- Department of Neurosurgery, Johns Hopkins University School of Medicine, Baltimore, MD, USA
- Johns Hopkins Spinal Biomechanics and Surgical Outcomes Laboratory, Baltimore, MD, USA
Correspondence Address:
Ali Bydon
Department of Neurosurgery, Johns Hopkins University School of Medicine, Baltimore, MD, USA
Johns Hopkins Spinal Biomechanics and Surgical Outcomes Laboratory, Baltimore, MD, USA
DOI:10.4103/2152-7806.156578
Copyright: © 2015 Bydon M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Bydon M, Macki M, Abt NB, Sciubba DM, Wolinsky J, Witham TF, Gokaslan ZL, Bydon A. Clinical and surgical outcomes after lumbar laminectomy: An analysis of 500 patients. Surg Neurol Int 07-May-2015;6:
How to cite this URL: Bydon M, Macki M, Abt NB, Sciubba DM, Wolinsky J, Witham TF, Gokaslan ZL, Bydon A. Clinical and surgical outcomes after lumbar laminectomy: An analysis of 500 patients. Surg Neurol Int 07-May-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/clinical-surgical-outcomes-lumbar-laminectomy/
Abstract
Background:The objective of this study is to determine the clinical and surgical outcomes following lumbar laminectomy.
Methods:We retrospectively reviewed medical records of neurosurgical patients who underwent first-time, bilateral, 1-3 level laminectomies for degenerative lumbar disease. Patients with discectomy, complete facetectomy, and fusion were excluded.
Results:Five hundred patients were followed for an average of 46.79 months. Following lumbar laminectomy, patients experienced statistically significant improvement in back pain, neurogenic claudication, radiculopathy, weakness, and sensory deficits. The rate of intraoperative durotomy was 10.00%; however, 1.60% experienced a postoperative cerebrospinal fluid leak. The risk of experiencing at least one postoperative complication with a lumbar laminectomy was 5.60%. Seventy-two patients (14.40%) required reoperations for progression of degenerative disease over a mean of 3.40 years. The most common symptoms prior to reoperation included back pain (54.17%), radiculopathy (47.22%), weakness (18.06%), sensory deficit (15.28%), and neurogenic claudication (19.44%). The relative risk of reoperation for patients with postoperative back pain was 6.14 times higher than those without postoperative back pain (P
Conclusion:Patients experienced statistically significant improvements in back pain, neurogenic claudication, radiculopathy, motor weakness, and sensory deficit following lumbar laminectomy. Incidental durotomy rate was 10.00%. Following a first-time laminectomy, the reoperation rate was 14.4% over a mean of 3.40 years.
Keywords: Fusion, laminectomy, lumbar, outcomes, reoperation, spine
INTRODUCTION
Lumbar laminectomy continues to be one of the most common lumbar procedures performed for spinal stenosis. According to the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample (NIS), the annual estimate of laminectomy discharges averages around 34 discharges per 100,000 adults from 1998 to 2008.[
METHODS
We retrospectively reviewed medical records of all neurosurgical patients undergoing first-time, bilateral lumbar laminectomy for degenerative spinal disease from 1990 to 2012 at a single institution. Patients undergoing discectomy, hemilaminectomy, laminotomy, laminoplasty, complete facetectomy, and/or fusion were excluded.
All 500 patients underwent one, two, or three level lumbar laminectomy. Multiple accompanying comorbidities were also assessed (e.g. coronary artery disease, diabetes mellitus, osteoporosis, obesity, ever smoker, chronic obstructive pulmonary disease [COPD], hypertension, and depression). All had undergone complete clinical assessment by a staff neurosurgeon preoperatively. Clinical symptoms, back pain, neurogenic claudication, radiculopathy, sensory deficits, and weakness were retrospectively ascertained from clinical notes. We also evaluated those requiring subsequent lumbar surgery/reoperations to address wound dehiscence/infection, hematoma, and progression of degenerative disease. Progression of degenerative disease was defined as those who underwent reoperation for progression of disease either at the initial spinal pathology or adjacent segments. Indications for progression of degenerative disease were confirmed with radiological imaging.
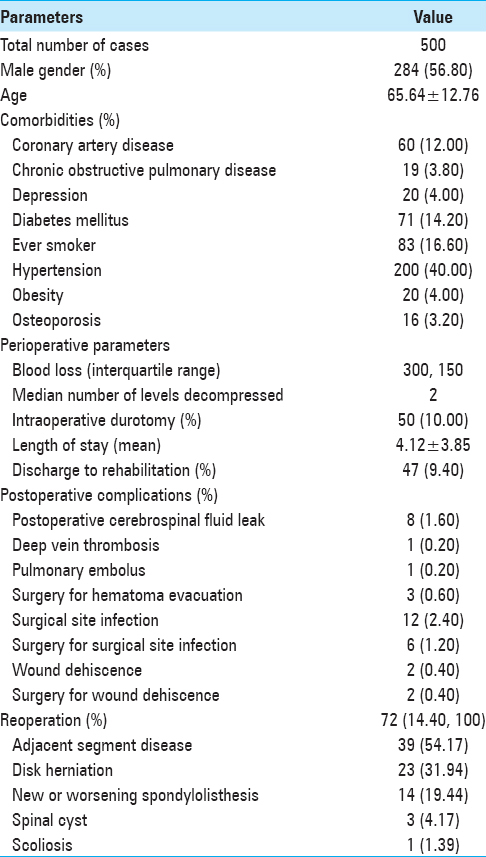
Perioperative characteristics including gender, age, comorbidities, perioperative parameters, and postoperative complications were evaluated [
RESULTS
Five hundred patients undergoing first-time, bilateral 1-3 level lumbar laminectomy for degenerative disease were followed for a mean of 46.79 months [
Intraoperative durotomy and postoperative cerebrospinal fluid fistulas
The rate of incidental intraoperative durotomy was 10.00% (n = 50); however, only 1.60% (n = 8 patients) experienced postoperative cerebrospinal fluid (CSF) leakage. Of the eight postoperative CSF leaks, two durotomies went undetected during the index operations. In both patients, the wound closure was accomplished with 0 polyglactin (VICRYL®, ETHICON) sutures for the fascia, 3-0 polyglactin for the skin, and staples for the skin edges. The remaining six durotomies were detected and primarily repaired during the index procedure. Of the six cases, dural repair included 4-0 nylon (NUROLON®, Ethicon) sutures (n = 2), 6-0 polypropylene (PROLENE®, Ethicon) sutures (n = 2), fibrin sealant (Evicel®, Ethicon or DuraSeal™, Covidien) (n = 3), and collagen matrix (DuraGen®, Integra) (n = 3). One patient underwent suture closure alone in a water-tight fashion, three underwent suture closure plus fibrin sealant, one patient underwent suture closure plus multilayers of fibrin sealant overlaid with collagen matrix then additional fibrin sealant, and one underwent subcutaneous fat graft fixated with collagen matrix. All six wound closures were over-sewn with 0 polyglactin sutures for the muscle layer, 2-0 (n = 1) or 3-0 (n = 5) polyglactin sutures for the fascial layers, and 3-0 nylon sutures for skin. Staples were not used to approximate the skin in any of six surgeries. Of the eight cases with postoperative CSF leakage, one patient required reoperation for repair of CSF leak; the remaining seven patients were managed with flat-bed rest and over-sewing of the wound. However, of the remaining 42 incidental durotomy cases without evidence of postoperative CSF leak, 2 patients were taken back to the operation room (OR) for pseudomeningocele repair and wound revision.
Length of stay, postoperative rehabilitation referral rate, complications, and reoperation rates
The mean length of hospital stay was 4.12 ± 3.85 days. Less than 10% required inpatient rehabilitation (n = 47). The risk of at least one postoperative complication was 5.60% (n = 28 patients ≥1 postoperative complication). Reoperations (2.0%) for nondegenerative pathologies included wound infection, dehiscence, or hematomas. Reoperations within 30 days were required in 10 patients for nondegenerative pathologies, and in 1 patient for a spinous process fracture.
Postoperative improvement in clinical symptoms
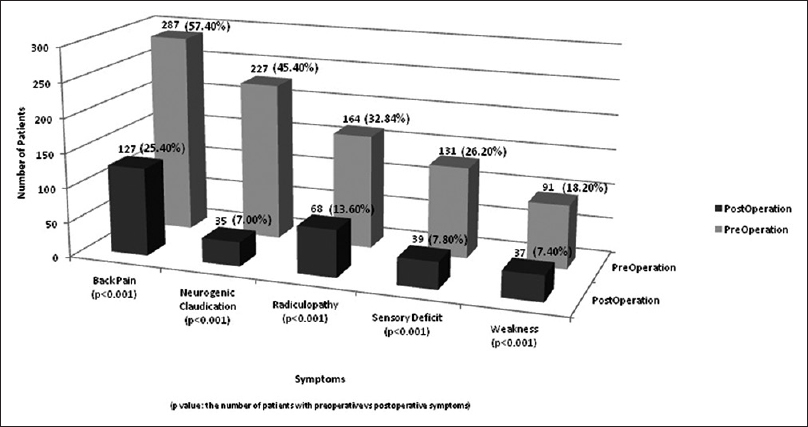
The number of patients with preoperative clinical symptoms improved in all categories following a lumbar laminectomy alone. Of 57.40% of patients presenting initially with back pain, only 25.40% had this symptom postoperatively (P < 0.001). Similar improvements (preoperative vs. postoperative) were reported for neurogenic claudication (45.40-7.00%, P < 0.001), radiculopathy (32.80% vs 13.60%, P < 0.001), weakness (18.20% vs 7.40%, P < 0.001), and sensory deficits (26.20-7.80%, P < 0.001) [
Reoperation rates for progression of degenerative disease
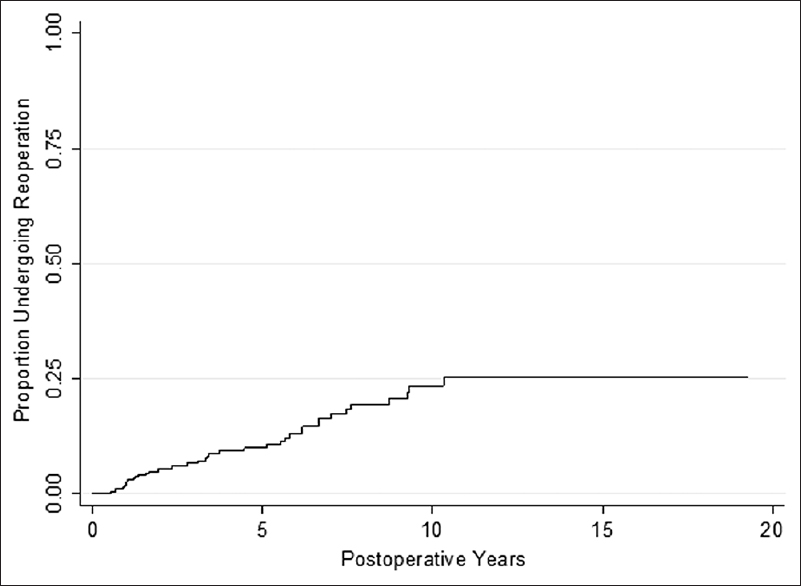
Reoperations were required in 14.40% (n = 72) of patients to address progression of degenerative disease over a mean interval of 3.40 years, yielding an annualized reoperation rate of 4.60% (IR = 0.046 person-years) [
Symptoms precipitating reoperations
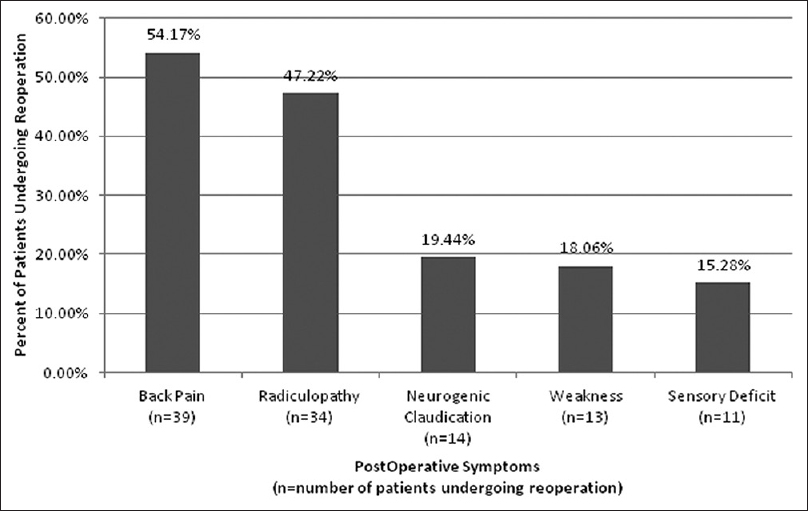
Of the 72 patients requiring reoperations after lumbar laminectomy, the most common recurrent symptoms included: Back pain (54.17%), radiculopathy (47.22%), neurogenic claudication (19.44%), weakness (18.06%), and sensory deficits (15.28%) [
DISCUSSION
In a large cohort series of 500 patients who underwent first-time, bilateral, 1-3 level lumbar laminectomy, the number of patients with preoperative back pain, radiculopathy, motor weakness, sensory deficit, and neurogenic claudication statistically significantly decreased postoperatively. The rate of durotomy during a lumbar laminectomy was 10.00%. This corroborates a retrospective review of 4835 lumbar spine operations over a 10-year period, in which Jankowitz et al. reported an incidental durotomy rate of 11.3%.[
In this series of 500 patients, the total reoperation incidence for progression of degenerative disease was 14.4% over a mean of 3.40 years, yielding an annualized reoperation rate of 4.60%. In a retrospective review of 88 patients undergoing lumbar laminectomy, Katz et al. reported a total reoperation incidence of 17% and 1-year reoperation incidence of 6%.[
References
1. Bydon M, Xu R, Santiago-Dieppa D, Macki M, Sciubba DM, Wolinsky JP. Adjacent-segment disease in 511 cases of posterolateral instrumented lumbar arthrodesis: Floating fusion versus distal construct including the sacrum. J Neurosurg Spine. 2014. 20: 380-6
2. Jankowitz BT, Atteberry DS, Gerszten PC, Karausky P, Cheng BC, Faught R. Effect of fibrin glue on the prevention of persistent cerebral spinal fluid leakage after incidental durotomy during lumbar spinal surgery. Eur Spine J. 2009. 18: 1169-74
3. Katz JN, Lipson SJ, Brick GW, Grobler LJ, Weinstein JN, Fossel AH. Clinical correlates of patient satisfaction after laminectomy for degenerative lumbar spinal stenosis. Spine. 1995. 20: 1155-60
4. Katz JN, Lipson SJ, Larson MG, McInnes JM, Fossel AH, Liang MH. The outcome of decompressive laminectomy for degenerative lumbar stenosis. J Bone Joint Surg Am. 1991. 73: 809-16
5. Malter AD, McNeney B, Loeser JD, Deyo RA. 5-year reoperation rates after different types of lumbar spine surgery. Spine. 1998. 23: 814-20
6. Rajaee SS, Bae HW, Kanim LE, Delamarter RB. Spinal fusion in the United States: Analysis of trends from 1998 to 2008. Spine. 2012. 37: 67-76
7. Santiago-Dieppa D, Bydon M, Xu R, De la Garza-Ramos R, Henry R, Sciubba DM. Long-term outcomes after non-instrumented lumbar arthrodesis. J Clin Neurosci. 2014. 21: 1393-7