- Trauma Research Center, Shahid Rajaee (Emtiaz) Trauma Hospital, Shiraz University of Medical Sciences, Shiraz, Iran.
Correspondence Address:
Hosseinali Khalili, Trauma Research Center, Shahid Rajaee (Emtiaz) Trauma Hospital, Shiraz University of Medical Sciences, Shiraz, Iran.
DOI:10.25259/SNI_1160_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Omid Yousefi, Pouria Azami, Roham Borazjani, Amin Niakan, Mahnaz Yadollahi, Hosseinali Khalili. Civilian penetrating traumatic brain injury: A 5-year single-center experience. 27-Jan-2023;14:28
How to cite this URL: Omid Yousefi, Pouria Azami, Roham Borazjani, Amin Niakan, Mahnaz Yadollahi, Hosseinali Khalili. Civilian penetrating traumatic brain injury: A 5-year single-center experience. 27-Jan-2023;14:28. Available from: https://surgicalneurologyint.com/surgicalint-articles/12128/
Abstract
Background: The aim of this study was to report the demographics and clinical features of patients with penetrating traumatic brain injury (PTBI) during the past 5 years in Rajaee Hospital, a tertiary referral trauma center in Shiraz, southern Iran.
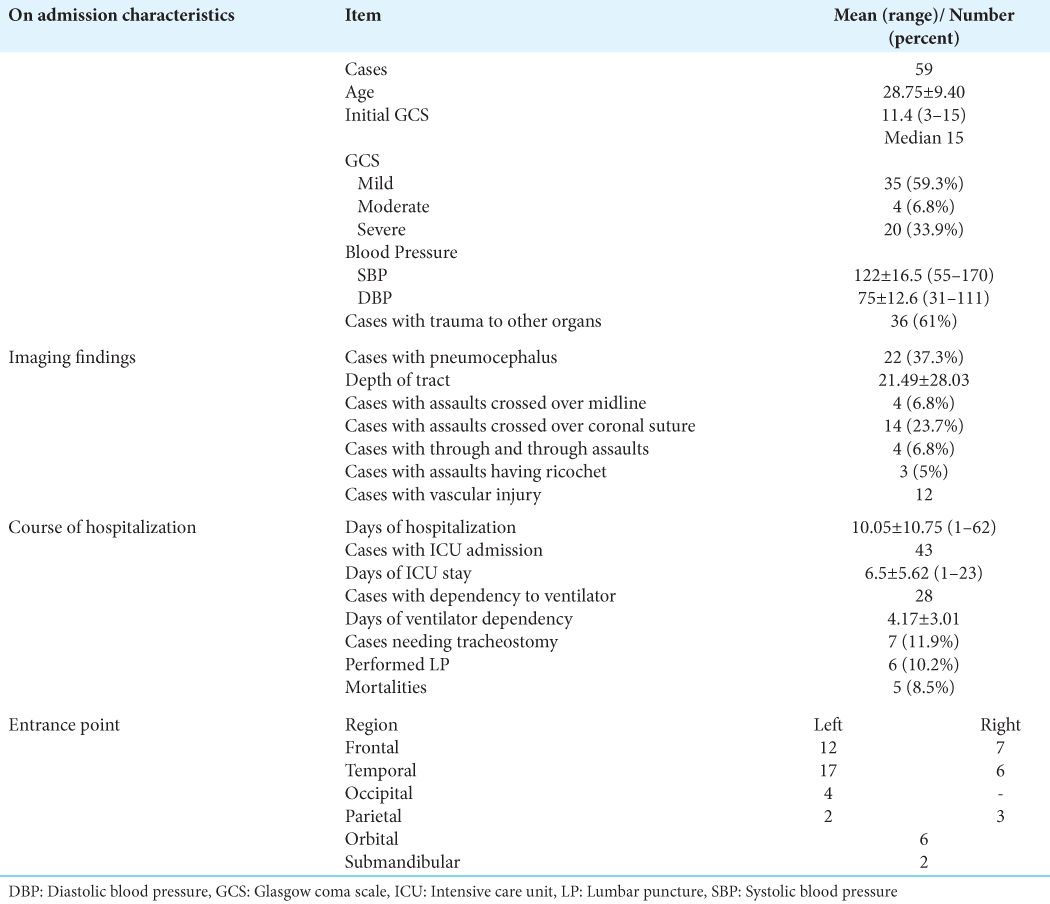
Methods: We conducted a 5-year retrospective evaluation of all patients diagnosed with PTBI who were referred to Rajaee Hospital. We retrieved the following items from the hospital’s database and PACS system: patients’ demographics, on-admission Glasgow Coma Scale (GCS), presence of trauma to other organs, duration of the hospital and ICU stay, the neurosurgical interventions, any necessity of tracheostomy, duration of ventilator dependency, the entrance point of the trauma in the skull, type of assault, length of trajectory in the brain parenchyma, the number of remaining objects in the brain, the occurrence of any hemorrhagic phenomenon, the cross of the bullet from the midline or coronal suture, and the presence of the pneumocephalus.
Results: A total of 59 patients with a mean age of 28.75 ± 9.40 had PTBI over the 5 years. The mortality rate was 8.5%. Stab wounds, shotguns, gunshots, and airguns were the cause of injury in 33 (56%), 14 (23.7%), 10 (17%), and 2 (3.4%) patients, respectively. The median initial GCS of patients was 15 (3–15). Intracranial hemorrhage was observed in 33 cases, subdural hematoma in 18 cases, intraventricular hemorrhage in eight cases, and subarachnoid hemorrhage in four cases. The mean duration of hospitalization was 10.05 ± 10.75 (ranging from 1 to 62 days). Furthermore, 43 patients experienced ICU admission with mean days of 6.5 ± 5.62 (1–23). The temporal and frontal regions were the most common entrance points, in 23 and 19 patients, respectively.
Conclusion: The incidence of PTBI is relatively low in our center, possibly due to the prohibition of possession or using warm weapons in Iran. Further, multicenter studies with larger sample sizes are needed to determine prognostic factors associated with worse clinical outcomes after PTBI.
Keywords: Gunshot, Penetrating traumatic brain injury, Shotgun, Stab wound, Traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI) is considered a leading cause of morbidity and mortality in different societies, like Iran.[
In Iran, like most of the other regions, the most common underlying cause of TBI is transport accidents, in a way that according to the study, held in our center, 6390 potential years of life lost following TBI were recorded in 2013.[
Penetrating TBI (PTBI) represents 0.4–1.5% of all TBI cases, but it is believed to cause the highest rate of mortality among TBI patients (up to 42% of TBI-related mortalities).[
The majority of PTBI reports reflect the war experiences which are mostly caused by high-velocity missiles and there are not many reports about civilian-based PTBIs in the literature.[
The pattern of involvement and piercing objects vary worldwide. In the US, where possession of firearms is not illegal, the annual number of gunshot victims reaches 70/000 cases, which leads up to 30/000 deaths and it is estimated that the target in 14% of all gunshot wounds (GSW) is the brain. It is also believed that the global mortality rate following firearm assaults is increasing.[
There are not many reports on the other etiologies of PTBI, such as the shotgun and stab assaults, as there are on gunshots. As a result, the clinical outcomes following PTBI are not favorable in most reports (because they mostly are about gunshots), in a way that a survival rate of 7–15% has been reported after a gunshot to the brain.[
The aim of the present study is to report the etiology, radiological, and hospitalization characteristics of patients who were admitted to Rajaee Hospital, a tertiary referral trauma center in southern Iran, with the diagnosis of PTBI during the past 5 years.
MATERIALS AND METHODS
All of the patients who were referred to the emergency room of the Rajaee Hospital, a tertiary referral trauma center in Shiraz, southern Iran, with the diagnosis of penetrating brain injury, during the past 5 years were included in the present study.
Patients who passed away before hospital arrival or obtaining brain imaging were excluded from this study. Hospitalization and imaging records of the patients were extracted from the hospital’s database and PACS system. By reviewing the obtained brain CT scans, the entrance point, type of assault, length of trajectory, the number of the remaining objects, the occurrence of any hemorrhagic phenomenon, the cross of the bullet from the midline or coronal suture, and the presence of the pneumocephalus were surveyed. The assessment of the injury to the vessels was also conducted by evaluating the CT angiography of the patients.
The information regarding patients’ demographics, on-admission Glasgow Coma Scale (GCS), presence of trauma to other organs, duration of the hospital and ICU stay, the neurosurgical interventions, any necessity of tracheostomy, and duration of ventilator dependency were also extracted from the hospitalization records of the patients.
The present study has been approved by the ethics committee of Shiraz University of Medical Sciences and informed consent has been obtained from the patients and their families for inclusion in this report.
Hospitalization
Based on the findings of the initial brain CT scan, the decision for further interventions was made. Patients were admitted to the ICU when they had significant intracranial hemorrhage (ICH), severe injury to other organs, and on admission GCS of lower than 10.
In cases with suspicion of vascular injury, a brain CT angiography was also obtained.
Cranioplasty and dural repair were performed when indicated, and the removal of the foreign bodies was also conducted when objects were not located in deep-seated or eloquent areas.
In cases with findings in favor of a midline shift of more than 5 mm or raised intracranial pressure, decompressive craniectomy was performed. Following the surgical intervention, patients were transferred to the ICU and then, once they were stable, to the ward.
RESULTS
Of the 59 patients diagnosed with penetrating brain injury, 65 patients were male, and the overall mean age was 28.75 ± 9.40.
In 10 (17%) patients, the gunshot was the cause of injury, in 14 (23.7%) shotguns, in 33 (56%) stab wounds, and in two patients (3.4%) air guns. All patients affected by firearms, were injured by civilian types, rather than military weapons, and as a result, these types of injuries were considered as low velocity ones.
Thirty-six cases had also injuries to other organs.
The midline cross was observed in four patients, the cross from coronal suture in 14 patients, and the through and through phenomenon in four cases. The mean length of assault trajectory in the brain parenchyma was 21.49 ± 19.3 mm.
ICH was observed in 33 cases, subdural hemorrhage in 18 cases, intraventricular hemorrhage in eight cases, and subarachnoid hemorrhage in four cases. No hemorrhagic phenomenon was observed in 17 cases. The mean volume of the ICH volume was 13.48 ± 14.2.
The severity of the injury was classified regarding the on-admission GCS of the patients, which is as follows: 1. GCS <8 was categorized as severe, 2. GCS score between 9 and 12 as moderate, and 3. A score of higher than 12 as mild TBI.
The details of the patient’s characteristics and imaging findings are provided in [
DISCUSSION
PTBI is defined as an injury to the craniocerebral structures caused by sharp objects with subsequent damage along the trajectory of the piercing insults.[
It is believed that PTBI has worse clinical outcomes than close blunt head trauma. The overall mortality rate has been reported to vary widely from 34% to 92% in different studies.[
The low mortality rate did not let us conduct the prognostic statistical analysis; however, by reviewing the literature, several factors are attributed to this rate.
In our study, the mean age was 28.75 years old which was younger than the reported series from Egypt[
In our study, the majority of patients had mild (59.3%) PTBI followed by severe (33.9%) and moderate (6.8%) PTBI. Among patients with severe TBI, 70% had a missile-related injury and in 77.1% of patients with mild PTBI, non-missiles related injuries were the most frequent mechanism. Presenting GCS is influenced by the mechanism of injury and it consequently does affect the final outcomes.
The reported presenting GCS vary widely in the previous studies. Wu et al. compared the transbase versus transvault low-velocity PTBI and showed that the majority of patients with low-velocity of PTBI had mild GCS on hospital arrival (74.1%).[
The previous studies address several prognostic factors affecting both survival rate and short-to-long-term functional outcomes.[
We have shown that the majority of our patients suffered from a stab wound which is a low-velocity penetrating object. Globally reported, non-missile low-velocity PTBI is a very rare condition. The majority of studies are case reports or series in adult patients and the most frequent causes are occupational, assaults, or self-inflicted.[
The civilian PTBI however differs extensively regarding the epidemiology, the underlying mechanisms, and outcomes between nations. In the US where having gunshot is legal, the majority of assaults are caused by GSW leading to a high-velocity PTBI. In Iran, however, the use of or having a warm weapon is illegal. In contrast to studies from the United States or other regions of the world, the majority of our patients had non-missile and low-velocity stab wounds caused by assault or self-inflicted injuries. PTBI by low-velocity objects causes more localized injuries limited to lacerations or local bleeding along the wound tract. However, gunshots and shotguns are high-velocity (not as high as riffles or ballistic missiles) leading to blast effect and remote damage.[
Shotguns represent a distinct form of ballistic injury due to projectile scatter and variable penetration. Due in part to their rarity, existing literature on shotgun injuries is scarce.[
Two of our patients suffering from low-velocity gunshot-related PTBI died in the hospital. The most frequently used weapon in our country is the handgun. Although injuries caused by handguns, hunting rifles, and other “high-velocity” objects have been well-described, events caused by “low-velocity” objects are particularly uncommon.[
The literature declares that the mortality rate among patients with PTBI is mostly related to missiles’ trajectory. By reviewing 27 patients with low-velocity PTBI (stab), Wu et al. have shown that injuries through the skull base (transbase) increased the risk of injury to nerves and major vessels. although the patients with transvault injuries had lower functional outcome scores.[
CONCLUSION
PTBI outcomes vary in different centers depending on mostly mechanism of injury. Its incidence and the subsequent mortality rate are relatively low in Iran, possibly due to the prohibition of possession or using warm weapons. Further, multicenter surveys with larger sample sizes are warranted to determine the association of on-admission and imaging characteristics, hospitalization course events, and the final clinical outcomes.
Limitations
Having no follow-up data on neurological deficits and chronic phase complication of the patients is regarded as the main limitation of the current study.
The small sample size is the main limitation of this study, which could have an adverse effect on meaningful comparisons between the subsets.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aarabi B, Tofighi B, Kufera JA, Hadley J, Ahn ES, Cooper C. Predictors of outcome in civilian gunshot wounds to the head. J Neurosurg. 2014. 120: 1138-46
2. Ambrosi PB, Valença MM, Azevedo-Filho H. Prognostic factors in civilian gunshot wounds to the head: A series of 110 surgical patients and brief literature review. Neurosurg Rev. 2012. 35: 429-36
3. Borazjani R, Ajdari MR, Niakan A, Yousefi O, Amoozandeh A, Sayadi M. Current status and outcomes of critical traumatic brain injury (GCS= 3-5) in a developing country: A retrospective, registry-based study. World J Surg. 2022. 46: 2335-43
4. Charry JD, Rubiano AM, Puyana JC, Carney N, Adelson PD. Damage control of civilian penetrating brain injuries in environments of low neuro-monitoring resources. Br J Neurosurg. 2016. 30: 235-9
5. D’Agostino R, Kursinskis A, Parikh P, Letarte P, Harmon L, Semon G. Management of penetrating traumatic brain injury: Operative versus non-operative intervention. J Surg Res. 2021. 257: 101-6
6. DeCuypere M, Muhlbauer MS, Boop FA, Klimo P. Pediatric intracranial gunshot wounds: The Memphis experience. J Neurosurg Pediatr. 2016. 17: 595-601
7. Deng H, Yue JK, Winkler EA, Dhall SS, Manley GT, Tarapore PE. Adult firearm-related traumatic brain injury in United States trauma centers. J Neurotrauma. 2019. 36: 322-37
8. Dozier KC, Miranda MA, Kwan RO, Cureton EL, Sadjadi J, Victorino GP. Despite the increasing use of nonoperative management of firearm trauma, shotgun injuries still require aggressive operative management. J Surg Res. 2009. 156: 173-6
9. Finneran MM, Marotta DA, Nardone EM. Nonmissile penetrating head injury with a wooden table leg: An illustrative case. Clin Case Rep. 2021. 9: 2424-8
10. Frösen J, Frisk O, Raj R, Hernesniemi J, Tukiainen E, Barner-Rasmussen I. Outcome and rational management of civilian gunshot injuries to the brain-retrospective analysis of patients treated at the Helsinki University Hospital from 2000 to 2012. Acta Neurochir. 2019. 161: 1285-95
11. Hasar TB, Bir T. Traumatic brain injury due to gunshot wounds: A single institution’s experience with 442 consecutive patients. Turk Neurosurg. 2009. 19: 216-23
12. Joseph B, Aziz H, Pandit V, Kulvatunyou N, O’Keeffe T, Wynne J. Improving survival rates after civilian gunshot wounds to the brain. J Am Coll Surg. 2014. 218: 58-65
13. Kavosi Z, Jafari A, Hatam N, Enaami M. The economic burden of traumatic brain injury due to fatal traffic accidents in shahid rajaei trauma hospital, shiraz, iran. Arch Trauma Res. 2015. 4: e22594
14. Kim HR, Go SJ, Sul YH, Ye JB, Lee JY, Choi JH. Experience of penetrating gunshot wound on head in Korea. J Trauma Injury. 2018. 31: 82-6
15. Li Z, Chen J, Qu X, Duan L, Huang C, Zhang D. Management of a steel bar injury penetrating the head and neck: A case report and review of the literature. World Neurosurg. 2019. 123: 168-73
16. Liu YQ, Zhang QL, Fan XY, Zhang MK, Liu GC. A rare case of craniocervical penetrating injury by a steel bar. J Craniofac Surg. 2022. 33: e365-8
17. Mansour A, Loggini A, El Ammar F, Ginat D, Awad IA, Lazaridis C. Cerebrovascular complications in early survivors of civilian penetrating brain injury. Neurocrit Care. 2021. 34: 918-26
18. Maragkos GA, Papavassiliou E, Stippler M, Filippidis AS. Civilian gunshot wounds to the head: Prognostic factors affecting mortality: Meta-analysis of 1774 patients. J Neurotrauma. 2018. 35: 2605-14
19. Marhold F, Scheichel F, Ladisich B, Pruckner P, Strasser E, Themesl M. Surviving the scene in civilian penetrating brain injury: Injury type, cause and outcome in a consecutive patient series in Austria. Front Surg. 2022. 9: 923949
20. Martins RS, Siqueira MG, Santos MT, Zanon-Collange N, Moraes OJ. Prognostic factors and treatment of penetrating gunshot wounds to the head. Surg Neurol. 2003. 60: 98-104
21. Oearsakul T, Kaewborisutsakul A, Jantharapattana K, Khumtong R, Puetpaiboon A, Sangthong B. Multidisciplinary management of a penetrating cerebellar injury by a fishing speargun: A case study and literature review. Surg Neurol Int. 2021. 12: 391
22. Qazi Z, Ojha B, Chandra A, Singh S, Srivastava C, Verma N. Self inflicted stab with a knife: An unusual mode of penetrating brain injury. Asian J Neurosurg. 2017. 12: 276-8
23. Saatian M, Ahmadpoor J, Mohammadi Y, Mazloumi E. Epidemiology and pattern of traumatic brain injury in a developing country regional trauma center. Bull Emerg Trauma. 2018. 6: 45-53
24. Santiago LA, Oh BC, Dash PK, Holcomb JB, Wade CE. A clinical comparison of penetrating and blunt traumatic brain injuries. Brain Inj. 2012. 26: 107-25
25. Schellenberg M, Inaba K, Heindel P, Forestiere MJ, Clark D, Matsushima K. The diagnostic dilemma of shotgun injuries. Eur J Trauma Emerg Surg. 2020. 46: 1351-6
26. Schellenberg M, Owattanapanich N, Cremonini C, Heindel P, Anderson GA, Clark DH. Shotgun wounds: Nationwide trends in epidemiology, injury patterns, and outcomes from US trauma centers. J Emerg Med. 2020. 58: 719-24
27. Skarupa DJ, Khan M, Hsu A, Madbak FG, Ebler DJ, Yorkgitis B. Trends in civilian penetrating brain injury: A review of 26,871 patients. Am J Surg. 2019. 218: 255-60
28. Sweeney JM, Lebovitz JJ, Eller JL, Coppens JR, Bucholz RD, Abdulrauf SI. Management of nonmissile penetrating brain injuries: A description of three cases and review of the literature. Skull Base Rep. 2011. 1: 39-46
29. Turco L, Cornell DL, Phillips B. Penetrating bihemispheric traumatic brain injury: A collective review of gunshot wounds to the head. World Neurosurg. 2017. 104: 653-9
30. Wahyudi Zaky A, Islam AA, Rosyidi RM. An extremely rare case: Transorbital penetrating intracranial injury by wooden foreign body. Case report. Ann Med Surg. 2021. 71: 102937
31. Wu Y, Chen TG, Chen SM, Zhou L, Yuan M, Wang L. Trans-base and trans-vault low-velocity penetrating brain injury: A retrospective comparative study of characteristics, treatment, and outcomes. Chin J Traumatol. 2021. 24: 273-9
32. Xue H, Zhang WT, Wang GM, Shi L, Zhang YM, Yang HF. Transorbital nonmissile penetrating brain injury: Report of two cases. World J Clin Cases. 2020. 8: 471-8
33. Yousef MS, Attia SM, Ahmed ME, Nabeeh MM. Patterns and outcomes of patients with penetrating head injury. Egypt J Hosp Med. 2022. 87: 1010-6
34. Zyck S, Toshkezi G, Krishnamurthy S, Carter DA, Siddiqui A, Hazama A. Treatment of penetrating nonmissile traumatic brain injury. Case series and review of the literature. World Neurosurg. 2016. 91: 297-307