- Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, Wisconsin, USA
Correspondence Address:
Ha Son Nguyen
Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, Wisconsin, USA
DOI:10.4103/2152-7806.166785
Copyright: © 2015 Nguyen HS. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Nguyen HS, Doan N, Shabani S, Gelsomino M, Mueller W. Co-presentation of a subdural empyema and an infected ventriculoperitoneal shunt in an adult patient: A rare complication with review of literature. Surg Neurol Int 07-Oct-2015;6:
How to cite this URL: Nguyen HS, Doan N, Shabani S, Gelsomino M, Mueller W. Co-presentation of a subdural empyema and an infected ventriculoperitoneal shunt in an adult patient: A rare complication with review of literature. Surg Neurol Int 07-Oct-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/co-presentation-of-a-subdural-empyema-and-an-infected/
Abstract
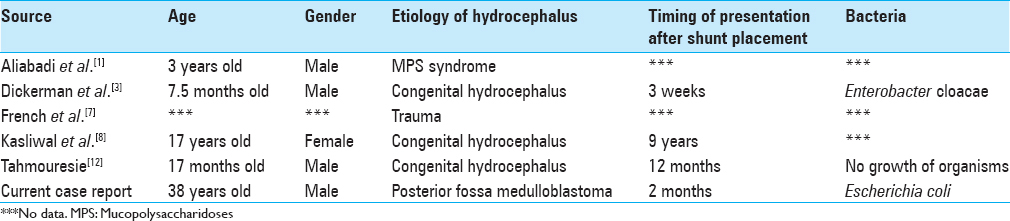
Background:The occurrence of a subdural empyema as a complication of a ventriculoperitoneal (VP) shunt infection is rare. Only three articles have been published on this topic. Moreover, the available literature only involves pediatric patients.
Case Description:The authors present a 38-year-old male with a preexisting right frontal subdural hygroma that developed into a subdural empyema in the presence of an infected right occipital VP shunt. A brief literature review is provided, and the pathogenesis is discussed.
Conclusion:This is the first known report regarding an adult patient with a subdural empyema and a VP shunt infection. Although a magnetic resonance imaging (MRI) brain is not typically ordered during diagnosis of a shunt infection, the authors advocate a low threshold to employ MRI brain to evaluate for other sources of infection, especially in an immunocompromised patient or in a patient with a history of a subdural hematoma or hygroma that can be easily overlook as being stable on computed tomography of head.
Keywords: Magnetic resonance imaging brain, subdural empyema, subdural hygroma, ventriculoperitoneal shunt
INTRODUCTION
Subdural empyema is a critical neurosurgical condition that may stem from neurosurgical procedures, trauma, meningitis, sinusitis, or otogenic infection.[
CASE REPORT
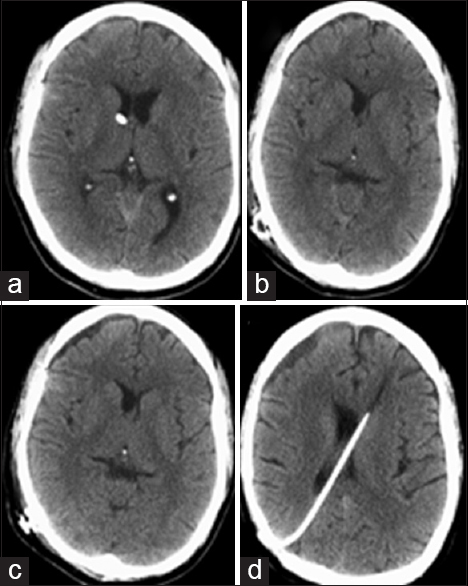
A 38-year-old male was consulted to rule out VP shunt infection. VP shunt was placed approximately 3 months prior to admission by an outside hospital (OSH). The patient presented with fever, emesis, and pancytopenia. Patient's history included a bilateral cerebellar mass resected by an OSH 3 months prior to admission. On postoperative day four, a right external ventricular drain (EVD) was placed due to hydrocephalus. Subsequently, the patient underwent right occipital VP shunt placement 10 days later. A follow-up computed tomography (CT) demonstrated interval development of right frontal subdural collection [Figure
Figure 1
(a) Computed tomography (CT) head with right frontal external ventricular drain (EVD) in place; (b) CT head after right EVD removed and right occipital ventriculoperitoneal shunt placed with the present of a small right frontal hypodense extra-axial fluid; (c) CT head a few days later demonstrates slight interval enlargement of right frontal subdural fluid; (d) CT head on the day of admission, which is approximately 3 months postsurgery, for shunt infection redemonstrates moderate enlargement of right frontal subdural fluid
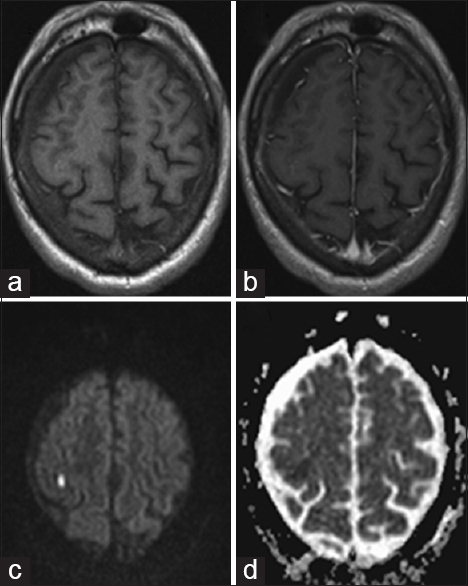
Figure 2
Magnetic resonance (MR) imaging was done 1-month prior to admission or 2 months postsurgery (a); MR T1 without contrast reveals right frontal subdural fluid (b); MR T1 with contrast reveals no enhancement of subdural fluid collection (c); Diffusion weighted imaging and (d); Apparent diffusion coefficient sequences failed to show restricted diffusion, suggesting a sterile subdural fluid collection that consisting with hygroma
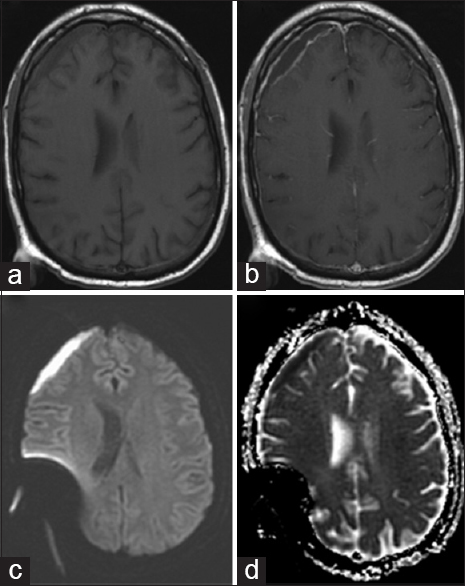
Given the recent surgery, fever, and symptoms, there was serious concern for shunt infection. Cerebrospinal fluid (CSF) from shunt valve was obtained, which showed Gram-negative rods and Gram-positive cocci. MRI of brain with and without contrast revealed right frontal subdural fluid collection with ring enhancement and restricted diffusion, highly suspicious of subdural empyema [Figure
Figure 3
Magnetic resonance (MR) was done on the day of admission with the diagnosis of shunt infection or approximately 3 months postsurgery (a); MR T1 sequence without contrast reveals right frontal subdural fluid (b); MR T1 sequence with contrast reveals ring enhancement of subdural fluid collection (c); Diffusion-weighted imaging and (d); Apparent diffusion coefficient sequences show significant restricted diffusion, suggesting the development of a subdural empyema, which was not present a month prior
DISCUSSION
To our knowledge, there have been no prior reports regarding an adult patient with a subdural empyema after placement of a VP shunt [
Subdural empyema can present with headaches, fevers, mental status deterioration, focal motor deficits, and seizure activity.[
Another possible source of infection is the recent diagnostic lumbar puncture, which may cause meningitis and seed the hygroma and the shunt as well. A meta-analysis of 179 cases of meningitis after lumbar puncture revealed that approximately 9% were attributed to a diagnostic lumbar puncture; most of the other cases were linked to spinal anesthesia, where there is also injection of material into the spinal canal.[
A VP shunt infection is typically diagnosed after a workup that includes a CT head, a shunt series, and shunt reservoir tap. An abdominal ultrasound may also be obtained to rule out a pseudocyst. Once an infection is confirmed, the shunt is externalized, and the infection is treated appropriately. Typically, MRI brain is not ordered in the case of shunt infection. In fact, a shunted patient was reported to have a subdural empyema undiagnosed and untreated for up to 9 years due to the lack of MRI and as a result, the patient suffered significant neurological injury.[
CONCLUSION
Subdural empyema is an unusual complication of a VP shunt. There should be a high suspicion of this pathology in a patient with a history of a subdural hematoma or hygroma. Subdural empyema requires urgent, if not emergent, treatment to minimize neurological injuries. Consequently, there should be a low threshold to obtain MRI brain during workup for a shunt infection. A prompt diagnosis of a subdural empyema offers the advantage of draining the infection and externalization of the infected shunt in the same operation.
References
1. Aliabadi H, Reynolds R, Powers CJ, Grant G, Fuchs H, Kurtzberg J. Clinical outcome of cerebrospinal fluid shunting for communicating hydrocephalus in mucopolysaccharidoses I, II, and III: A retrospective analysis of 13 patients. Neurosurgery. 2010. 67: 1476-81
2. Baer ET. Post-dural puncture bacterial meningitis. Anesthesiology. 2006. 105: 381-93
3. Dickerman RD, Piatt JH, Hsu F, Frank EH. Subdural empyema complicating cerebrospinal fluid shunt infection. Pediatr Neurosurg. 1999. 30: 310-1
4. Dill SR, Cobbs CG, McDonald CK. Subdural empyema: Analysis of 32 cases and review. Clin Infect Dis. 1995. 20: 372-86
5. Edwards NC, Engelhart L, Casamento EM, McGirt MJ. Cost-consequence analysis of antibiotic-impregnated shunts and external ventricular drains in hydrocephalus. J Neurosurg. 2015. 122: 139-47
6. Eng RH, Seligman SJ. Lumbar puncture-induced meningitis. JAMA. 1981. 245: 1456-9
7. French H, Schaefer N, Keijzers G, Barison D, Olson S. Intracranial subdural empyema: A 10-year case series. Ochsner J. 2014. 14: 188-94
8. Kasliwal MK, Sinha S, Kumar R, Sharma BS. Giant hemicranial calcified subdural empyema - Unusual complication following ventriculoperitoneal shunt insertion. Indian J Pediatr. 2009. 76: 651-2
9. Khan M, Griebel R. Subdural empyema: A retrospective study of 15 patients. Can J Surg. 1984. 27: 283-5
10. Miller ES, Dias PS, Uttley D. Management of subdural empyema: A series of 24 cases. J Neurol Neurosurg Psychiatry. 1987. 50: 1415-8
11. Pathak A, Sharma BS, Mathuriya SN, Khosla VK, Khandelwal N, Kak VK. Controversies in the management of subdural empyema. A study of 41 cases with review of literature. Acta Neurochir (Wien). 1990. 102: 25-32
12. Tahmouresie A. Subdural empyema secondary to ventriculo-peritoneal shunt. N Y State J Med. 1979. 79: 375-6
13. Tewari MK, Sharma RR, Shiv VK, Lad SD. Spectrum of intracranial subdural empyemas in a series of 45 patients: Current surgical options and outcome. Neurol India. 2004. 52: 346-9