- Department of Spine Surgery, Hospital Universitario Fundación Santa Fe de Bogotá, Bogota, Cundinamarca, Colombia.
Correspondence Address:
Omar Marroquin-Herrera, Department of Spine Surgery, Hospital Universitario Fundación Santa Fe de Bogotá, Bogota, Cundinamarca, Colombia.
DOI:10.25259/SNI_1039_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Omar Marroquin-Herrera, Santiago Andres Rosales-Camargo, Luis Carlos Morales-Sáenz, Fernando Alvarado-Gomez. Clostridium perfringens in the spine: A rare cause of post-surgical infection. 02-Nov-2021;12:544
How to cite this URL: Omar Marroquin-Herrera, Santiago Andres Rosales-Camargo, Luis Carlos Morales-Sáenz, Fernando Alvarado-Gomez. Clostridium perfringens in the spine: A rare cause of post-surgical infection. 02-Nov-2021;12:544. Available from: https://surgicalneurologyint.com/surgicalint-articles/11214/
Abstract
Background: Post-surgical infections of the spine occur in from 0% to 18% of cases. Postoperative spine infections due to Clostridium Perfringens (CP) resulting in necrotizing fasciitis are extremely rare. However, since they may be fatal, early and definitive treatment is critical.
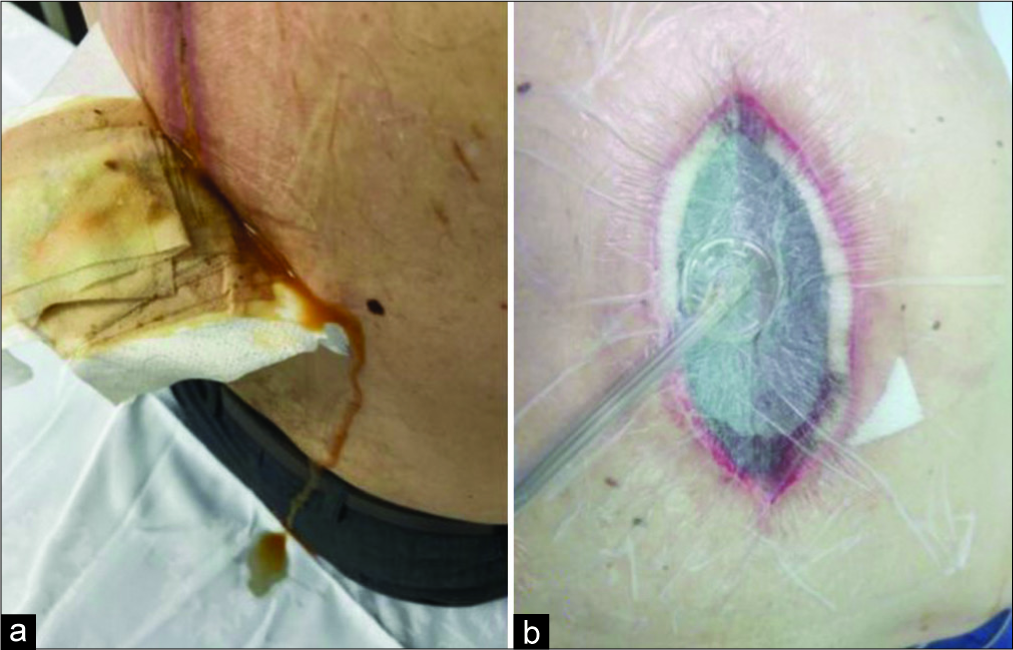
Case Description: A62-year-old male with a T8-T9 Type C fracture, in ASIA Grade “E” (neurologically intact) underwent a posterior T6-T10 arthrodesis. However, 2 weeks postoperatively, he developed a postoperative thoracic wound infection; the cultures were positive for CP. As the patient developed necrotizing fasciitis, emergent debridement, negative pressure continued drainage, and initiation of appropriate antibiotic therapy were critical.
Conclusion: Postoperative spinal infections due to CP with accompanying necrotizing fasciitis are extremely rare. As these infections may be fatal, they must be rapidly diagnosed and treated.
Keywords: Clostridium perfringens, Discitis, Necrotizing fasciitis, Postoperative infection, Spine
INTRODUCTION
Clostridium perfringens (CP) is a gram-positive anaerobic spore-forming microorganism found in the gastrointestinal tract and is the most common cause of gas gangrene. As CP can result in necrotizing fasciitis, with rapid progression to myonecrosis, gas production, and sepsis, CP must be rapidly diagnosed and treated (i.e. with antibiotics and surgical debridement).[
CASE REPORT
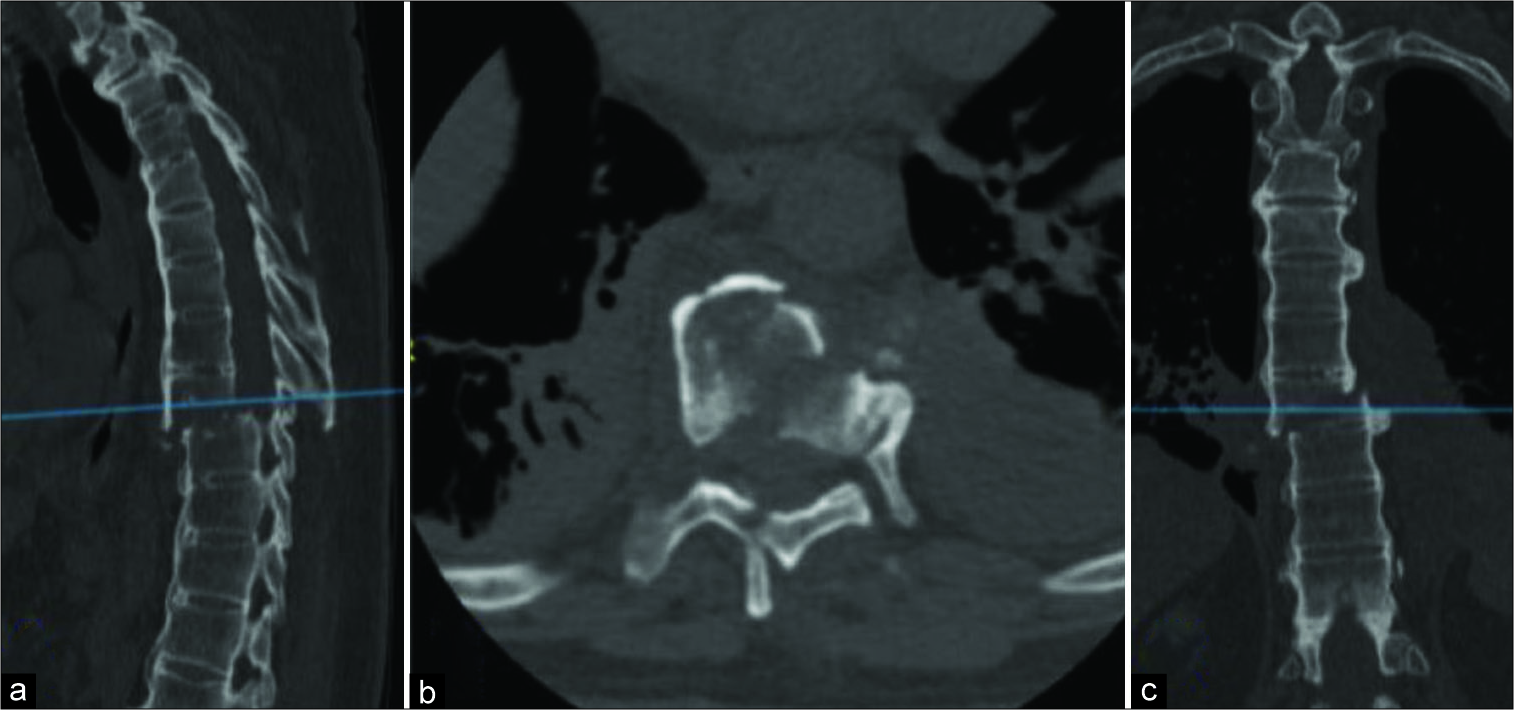
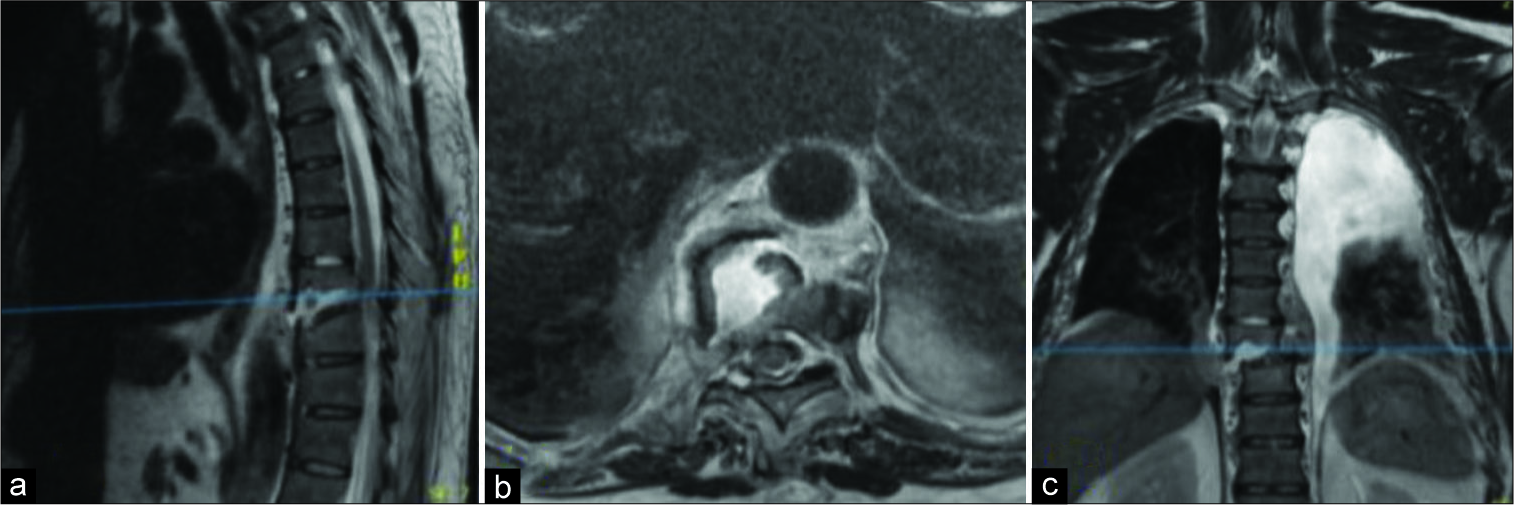
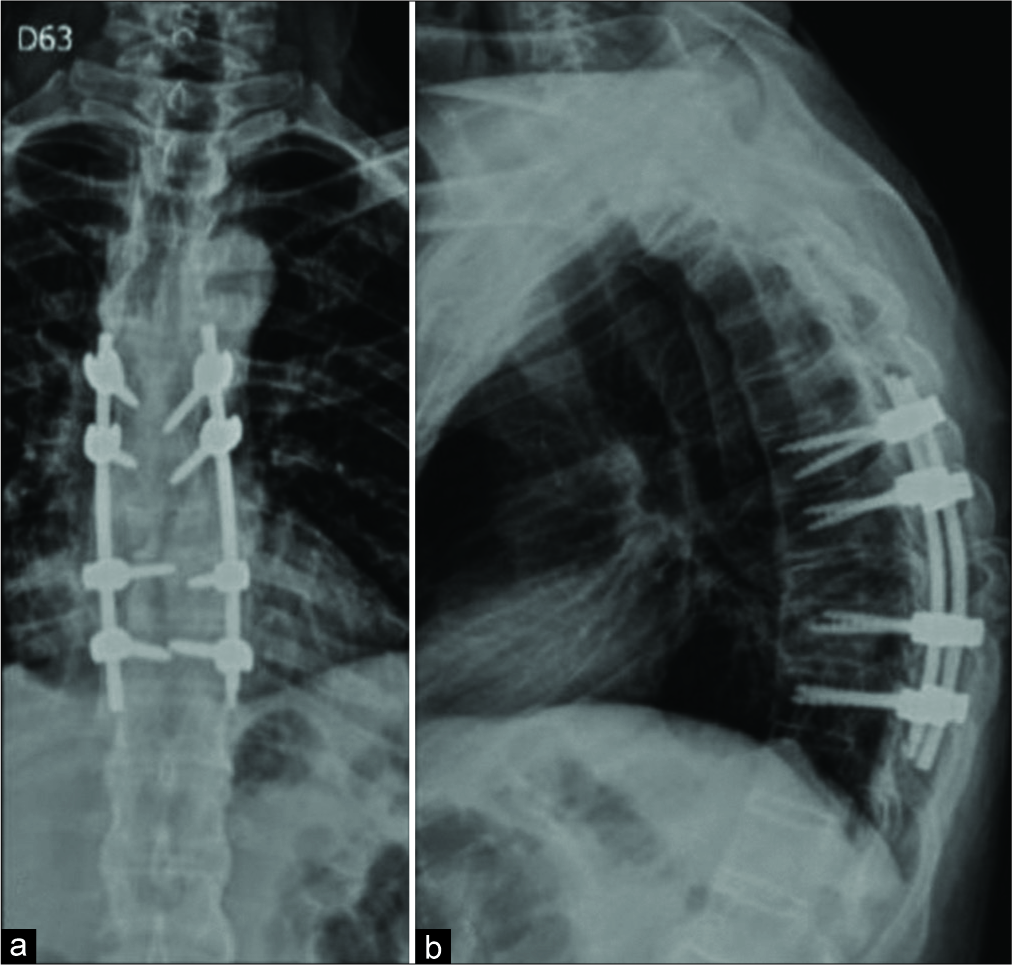
A 62-year-old male presented with a T8-T9 Type C fracture; neurologically intact [
Lab studies
Blood tests showed an elevated erythrocyte sedimentation rate (ESR 96 mm/H), a high C-reactive protein (CRP 12.6 mg/L), and increased peripheral leukocyte count (WBC 15,200/μL); all studies were consistent with sepsis.
Diagnostic studies
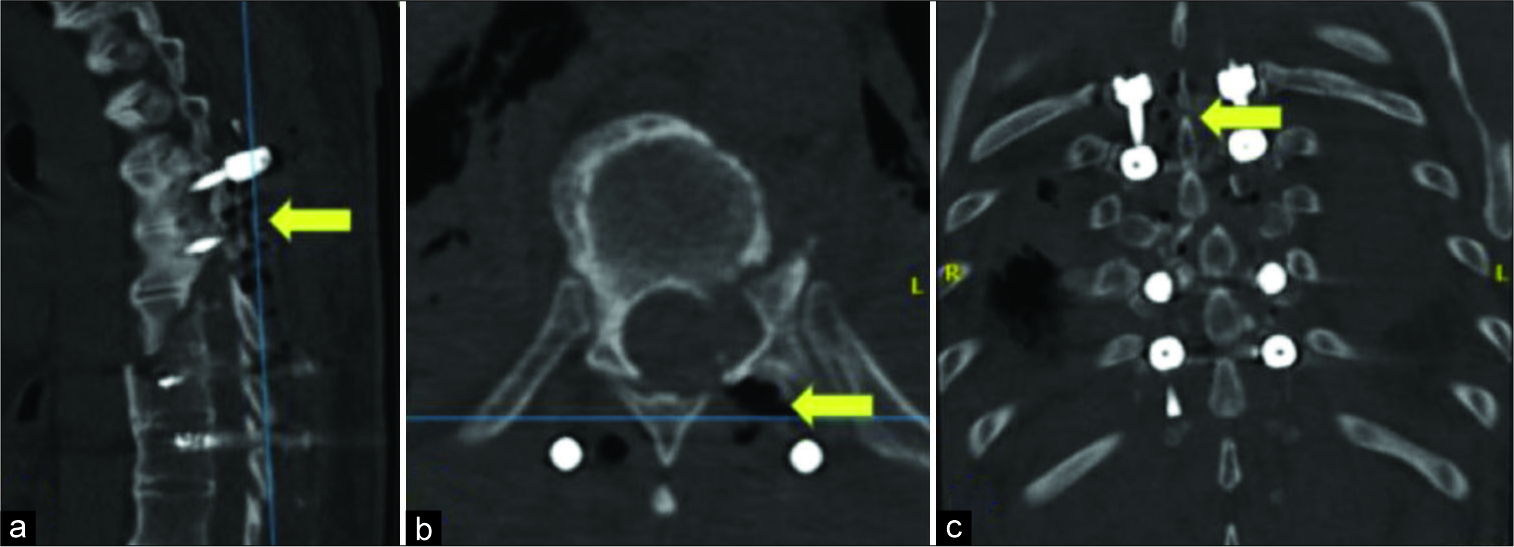
As the thoracic CT scan showed gas within the T6-T10 thoracic wound T6-T10 [
Antibiotic therapy
Cultures were taken which later showed CP. Although intravenous vancomycin was initially started postoperatively, 5 days later, the CP cultures showed sensitivity to Ceftaroline.
Postoperative course
Surgical wash-outs and drainage with the negative pressure suction system were repeated 4 times over 3 weeks During which time the patient continued to improve. He was discharged after 6 postoperative weeks, and of interest, the patient retained the transpedicular instrumentation system without the need for revision 6 months postoperatively [
DISCUSSION
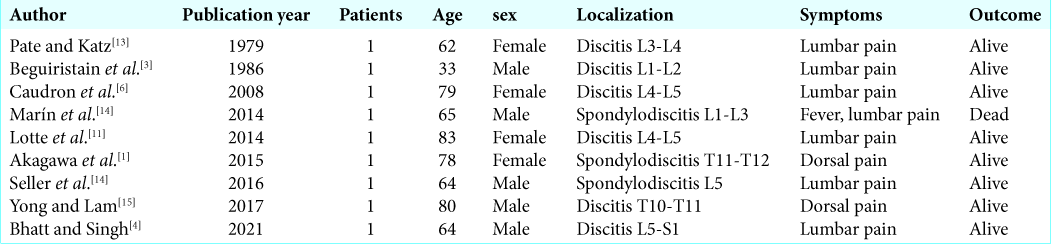
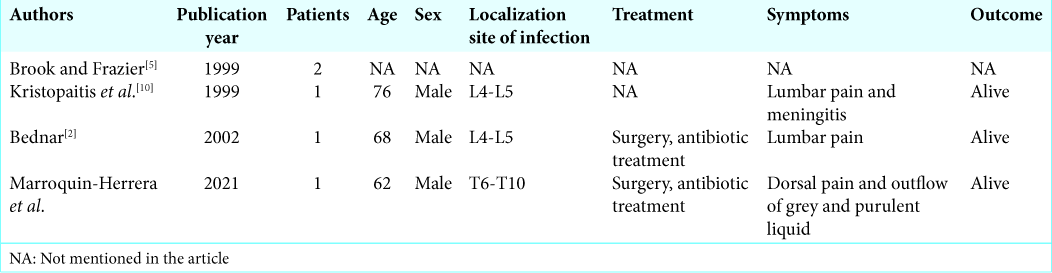
The presence of primary spine infections due to CP are rare,[
Necrotizing fasciitis due to CP
Necrotizing fasciitis due to CP usually occurs in the 2nd postoperative week. A CP infection of the spine usually causes the new onset of pain, fever, and potential neurological dysfunction, depending upon its location spine). Typically, there is a serious exudate that is grayish and contains bubbles.
Lab studies typical for CP
Laboratory tests for CP often demonstrate elevation of the peripheral white blood cell count plus acute phase reactants such as CRP, and the erythrocyte sedimentation rate.
Radiologist studies for CP
Radiographic studies for CP classically demonstrate gas within the wound and paravertebral space. As these lesions may prove fatal, they typically warrant emergent surgical debridement/wash-out, continued negative pressure drainage, and appropriate antibiotic therapy.[
CONCLUSION
CP is a rare cause of postoperative spine infections, As necrotizing fasciitis attributed to CP can be fatal, it should be rapidly diagnosed and treated (i.e., with operative debridement, continued negative suction drainage, and antibiotic therapy).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akagawa M, Kobayashi T, Miyakoshi N, Abe E, Abe T, Kikuchi K. Vertebral osteomyelitis and epidural abscess caused by gas gangrene presenting with complete paraplegia: A case report. J Med Case Rep. 2015. 9: 81
2. Bednar DA. Postoperative Clostridium perfringens lumbar discitis with septicemia: Report of a case with survival. J Spinal Disord Tech. 2002. 15: 172-4
3. Beguiristain JL, de Pablos J, Llombart R, Gómez A. Discitis due to Clostridium perfringens. Spine (Phila PA 1976). 1986. 11: 170-2
4. Bhatt H, Singh S. A 64-year-old man with low back pain due to Clostridium perfringens lumbar discitis. Am J Case Rep. 2021. 22: e928014
5. Brook I, Frazier EH. Aerobic and anaerobic microbiology of surgical-site infection following spinal fusion. J Clin Microbiol. 1999. 37: 841-3
6. Caudron A, Grados F, Boubrit Y, Coullet JM, Merrien D, Domart Y. Discitis due to Clostridium perfringens. Joint Bone Spine. 2008. 75: 232-4
7. Dowdell J, Brochin R, Kim J, Overley S, Oren J, Freedman B. Postoperative spine infection: Diagnosis and management. Glob Spine J. 2018. 8: 37S-43
8. Epstein NE. Preoperative measures to prevent/minimize risk of surgical site infection in spinal surgery. Surg Neurol Int. 2018. 9: 251
9. Gohari IM, Navarro MA, Li J, Shrestha A, Uzal F, McClane BA. Pathogenicity and virulence of Clostridium perfringens. Virulence. 2021. 12: 723-53
10. Kristopaitis T, Jensen R, Gujrati M. Clostridium perfringens A rare cause of postoperative spinal surgery meningitis. Surg Neurol. 1999. 51: 448-50
11. Lotte R, Popoff MR, Degand N, Lotte L, Bouvet P, Baudin G. Lumbar discitis caused by Clostridium perfringens. J Clin Microbiol. 2014. 52: 3813-5
12. Marín AS, Gómez CM, Tomé IC, Zabala AP. Spondylodiscitis due to Clostridium perfringens. Rev Clin Espanola. 2014. 214: 286-7
13. Pate D, Katz A. Clostridia discitis: A case report. Arthritis Rheum. 1979. 22: 1039-40
14. Seller M, Burghardt RD, Rolling T, Hansen-Algenstaedt N, Schaefer C. Clostridium perfringens A rare cause of spondylodiscitis case report and review of the literature. Br J Neurosurg. 2018. 32: 574-6
15. Yong CH, Lam M. Discitis and Clostridium perfringens bacteraemia. BMJ Case Rep. 2017. 2017: bcr2017220646