- Department of Neurosurgery, Kano General Hospital, Osaka, Japan
- Department of Neurosurgery, Osaka Medical and Pharmaceutical University, Takatsuki, Japan.
Correspondence Address:
Yuichiro Tsuji, Department of Neurosurgery, Kano General Hospital, Osaka, Japan.
DOI:10.25259/SNI_810_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yuichiro Tsuji1, Yuzo Kuroda1, Masahiko Wanibuchi2. Coil embolization for ruptured distal anterior cerebral artery aneurysm at the supracallosal portion: Two case reports. 22-Dec-2023;14:444
How to cite this URL: Yuichiro Tsuji1, Yuzo Kuroda1, Masahiko Wanibuchi2. Coil embolization for ruptured distal anterior cerebral artery aneurysm at the supracallosal portion: Two case reports. 22-Dec-2023;14:444. Available from: https://surgicalneurologyint.com/surgicalint-articles/12676/
Abstract
Background: Distal anterior cerebral artery (ACA) aneurysms occur more frequently in the genu portion and much less frequently in the supracallosal portion (A4–A5). This report describes two cases of ruptured cerebral aneurysms occurring at the supracallosal portion successfully treated with coil embolization.
Case Description: Case 1 involved a 61-year-old female with sudden-onset headache and vomiting attributed to subarachnoid hemorrhage (SAH). Digital subtraction angiography (DSA) revealed a bihemispheric ACA and aneurysm in the supracallosal portion. Coil embolization was performed, and the patient was discharged without neurological deficit. Case 2 involved a 35-year-old man with severe headache and disturbance of consciousness caused by SAH. DSA showed an aneurysm in A4 of the accessory ACA, and coil embolization was performed. After rehabilitation, he was discharged with a modified Rankin scale score of 2.
Conclusion: Coil embolization for a ruptured aneurysm at the supracallosal portion can yield good results if the patient is appropriately selected.
Keywords: Coil embolization, Distal anterior cerebral artery, Supracallosal portion
INTRODUCTION
Distal anterior cerebral artery (DACA) aneurysms account for approximately 5% of all aneurysms.[
In this report, we describe two cases of ruptured cerebral aneurysms in the supracallosal portion successfully treated with coil embolization.
CASE REPORTS
Case 1
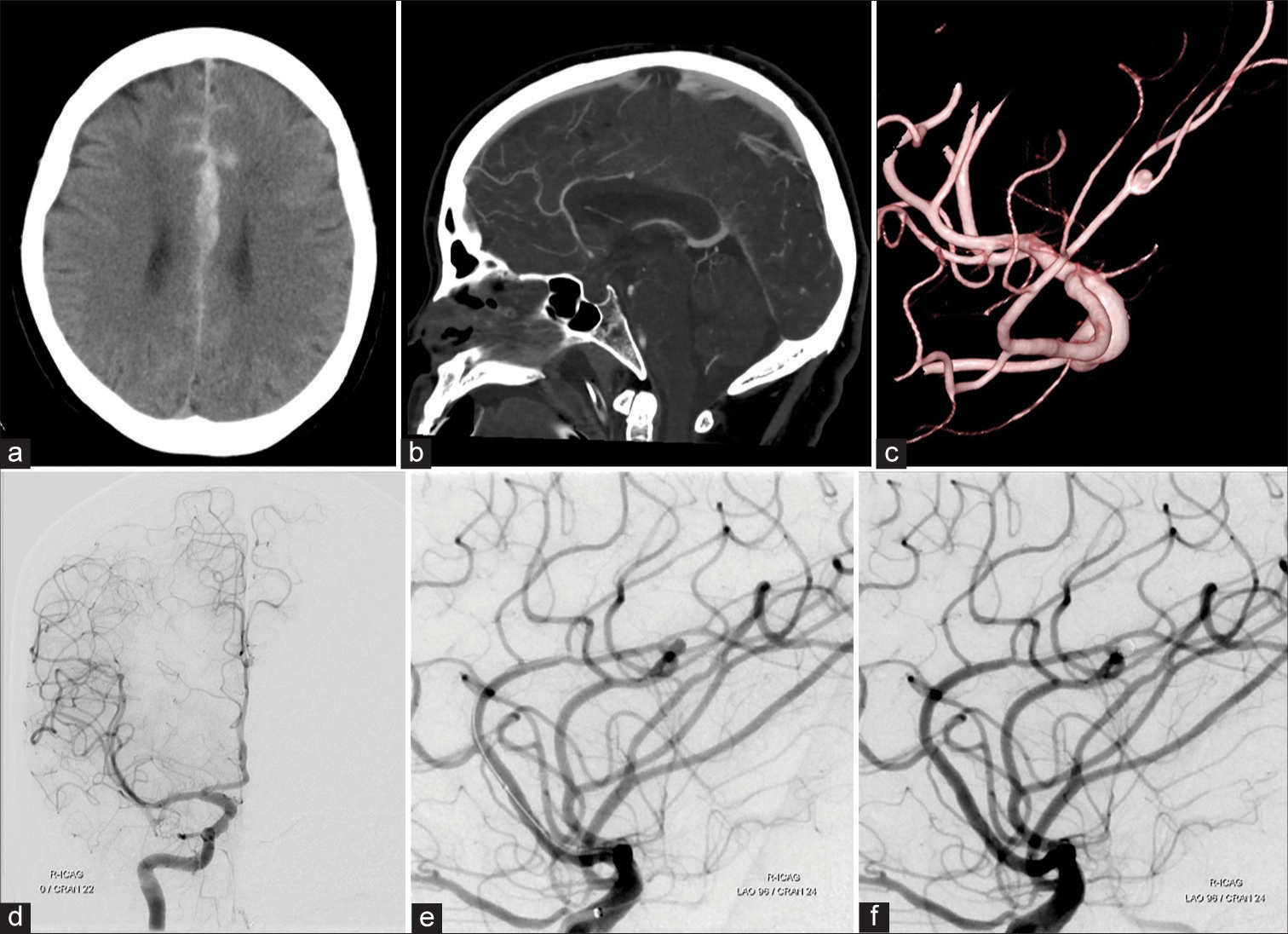
A 61-year-old female presented to the emergency department after the sudden onset of headache and vomiting. Her Glasgow Coma scale (GCS) score was 15. Computed tomography (CT) of the brain revealed a subarachnoid hemorrhage (SAH) and hematoma in the interhemispheric fissure [
Figure 1:
(a) Plain computed tomography (CT) of the brain revealed a subarachnoid hemorrhage and hematoma in the interhemispheric fissure. (b and c) CT angiography of sagittal view (b) and 3D digital subtraction angiography (c) showed an aneurysm at the A4-A5 junction. (d and e) Right internal cerebral artery angiogram showed a bihemispheric type anterior cerebral artery and a saccular aneurysm. (f) Postoperative angiogram showed complete obliteration of the aneurysm.
Case 2
A 35-year-old man was admitted to the emergency room with a sudden onset of headache, vomiting, and disturbance of consciousness. His GCS score was 6 (E1V1M4), and he was diagnosed with SAH. Brain CT revealed intracerebral hemorrhage and SAH from the corpus callosum to the cingulate gyrus [
Figure 2:
(a) Initial computed tomography (CT) of the brain showed intracerebral hemorrhage and subarachnoid hemorrhage in the cingulate gyrus. (b and c) CT angiography of sagittal view (b) and 3D digital subtraction angiography (c) showed a saccular aneurysm at the A3-A4 junction. (d and e) Right internal cerebral artery angiogram showed an accessory anterior cerebral artery and a saccular aneurysm. (f) Postoperative angiogram showed complete obliteration of the aneurysm.
DISCUSSION
Aneurysms in the A4 and A5 (supra callosal portion) located distal to the genu of the corpus callosum are estimated to account for 0.5% of all aneurysms.[
In previous reports, almost all aneurysms in the supracallosal portion were treated with aneurysmal neck clipping.[
Endovascular treatment of ruptured DACA aneurysms is considered preferable for patients with an aneurysm dome/neck ratio >1.5, poor or complicated clinical status, and no large hematoma within the intracranial area. In addition, coiling is more favorable than clipping in clinical outcomes and the incidence of treatment-related complications for ruptured DACA aneurysms.[
During intraoperative rupture, hemostasis near the ruptured aneurysm using a balloon catheter is most effective; however, it is difficult to use for DACA aneurysms due to the small diameter of the mother vessel. Therefore, the use of a balloon-guiding catheter for intraoperative rupture was considered effective for treating DACA aneurysms, which is also used in Case 2. In the case of DACA aneurysms, it is difficult to completely block the blood flow due to cross-blood flow through the anterior communicating artery. However, it is effective in terms of hemostasis and flow control during intraoperative rupture and provides a safe treatment.
By contrast, coil embolization of DACA aneurysms has a higher incidence of recurrence after endovascular therapy than that of other portions. The loose coil packing rate is a factor that leads to recurrence.[
To date, several cases of coil embolization or parent artery occlusion of a traumatic aneurysm have been reported at the supracallosal portion.[
A simple technique is usually selected for coil embolization of aneurysms at the supracallosal portion due to the long approach route and vessel diameter of the parent artery.[
CONCLUSION
Coil embolization was performed in two cases of ruptured cerebral aneurysms in the supracallosal portion. Although clipping surgery is usually the selected treatment for ruptured aneurysms in this region, coil embolization can provide excellent results if patient selection is appropriate. We expect that indications for endovascular treatment will be expanded in the future.
Ethical approval
The current study has been performed in accordance with the Declaration of Helsinki. IRB approval number is 23012. Date; September 25th, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Carvi y Nievas MN. The influence of configuration and location of ruptured distal cerebral anterior artery aneurysms on their treatment modality and results: Analysis of our casuistry and literature review. Neurol Res. 2010. 32: 73-81
2. Cavalcanti DD, Abla AA, Martirosyan NL, McDougall CG, Spetzler RF, Albuquerque FC. Endovascular management of distal ACA aneurysms: Single-institution clinical experience in 22 consecutive patients and literature review. AJNR Am J Neuroradiol. 2013. 34: 1593-9
3. Hernesniemi J, Tapaninaho A, Vapalahti M, Niskanen M, Kari A, Luukkonen M. Saccular aneurysms of the distal anterior cerebral artery and its branches. Neurosurgery. 1992. 31: 994-8
4. Lehecka M, Dashti R, Hernesniemi J, Niemelä M, Koivisto T, Ronkainen A. Microneurosurgical management of aneurysms at A4 and A5 segments and distal cortical branches of anterior cerebral artery. Surg Neurol. 2008. 70: 352-67
5. Lehecka M, Porras M, Dashti R, Niemelä M, Hernesniemi JA. Anatomic features of distal anterior cerebral artery aneurysms: A detailed angiographic analysis of 101 patients. Neurosurgery. 2008. 63: 219-28
6. Matsuzaki K, Uno M, Fujihara T, Miyamoto T, Yokosuka K, Toi H. Ruptured distal accessory anterior cerebral artery aneurysm--case report. Neurol Med Chir (Tokyo). 2011. 51: 839-42
7. Morigaki R, Uno M, Matsubara S, Satoh K, Nagahiro S. Choreoathetosis due to rupture of a distal accessory anterior cerebral artery aneurysm. Cerebrovasc Dis. 2008. 25: 285-7
8. Morioka M, Fujioka S, Itoyama Y, Ushio Y. Ruptured distal accessory anterior cerebral artery aneurysm: Case report. Neurosurgery. 1997. 40: 399-401
9. Ohno K, Monma S, Suzuki R, Masaoka H, Matsushima Y, Hirakawa K. Saccular aneurysms of the distal anterior cerebral artery. Neurosurgery. 1990. 27: 907-12
10. Park HS, Kwon SC, Kim MH, Park ES, Sim HB, Lyo IU. Endovascular coil embolization of distal anterior cerebral artery aneurysms: Angiographic and clinical follow-up results. Neurointervention. 2013. 8: 87-91
11. Park KY, Kim BM, Lim YC, Chung J, Kim DJ, Joo JY. The role of endovascular treatment for ruptured distal anterior cerebral artery aneurysms: Comparison with microsurgical clipping. J Neuroimaging. 2015. 25: 81-6
12. Sui M, Mei Q, Sun K. Surgical treatment achieves better outcome in severe traumatic pericallosal aneurysm: Case report and literature review. Int J Clin Exp Med. 2015. 8: 1598-603
13. Take Y, Kamide T, Kikkawa Y, Ikegami M, Teranishi A, Ehara T. Current treatment options and prognostic factors for ruptured distal anterior cerebral artery aneurysms. Surg Neurol Int. 2021. 12: 171
14. Uchino K, Kondo K, Harada N, Aoki Y, Noguchi Y, Oishi H. A case of a ruptured aneurysm at the supracallosal portion (A4-A5) of the bihemispheric anterior cerebral artery treated with endovascular surgery. J Neuroendovasc Ther. 2022. 16: 147-51
15. Zhou J, Wang Y, Wang D, Chen Q, Wang H, Gao L. Endovascular treatment for ruptured aneurysms at distal cerebral arteries. World Neurosurg. 2019. 123: e387-92