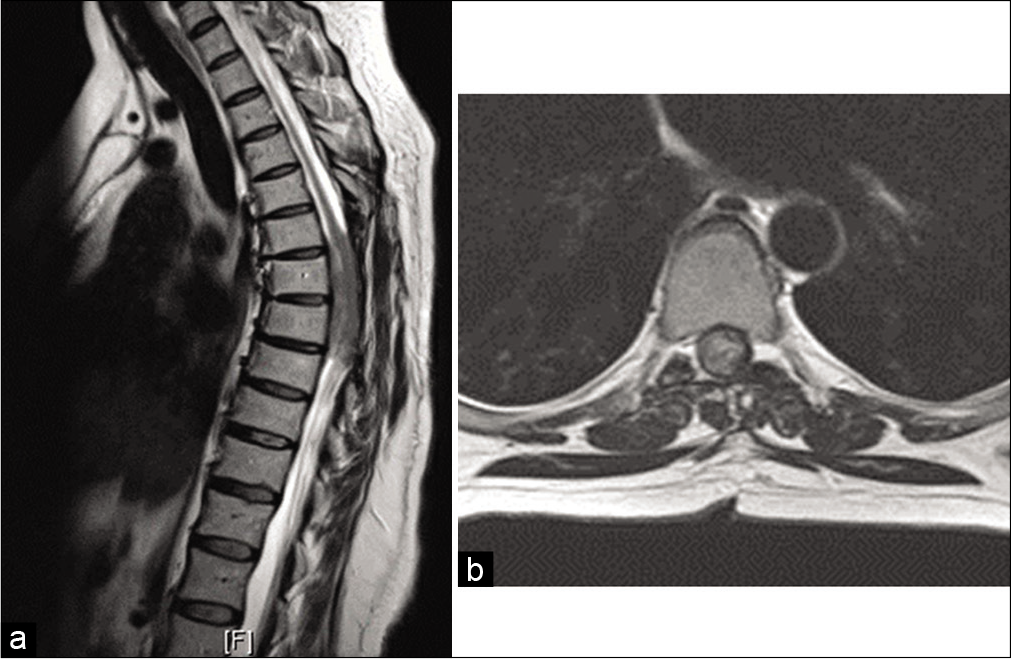
Five years later, the patient again presented with 4 weeks of decreased mobility, worsening balance, and lower limb weakness. She demonstrated a T7 sensory level. The repeat MR scans showed tumor recurrence and cord compression at the T5 to T7 levels, and the tumor was now larger than noted at the initial presentation [
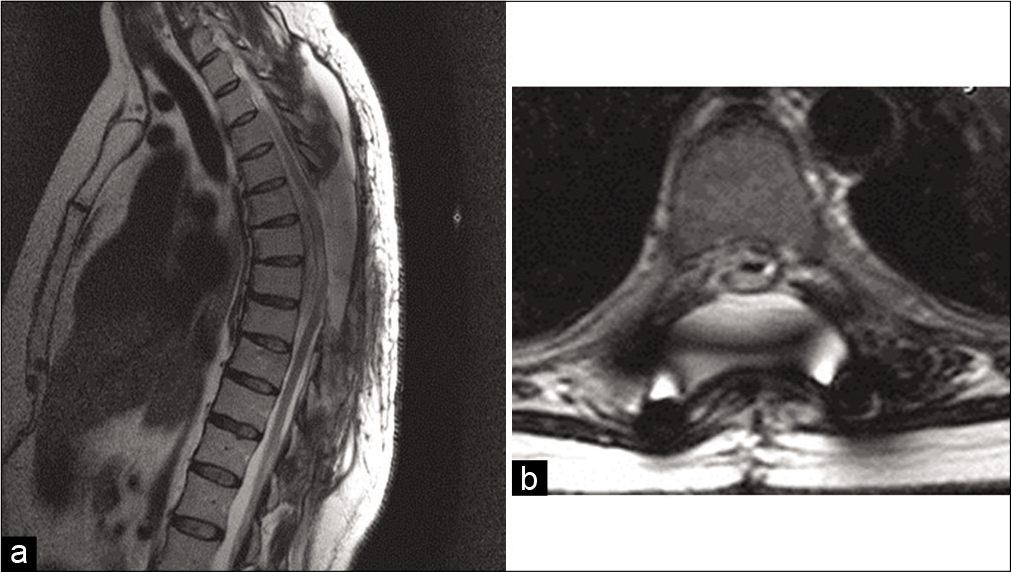
The patient underwent a second surgery for intradural debulking of the tumor, and fusion from T3 to T10 under intraoperative neurophysiological monitoring. The tumor was calcified and adherent to the cord, with only a small soft component being found. The posterior and lateral portions of the tumor were resected, while a small amount of tumor was left ventrally, again to protect the anterior spinal artery. Postoperatively, the patient had paraparesis with proprioceptive loss. After 6 months of neurorehabilitation, she was able to walk with a cane. The postoperative scans showed some residual tumor ventrally, and a small pseudo-meningocele [
DISCUSSION
Meningiomas are the most common primary tumors of the spine and are typically intradural extramedullary in location (100% in 25 patients; study by Gottfried, et al.). Approximately 83–94% are intradural, 5–14% have an extradural component, and 3–9% are completely extradural. They have a predilection for thoracic spine (67–84% thoracic meningiomas; Gottfried et al.).[
Meningiomas are frequently found in middle aged female (female:male ratio between 3 and 4. 2:1; mean age range 49–62 years) and the most common location of tumor in female is thoracic as evidenced in the study by Gottfried et al. and Levy et al., respectively. Most tumors are located posterior/lateral to the spinal cord, with fewer found anteriorly.[
En-Plaque circumferential meningiomas are extremely rare. The posterolateral portions of tumor are typically accessible for resection, while the anterior segment may have to be left behind to avoid damaging the anterior spinal artery. There is a high probability of recurrence with incomplete resection.[
Diagnostic studies and surgery for circumferential meningiomas
MR images with/without contrast, including those for circumferential en plaque lesions, are characteristically hypointense to isointense on T1, and isointense to hyperintense on T2, and homogeneously enhance. Surgery is the mainstay of treatment while lately gamma knife or cyber knife therapy is also recommended with variable success.[
Surgery can be done through the anterior and/or posterior approach. These tumors are typically adherent to the cord which makes surgery technically difficult and risk of spinal cord injury, high. Intraoperative neurophysiology is recommended.
In this patient, the ventral part of tumor was left behind during the first surgery to avoid injury to the anterior spinal artery and limit the potential for neurological injury. As evidenced in the literature, 5 years later, the patient again presented with myelopathy, the repeat MR scans confirmed tumor recurrence with cord compression. Although the posterolateral portion of tumor could again be removed, the ventral portion had to be partially left behind.
CONCLUSION
Circumferential en plaque meningiomas are rare; resection of the ventral tumor is complex and is occasionally avoided to protect the anterior spinal artery. This residual anterior disease typically recurs over a 5-year postoperative interval.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chamberlain MC, Blumenthal DT. Intracranial meningiomas: Diagnosis and treatment. Expert Rev Neurother. 2004. 4: 641-8
2. Foster M, Soh C, DuPlessis D, Karabatsou K. Circumferential intradural meningioma of the thoracic spinal cord. Spine J. 2016. 16: e479-83
3. Gottfried ON, Gluf W, Quinones-Hinojosa A, Kan P, Schmidt MH. Spinal meningiomas: Surgical management and outcome. Neurosurg Focus. 2003. 14: 1-7
4. Harter PN, Braun Y, Plate KH. Classification of meningiomas-advances and controversies. Chin Clin Oncol. 2017. 6: S2
5. Singh BR, Agrawal A. En-plaque meningioma completely encircling the cervical cord: Case report. Iran J Radiol. 2009. 6: 159-61
6. Tsai EC, Butler J, Benzel EC, Lee JH.editors. Spinal Meningiomas. London: Springer; 2009. p. 529-39
7. Vergara P. Is the complete excision of circumferential intradural spinal meningiomas achievable?. Acta Neurochir. 2017. 159: 2385-8