- Department of Neurosurgery, National Institute of Neurology and Neurosurgery, Mexico City, Mexico
- Mexico City Spine Clinic, “Dr. Manuel Dufoo Olvera,” Mexican Social Security Institute, Mexico City, Mexico
- Department of Neurosurgery, Specialties Hospital, La Raza National Medical Center, Mexican Social Security Institute, Mexico City, Mexico.
Correspondence Address:
Martín R. Casas-Martínez, Department of Neurosurgery, National Institute of Neurology and Neurosurgery, Mexico City, Mexico.
DOI:10.25259/SNI_147_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Martín R. Casas-Martínez1, Héctor A. Rodríguez-Rubio1, Alfredo Bonilla-Suastegui1, Rodrigo López-Rodríguez1, Alejandro Serrano-Rubio1, Oscar Josue Montes-Aguilar2, Leonardo Alvarez-Betancourt3, Jonathan Samuel Morgado-Vazquez3. Citrobacter koseri: A rare cause of an epidural spinal abscess. 10-Mar-2023;14:83
How to cite this URL: Martín R. Casas-Martínez1, Héctor A. Rodríguez-Rubio1, Alfredo Bonilla-Suastegui1, Rodrigo López-Rodríguez1, Alejandro Serrano-Rubio1, Oscar Josue Montes-Aguilar2, Leonardo Alvarez-Betancourt3, Jonathan Samuel Morgado-Vazquez3. Citrobacter koseri: A rare cause of an epidural spinal abscess. 10-Mar-2023;14:83. Available from: https://surgicalneurologyint.com/surgicalint-articles/12186/
Abstract
Background: Citrobacter koseri, a Gram-negative organism, rarely causes an epidural spinal abscess.
Case Description: A 50-year-old male presented with mild paraparesis attributed to an magnetic resonance (MR)-documented spinal epidural abscess (SEA) at the T10-level. Following surgical debridement, cultures grew C. koseri, a rare Gram-negative organism. The abscess was subsequently managed with a prolonged course of antibiotics resulting in complete symptom and MR-documented radiological resolution.
Conclusion: A 50-year-old male presented with a T10 SEA attributed to a rare Gram-negative organism, C. koseri. The abscess was appropriately managed with surgical decompression/debridement, followed by prolonged antibiotic therapy.
Keywords: Antimicrobial treatment, Citrobacter koseri, Epidural spinal abscesses, Laminectomy, Spinal infection
INTRODUCTION
A 50-year-old male presented with a mild thoracic paraparesis attributed to an magnetic resonance (MR)-documented T10 epidural abscess. At surgery, the pathology proved to be a rate Gram-negative organism, Citrobacter koseri.[
CASE DESCRIPTION
Presentation and first operative course
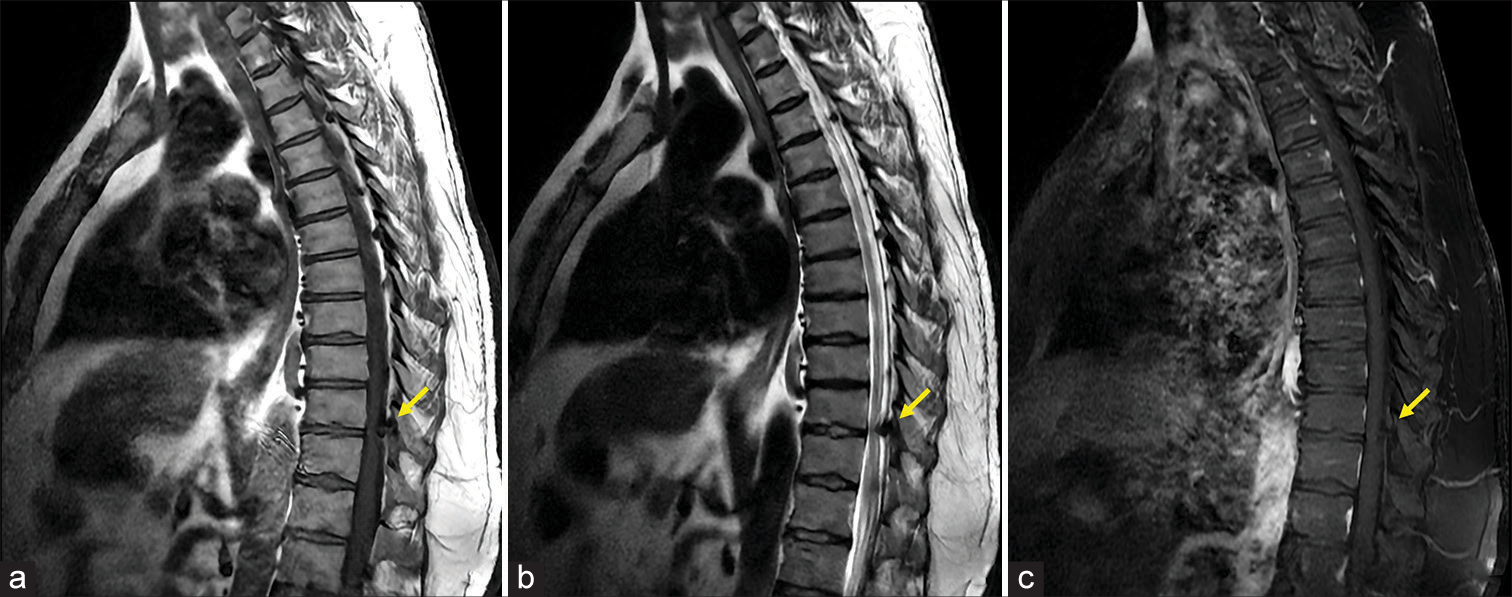
A 50-year-old male with hypertension and diabetes presented with thoracic pain of 4 months duration, and the acute onset of a T10-level paraparesis. The MR documented epidural cord compression at the T10-T11 (compressing cord to the left) and T11-T12 (compressing the cord to the right) levels [
Figure 1:
Preoperative studies, sagittal magnetic resonance imaging. (a and b) T1-weighted and T2-weighted show an epidural hypointense image of triangular appearance (arrow) at the anatomical site of the yellow ligaments at the T10 vertebral level that molds to the dura mater and compresses posterior and lateral left cords. (c) T1-weighted post contrast does not enhance with the contrast material; it is introduced to the left intervertebral foramen (arrow).
Return 7 days later with infection diagnosed as C. koseri
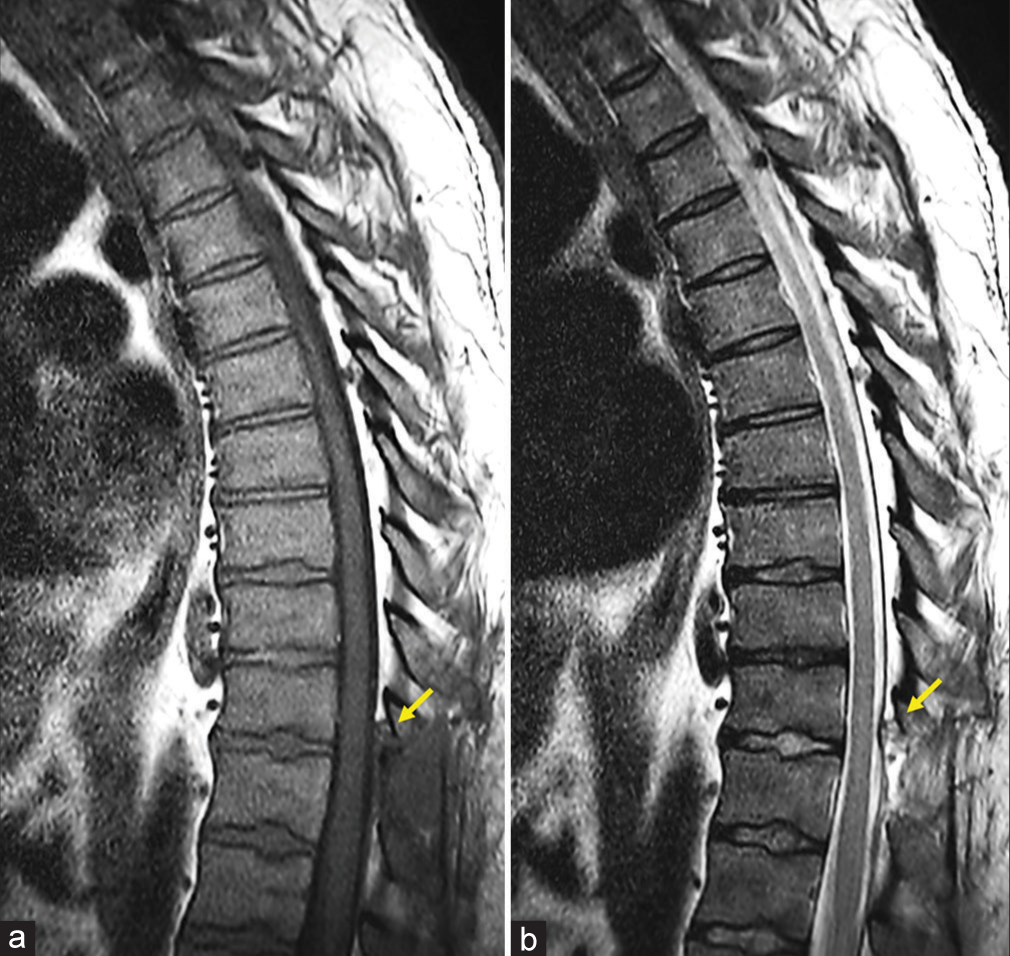
The patient returned 7 days later with a wound infection; once reopened, a brown discharge was cultured. Broad-spectrum antibiotics (AB) (i.e., Ertapenem and Vancomycin) were immediately started; 5 days after the second surgery, cultures from both the first and second surgeries were documented in a rare Gram-negative organism, C. koseri. Within 8 postoperative days, the peripheral white blood cell count and acute phase reactants normalized; then continued, Ciprofloxacin for an additional 2 weeks, along with 4 days of Ertapenem. Six months later, the thoracic magnetic resonance imaging showed complete resolution of the epidural abscess/ wound infection, and the patient fully recovered [
DISCUSSION
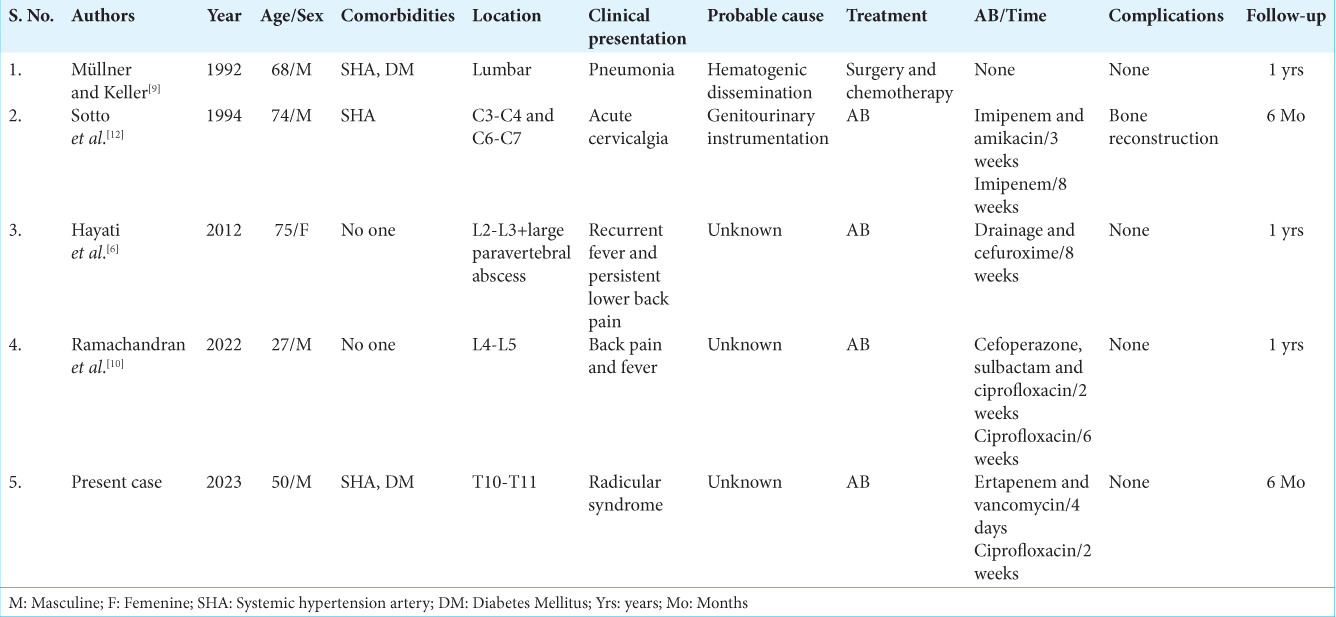
Risk factors for spinal epidural abscesses (SEAs) due to C. koseri
Citrobacter is a nonsporulating, facultatively anaerobic, and Gram-negative bacteria of the Enterobacteriaceae family that was first isolated in 1932 by Werkman and Gillen.[
Treatment of choice for SEA due to C. koseri
The treatment of choice for epidural spinal abscesses in patients with significant neurological deficits is often operative decompression (i.e., laminectomy)/aggressive operative debridement, followed by 4–16 weeks of postoperative intravenous AB.[
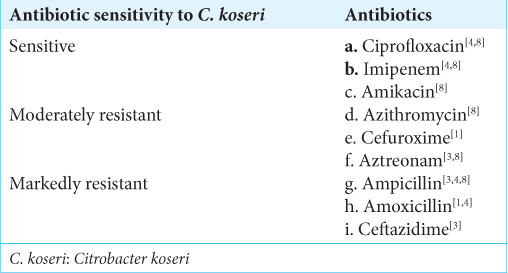
Antibiotic sensitivity of C. koseri
C. koseri is typically sensitive to ciprofloxacin, carbapenems, third-generation cephalosporins, piperacillin-tazobactam, aminoglycosides, and trimethoprim-sulfamethoxazole, but are typically markedly or moderately resistant to multiple other AB [
CONCLUSION
SEA caused by C. koseri is very rare. However, once recognized in conjunction with significant neurological deficits, they typically require surgical decompression/aggressive debridement and prolonged postoperative antibiotic therapy.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Arens S, Verbist L. Differentiation and susceptibility of Citrobacter isolates from patients in a university hospital. Clin Microbiol Infect. 1997. 3: 53-7
2. Canario DG, Remé P, Cunha BA. Citrobacter koseri infection and abscess associated with Harrington rods. Am J Infect Control. 2004. 32: 372-4
3. Céspedes L, Fonseca Y. JMEN-10-00353. J Microbiol Exp. 2022. 10: 54-7
4. Deveci A, Coban AY. Optimum management of Citrobacter koseri infection. Expert Rev Anti Infect Ther. 2014. 12: 1137-42
5. Drelichman V, Band JD. Bacteremias due to Citrobacter diversus and Citrobacter freundii. Incidence, risk factors, and clinical outcome. Arch Intern Med. 1985. 145: 1808-10
6. Hayati SN, Leong CL, Kumar CS, Lee C. Citrobacter koseri bacteraemia complicated by paraspinal abscess and spondylodiscitis--a case report. Med J Malaysia. 2012. 67: 337-9
7. Lee DG, Park KB, Kang DH, Hwang SH, Jung JM, Han JW. A clinical analysis of surgical treatment for spontaneous spinal infection. J Korean Neurosurg Soc. 2007. 42: 317-25
8. Liu L, Zhang L, Zhou H, Yuan M, Hu D, Wang Y. Antimicrobial resistance and molecular characterization of Citrobacter spp. causing extraintestinal infections. Front Cell Infect Microbiol. 2021. 11: 737636
9. Müllner GF, Keller H. Spondylitis due to Citrobacter diversus. Case report and review of Citrobacter diversus infections. Schweiz Med Wochenschr. 1992. 122: 1173-7
10. Ramachandran K, Patel Y, Shetty AP, Shanmuganathan R. Citrobacter koseri as a rare cause of hematogenous pyogenic spondylodiscitis in young adult-a case report. J Orthop Rep. 2022. 1: 51-4
11. Redfern RM, Miles J, Banks AJ, Dervin E. Stabilisation of the infected spine. J Neurol Neurosurg Psychiatry. 1988. 51: 803-7
12. Sotto A, Bernard JC, Brunschwig C, Blin D, Lopez FM, Combe B. Bifocal cervical spondylodiscitis due to Citrobacter diversus. Infection. 1994. 22: 423-4
13. Tellez I, Chrysant GS, Omer I, Dismukes WE. Citrobacter diversus endocarditis. Am J Med Sci. 2000. 320: 408-10
14. Vakili M, Crum-Cianflone NF. Spinal epidural abscess: A series of 101 cases. Am J Med. 2017. 130: 1458-63
15. Werkman CH, Gillen GF. Bacteria producing trimethylene glycol. J Bacteriol. 1932. 23: 167-82