- Department of Neurosurgery, University of Tsukuba, Tsukuba, Ibaraki, Japan.
- Department of Otolaryngology, University of Tsukuba, Tsukuba, Ibaraki, Japan.
Correspondence Address:
Hiroyoshi Akutsu
Department of Neurosurgery, University of Tsukuba, Tsukuba, Ibaraki, Japan.
DOI:10.25259/SNI_826_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Erika Yamada1, Hiroyoshi Akutsu1, Hiroyoshi Kino1, Shuho Tanaka2, Hidetaka Miyamoto2, Takuma Hara1, Masahide Matsuda1, Shingo Takano1, Akira Matsumura1, Eiichi Ishikawa1. Combined simultaneous endoscopic endonasal and microscopic transventricular surgery using a port retractor system for giant pituitary adenoma: A technical case report. 08-Mar-2021;12:90
How to cite this URL: Erika Yamada1, Hiroyoshi Akutsu1, Hiroyoshi Kino1, Shuho Tanaka2, Hidetaka Miyamoto2, Takuma Hara1, Masahide Matsuda1, Shingo Takano1, Akira Matsumura1, Eiichi Ishikawa1. Combined simultaneous endoscopic endonasal and microscopic transventricular surgery using a port retractor system for giant pituitary adenoma: A technical case report. 08-Mar-2021;12:90. Available from: https://surgicalneurologyint.com/surgicalint-articles/10633/
Abstract
Background: We report a case of a giant pituitary adenoma with marked extension into the third ventricle that was successfully removed using combined simultaneous endoscopic endonasal surgery (EES) and microscopic transventricular port surgery.
Case Description: A 47-year-old woman, who complained of memory disturbance, had a giant pituitary adenoma with marked extension into the third ventricle that was causing obstructive hydrocephalus. She underwent combined EES and microscopic transventricular surgery using a port retractor system. Most of the tumor was resected from the EES side with assistance from the transcranial side with minimum cortical trajectory damage. The tumor was completely excised without any complications.
Conclusion: For giant pituitary adenoma with marked extension into the third ventricle, combined simultaneous EES and transventricular surgery using a port retractor system is effective to maximize the extent of tumor resection while also preventing complications. Using port surgery on the transcranial side, microscopic secure dissection is possible with minimum additional cortical damage.
Keywords: Combined endoscopic endonasal surgery and transcranial surgery, Giant pituitary adenoma, Minimally invasive surgery, Port surgery
INTRODUCTION
Recently, excellent results of endoscopic endonasal surgery (EES) for pituitary adenoma have been reported.[
CASE DESCRIPTION
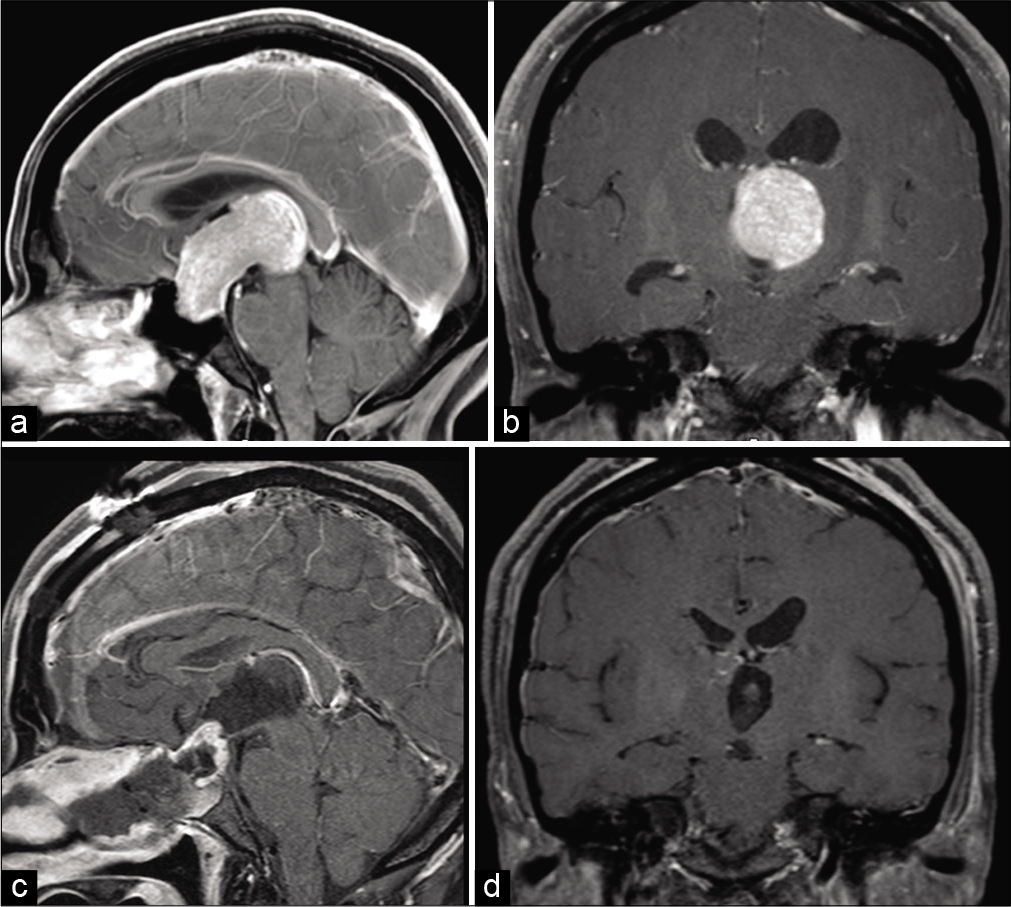
A 47-year-old woman was admitted to a local hospital because of memory disturbance. Magnetic resonance imaging (MRI) showed a giant pituitary adenoma; therefore, she was referred to our hospital for more extensive diagnosis and specialized treatment. At the time of admission, mild cognitive deficit was revealed through a psychometric test: the scores of the Mini-Mental State Examination (MMSE) and Revised Hasegawa Dementia Scale (HDS-R) were 21/30 and 18/30, respectively. Her visual acuity was 1.0 (right) and 1.0 (left), and Goldmann perimetry testing revealed bitemporal hemianopia. In addition, bilateral papilledema was detected. A blood test showed hyperprolactinemia (PRL 386 ng/ml, normal range 4.1–28.9) and hypothyroidism (free T4 0.66 ng/ml, normal range 0.9–1.7; free T3 2.0 ng/ml, normal range 2.3–4.0), but no abnormality otherwise. MRI revealed an intrasellar and suprasellar contrast-enhanced mass lesion (maximum diameter of 55 mm) extending into the third ventricle causing the obstructive hydrocephalus [
Regarding the surgical strategy, we expected that most of the tumor could be removed by EES; however, we were afraid of the risk of postoperative hemorrhage from the residual tumor due to the marked tumor extension into the third ventricle. Therefore, we planned combined simultaneous EES and transventricular surgery so that we could resect or at least assist resection from above the uppermost part of the tumor. For the transventricular surgery, we selected the transcortical route because of the presence of ventriculomegaly, and we additionally used a port retractor system, the ViewSite Brain Access System (Vycor Medical Inc., FL, USA), to minimize the surgical trajectory.
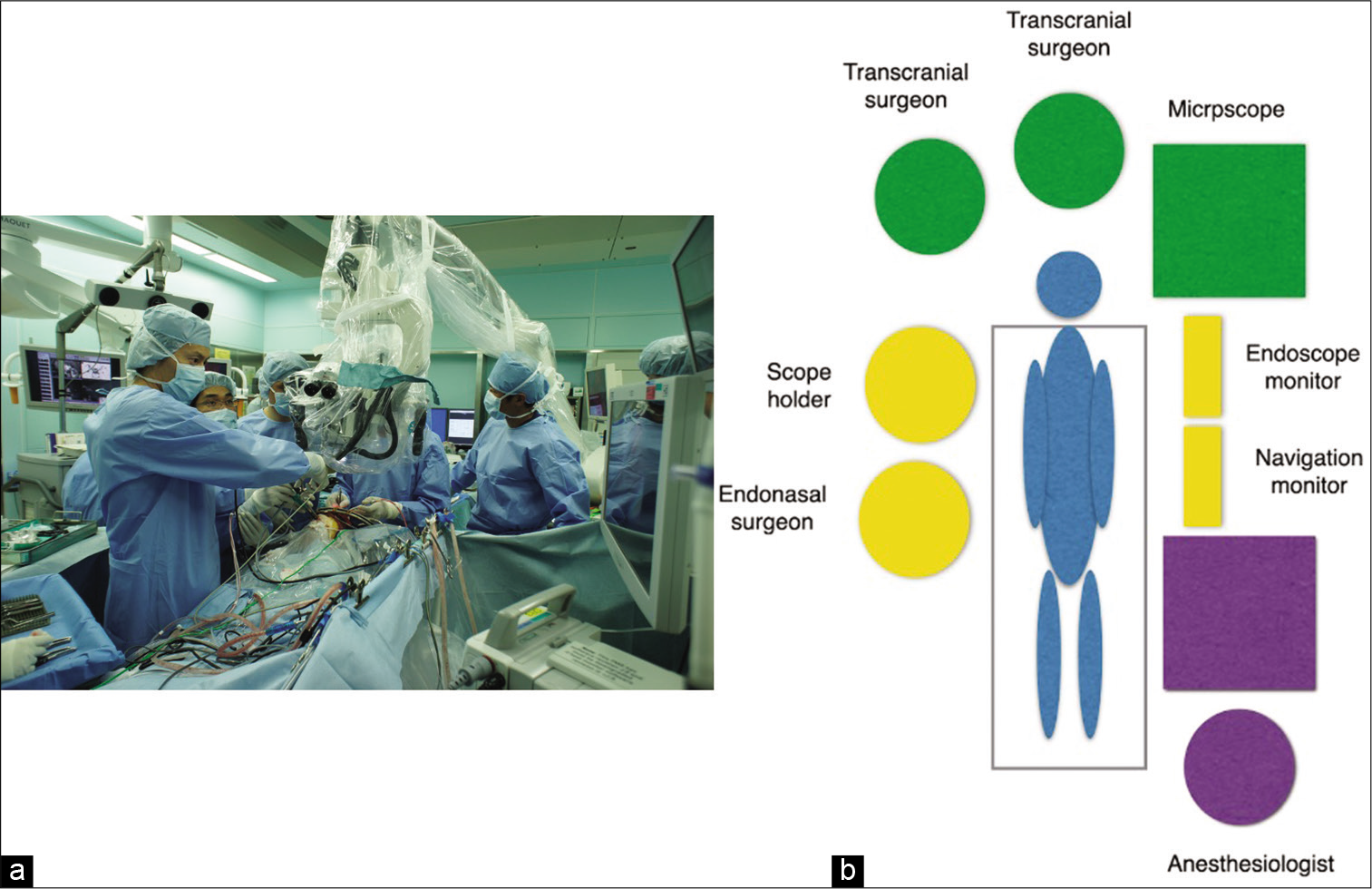
The operation was started from above and below at the same time. The operative setting is shown in [
Figure 2:
The photograph (a) and schematic diagram (b) show the setup for the combined endoscopic endonasal surgery (EES) and microscopic transcranial (transventricular) surgery. During the operation, the two surgeons performing the transcranial surgery are on the cranial side and the two surgeons performing the EES are on the right side of the patient. On the left side of the patient, the microscope is placed most cranially, then the monitors of the endoscope and navigation are placed, and the anesthesiologist is standing caudally.
EES
When indicated, EES is typically performed in all cases of 3- or 4-handed surgeries done by an interdisciplinary team of neurosurgeons and otolaryngologists at our hospital. In this case, the middle turbinate was gently lateralized, and the nasal septum mucosa was incised and elevated. After the resection of the posterior bony nasal septum, the anterior wall of the sphenoid sinus was widely opened using a drill. Next, the skull base bone resection area was enlarged to expose the dura mater from the sellar floor to the frontal base. The area of the bone resection included the sellar floor, the tuberculum sellae, the medial part of the bilateral carotid prominence, and the medial opticocarotid recess, facilitating resection of the suprasellar and lateral compartments of the tumor.
Microscopic transventricular surgery using a port retractor system
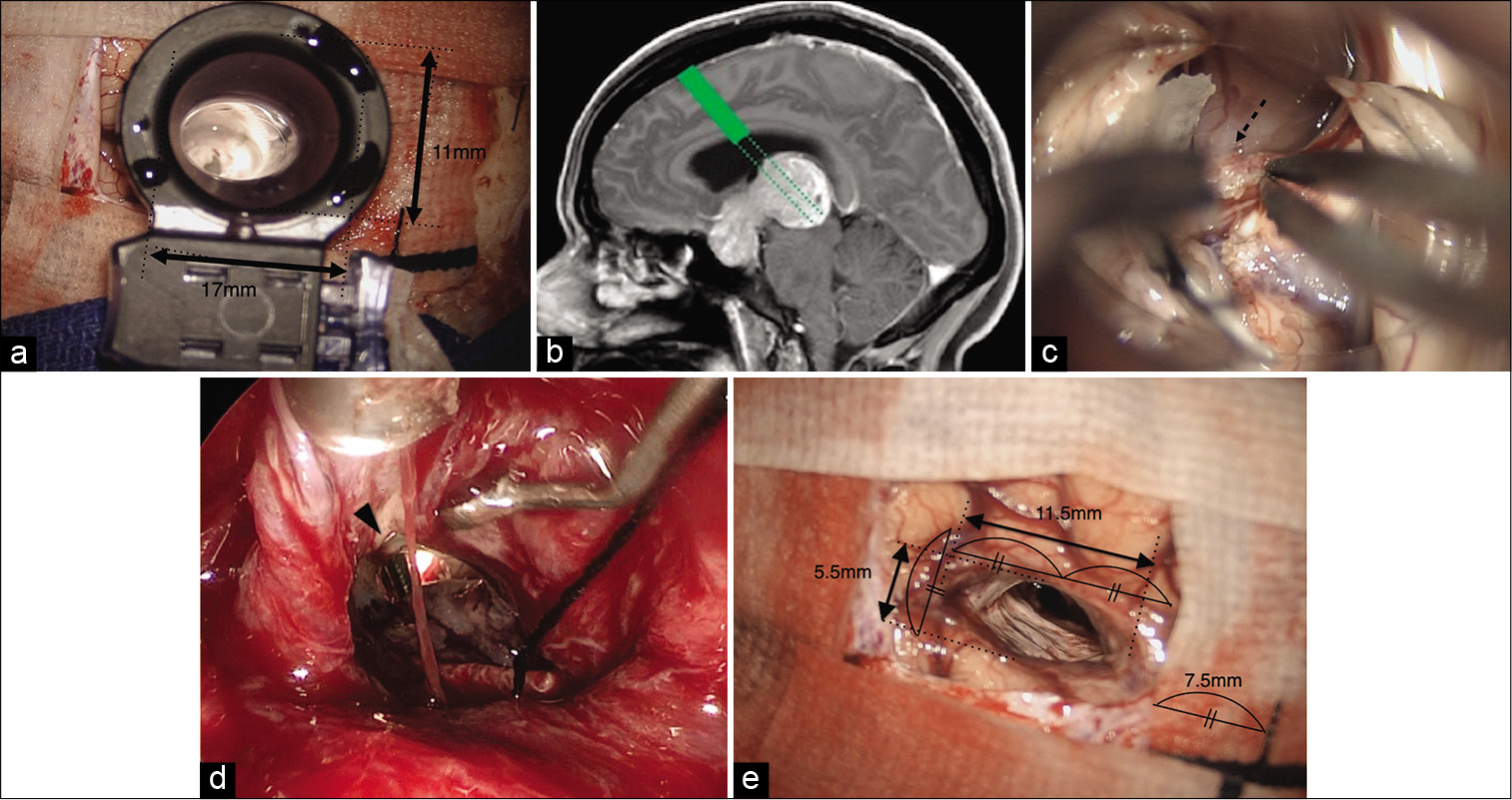
Bicoronal skin incision. After small right frontal craniotomy, the port retractor, 17 mm x 11 mm in distal opening width and 70 mm in length, was inserted into the right anterior horn along the tract of the ventricular catheter that was inserted under the navigation guide [
Figure 3:
(a) After the ventricular catheter is inserted through the right anterior horn and the outflow of the cerebrospinal fluid is confirmed, a port retractor (ViewSite Brain Access System) (17 mm × 11 mm in distal opening width, 70 mm in length) is inserted along the tract of the tube. The port retractor is connected with the Budde Halo self-retaining retractor system. (b) The direction (green dotted line) of the port retractor (green rectangle) for the microscopic transventricular approach. The direction of the port retractor is aiming to the most upper and dorsal part of the tumor, which is the most difficult area to reach from the endonasal side. (c) Microscopic view through the inserted port retractor. The tumor (arrow) is observed beyond the foramen of Monro (dotted line). Due to the obstructive hydrocephalus, the foramen of Monro is dilated; therefore, the working space is sufficient for following the procedure through the foramen of Monro. (d) Microscopic view through the port retractor. The choroid plexus (dotted arrow) and surrounding veins are attached to the upper surface of the tumor and are detached by means of microscopic bimanual dissection using a thin tip bipolar coagulator and suction. (e) Endoscopic view from the EES side. During the tumor resection through EES, the surgical instruments from the cranial side are seen through the small defect of the diaphragma sellae. (f) Microscopic view after the removal of the port retractor at the end of the tumor resection. The trajectory injury is minimal, and the size of the trajectory is calculated from the width of the neurosheet in the picture; the length and width of the trajectory are 11.5 mm and 5.5 mm, respectively.
The direction of the port retractor was aiming to the most upper and dorsal part of the tumor, which was the most difficult area to reach from the endonasal side [
The port retractor was connected with the self-retaining Budde Halo Retractor System. Then, the tumor was confirmed beyond the foramen of Monro. Due to the obstructive hydrocephalus, the foramen of Monro was enlarged; therefore, the working space was sufficient for following the procedure through the foramen of Monro [
Combined EES and microscopic transventricular surgery using the port retractor system for tumor resection
Most of the tumor was resected mainly from the EES side, and the resection was assisted from the transventricular surgery side. After the incision of the sellar dura, a soft and fragile tumor, typical of a pituitary adenoma, was removed with a curette or by suction. After resection of the intrasellar part of the tumor, the suprasellar part was resected under visualization with a 30-degree angled scope. After the lower part of the tumor was debulked by ESS, the upper part gradually descended. During the descent of the tumor by ESS, on the craniotomy side, the adhered surrounding blood vessels or choroid plexus around the foramen of Monro were dissected from the tumor capsule or the diaphragma sellae (hereafter, the diaphragma) by means of bimanual dissection using a thin tip bipolar coagulator and suction [
After the tumor resection, the cortical damage by the port retractor was minimal [
Postoperatively, transient insufficiency of the adrenocortical axis and transient diabetes insipidus were encountered; therefore, supplement therapy was done for 3–6 months. The preoperatively presented insufficiency of the thyroid axis was unchanged after the surgery; thus, only levothyroxine was given at the 2-year follow-up after the surgery. The postoperative PRL level was 13.6 ng/ml at 2 months after the surgery. The preoperative cognitive dysfunction had completely resolved (MMSE: 29/30, HDS-R: 30/30), and the visual field was almost normalized 2 weeks after the surgery. The patient returned to normal work. The pathological diagnosis was pituitary adenoma with positive staining for LH and PRL. The MIB-1 labeling index was below 1%.
DISCUSSION
Despite recent advancements in EES, surgery for giant pituitary adenoma is still challenging. The mortality rate after EES for giant pituitary adenoma was reported as still being 5.5%.[
Combined microscopic TSS with microscopic transcranial surgery
Combined surgery using microscopic TSS and microscopic transcranial surgery was reported by Loyo et al.,[
Combined EES with microscopic transcranial surgery
Kuga et al.[
Combined EES and endoscopic supraorbital keyhole surgery
Nagata et al. reported the efficacy of combined endoscopic supraorbital keyhole surgery and EES for suprasellar lesions. Endoscopic use from above and below is promising and advantageous in terms of limited space interference between the nasal and transcranial sides and ergonomics for surgeons on both sides. However, the disadvantage of this method is that a supraorbital keyhole approach is not suitable for a giant adenoma with marked extension into the third ventricle, as in the present case.
Combined microscopic TSS and endoscopic transventricular surgery using ventriculoscope
Several reports have been published on combined EES and endoscopic transventricular surgery using a ventriculoscope.[
On the other hand, in our method of using microscopic transcranial surgery, we can assist from the transcranial side more effectively than in surgery using an endoscope because of the better maneuverability of the instruments.
Combined EES with microscopic transventricular surgery using a port retractor system
No reports have hitherto been published on EES and microscopic transventricular surgery using a port retractor system for a giant pituitary adenoma. The trajectory injury on the cerebral cortex can be minimized using a port retractor system for deep-seated intra-axial or intraventricular lesions.[
In this combined surgery, the advantage of ESS over microscopic transventricular surgery is that instrument maneuverability is better in EES because no factor limits surgical space such as port retractor or foramen Monro. In addition, as the lower part of the tumor is debulked by EES, the upper part gradually descends, therefore, the surgical procedure becomes easier by EES but more difficult through transventricular route as time goes by because the tumor gets closer to the EES side but become invisible from the transventricular side as the tumor descends to the direction of the sella. This can be understandable to see [
On the other hand, the advantage of the microscopic transventricular surgery over EES is the direct access to the upper and dorsal surface of the tumor, which cannot be observed by EES side. However, transventricular approach angle through the foramen of Monro to the upper and dorsal surface was very steep in this case, transchoroidal dissection posteriorly extending the foramen Monro was useful to facilitate to get access to this area.
CONCLUSION
For a giant pituitary adenoma with marked extension into the third ventricle, combined simultaneous EES and microscopic transventricular surgery is effective to maximize the extent of tumor resection while at the same time preventing complications. Using a port retractor system for the transcranial side, microscopic secure dissection is possible with minimum additional cortical damage.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors thank Dr. Alexander Zaboronok, Department of Neurosurgery, and Ms. F. Miyamasu of the Medical English Communications Center of the Faculty of Medicine, University of Tsukuba, for manuscript revision.
References
1. Akiyama Y, Wanibuchi M, Mikami M, Horita Y, Komatsu K, Suzuki K. Rigid endoscopic resection of deep-seated or intraventricular brain tumors. Neurol Res. 2015. 37: 278-82
2. Chabot DJ, Chakraborty S, Imbarrato G, Dehdashti AR. Evaluation of outcomes after endoscopic endonasal surgery for large and giant pituitary macroadenoma: A retrospective review of 39 consecutive patients. World Neurosurg. 2015. 84: 978-88
3. Charalampaki P, Ayyad A, Kockro RA, Perneczky A. Surgical complications after endoscopic transsphenoidal pituitary surgery. J Clin Neurosci. 2009. 16: 786-9
4. D’Haens J, Rompaey KV, Stadnik T, Haentjens P, Poppe K, Velkeniers B. Fully endoscopic transsphenoidal surgery for functioning pituitary adenomas: A retrospective comparison with traditional transsphenoidal microsurgery in the same institution. Surg Neurol. 2009. 72: 336-40
5. Greenfield JP, Leng LZ, Chaudhry U, Brown S, Anand VK, Souweidane MM. Combined simultaneous endoscopic transsphenoidal and endoscopic transventricular resection of a giant pituitary macroadenoma. Minim Invasive Neurosurg. 2008. 51: 306-9
6. Herrera SR, Shin JH, Chan M, Kouloumberis P, Goellner E, Slavin KV. Use of transparent plastic tubular retractor in surgery for deep brain lesions: A case series. Surg Technol Int. 2010. 19: 47-50
7. Hong CS, Prevedello DM, Elder JB. Comparison of endoscope-versus microscope-assisted resection of deep-seated intracranial lesions using a minimally invasive port retractor system. J Neurosurg. 2016. 124: 799-810
8. Juraschka K, Khan OH, Godoy BL, Monsalves E, Kilian A, Krischek B. Endoscopic endonasal transsphenoidal approach to large and giant pituitary adenomas: Institutional experience and predictors of extent of resection. J Neurosurg. 2014. 121: 75-83
9. Koktekir E, Karabagli H, Ozturk K. Simultaneous transsphenoidal and transventricular endoscopic approaches for giant pituitary adenoma with hydrocephalus. J Craniofac Surg. 2015. 26: e39-42
10. Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH. Endoscopic endonasal compared with microscopic transsphenoidal and open transcranial resection of giant pituitary adenomas. Pituitary. 2012. 5: 150-9
11. Koutourousiu M, Gardner PA, Fernandez-Miranda JC, Paluzzi A, Wang EW, Snyderman CH. Endoscopic endonasal surgery for giant pituitary adenomas: Advantages and limitations. J Neurosurg. 2013. 118: 621-31
12. Kuga D, Toda M, Ozawa H, Ogawa K, Yoshida K. Endoscopic endonasal approach combined with a simultaneous transcranial approach for giant pituitary tumors. World Neurosurg. 2019. 121: 173-9
13. Loyo M, Kleriga E, Mateos H, de Leo R, Delgado A. Combined supra-infrasellar approach for large pituitary tumors. Neurosurgery. 1984. 14: 485-8
14. McLaughlin N, Prevedello DM, Engh J, Kelly DF, Kassam AB. Endoneurosurgical resection of intraventricular and intraparenchymal lesions using the port technique. World Neurosurg. 2013. 79: S18-e1-8
15. Nagata Y, Watanabe T, Nagatani T, Takeuchi K, Chu J, Wakabayashi T. Fully endoscopic combined transsphenoidal and supraorbital keyhole approach for parasellar lesions. J Neurosurg. 2018. 128: 685-94
16. Nishioka H, Hara T, Usui M, Fukuhara N, Yamada S. Simultaneous combined supra-infrasellar approach for giant/ large multilobulated pituitary adenomas. World Neurosurg. 2012. 77: 533-9
17. Ojha BK, Husain M, Rastogi M, Chandra A, Chugh A, Husain N. Combined trans-sphenoidal and simultaneous trans-ventricular-endoscopic decompression of a giant pituitary adenoma: Case report. Acta Neurochir (Wien). 2009. 151: 843-7
18. Raza SM, Recinos PF, Avendono J, Adams H, Jallo GI, Quinones-Hinojosa A. Minimally invasive trans-portal resection of deep intracranial lesions. Minim Invasive Neurosurg. 2011. 54: 5-11
19. Romano A, Chibbaro S, Marsella M, Oretti G, Spiriev T, Iaccarino C. Combined endoscopic transsphenoidaltransventricular approach for resection of a giant pituitary macroadenoma. World Neurosurg. 2010. 74: 161-4