- Department of Neurosurgery, Umberto I General Hospital, Polytechnic University of Marche, Ancona, Italy
- Department of Oral and Head-Neck Surgery, Umberto I General Hospital, Polytechnic University of Marche, Ancona, Italy
- Department of Radiology, Section of Neuroradiology, Umberto I General Hospital, Polytechnic University of Marche, Ancona, Italy
Correspondence Address:
Maurizio Iacoangeli
Department of Neurosurgery, Umberto I General Hospital, Polytechnic University of Marche, Ancona, Italy
DOI:10.4103/2152-7806.173561
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Somma Ld, Iacoangeli M, Nasi D, Balercia P, Lupi E, Girotto R, Polonara G, Scerrati M. Combined supra-transorbital keyhole approach for treatment of delayed intraorbital encephalocele: A minimally invasive approach for an unusual complication of decompressive craniectomy. Surg Neurol Int 07-Jan-2016;7:
How to cite this URL: Somma Ld, Iacoangeli M, Nasi D, Balercia P, Lupi E, Girotto R, Polonara G, Scerrati M. Combined supra-transorbital keyhole approach for treatment of delayed intraorbital encephalocele: A minimally invasive approach for an unusual complication of decompressive craniectomy. Surg Neurol Int 07-Jan-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/combined-supra%e2%80%91transorbital-keyhole-approach-for-treatment-of-delayed-intraorbital-encephalocele-a-minimally-invasive-approach-for-an-unusual-complication-of-decompressive-craniectomy/
Abstract
Background:Intraorbital encephalocele is a rare entity characterized by the herniation of cerebral tissue inside the orbital cavity through a defect of the orbital roof. In patients who have experienced head trauma, intraorbital encephalocele is usually secondary to orbital roof fracture.
Case Description:We describe here a case of a patient who presented an intraorbital encephalocele 2 years after severe traumatic brain injury, treated by decompressive craniectomy and subsequent autologous cranioplasty, without any evidence of orbital roof fracture. The encephalocele removal and the subsequent orbital roof reconstruction were performed by using a modification of the supraorbital keyhole approach, in which we combine an orbital osteotomy with a supraorbital minicraniotomy to facilitate view and access to both the anterior cranial fossa and orbital compartment and to preserve the already osseointegrated autologous cranioplasty.
Conclusions:The peculiarities of this case are the orbital encephalocele without an orbital roof traumatic fracture, and the combined minimally invasive approach used to fix both the encephalocele and the orbital roof defect. Delayed intraorbital encephalocele is probably a complication related to an unintentional opening of the orbit during decompressive craniectomy through which the brain herniated following the restoration of physiological intracranial pressure gradients after the bone flap repositioning. The reconstruction of the orbital roof was performed by using a combined supra-transorbital minimally invasive approach aiming at achieving adequate surgical exposure while preserving the autologous cranioplasty, already osteointegrated. To the best of our knowledge, this approach has not been previously used to address intraorbital encephalocele.
Keywords: Decompessive craniectomy, intraorbital encephalocele, minimally invasive surgery, piezosurgery
INTRODUCTION
Intraorbital encephalocele is a rare entity characterized by the herniation of cerebral tissue inside the orbital cavity through a defect of the orbital roof.[
CASE REPORT
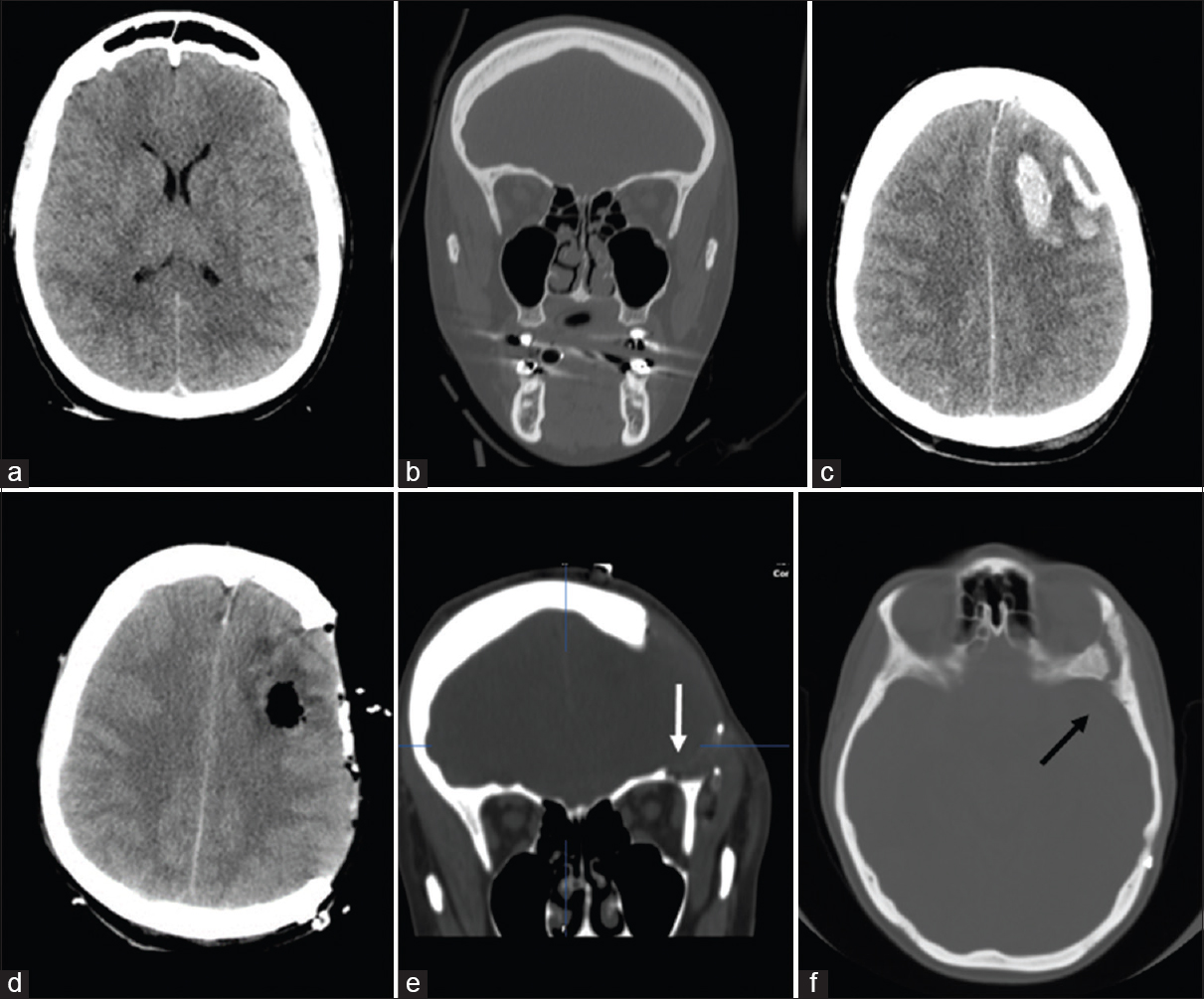
A 40-year-old female was admitted at our institution following a motor vehicle accident. The patient was unresponsive with a Glasgow Coma Scale (GCS) score of 6 (E1V1M4) and was put on mechanical ventilation. The pupils were bilaterally equal and reactive. She had no periorbital hematoma and no proptosis. Visual acuity and extraocular muscle motility of both eyes were not assessed because of the reduced level of consciousness of the patient. The immediate postinjury computed tomography (CT) scan showed only a mild, diffuse brain swelling [
Figure 1
(a and b) The immediate postinjury thin-slice computed tomography scan with coronal reconstruction showed generalized brain edema without left orbital roof fractures. (c) Computed tomography scan 24 h after trauma revealed a left-sided frontal contusion causing midline shift and increased diffuse brain swelling. (d and e) Postoperative computed tomography scan showing left decompressive craniotomy and evacuation of frontal contusion with a small bony defect in the roof of the orbit (see arrow) probably related to an unintentional opening of the orbit during keyhole burr hole without evidence of encephalocele. (f) Computed tomography scan after cranioplasty confirming the small bone opening on the orbital roof (see arrow)
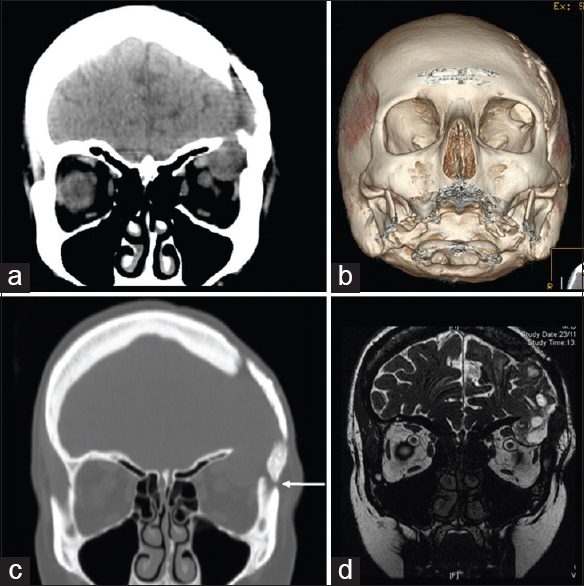
Two years following the last operation, the patient complained left fronto-orbital headache without any others ocular symptoms and/or signs, such as visual disturbance, proptosis, or pulsatile exophthalmos. 3D CT scan demonstrated the complete bone fusion of autologous cranioplasty, and no others intracranial complication. However, a thin-slice orbital CT sections with coronal reconstruction revealed the enlargement of the supero-lateral orbital roof defect with intraorbital encephalocele [Figure
Figure 2
(a-c) Thin-slice orbital computed tomography sections with three-dimensional and coronal reconstruction (2 years after the cranioplasty) revealed the enlargement of the lateral orbital roof bony defect associated with intraorbital encephalocele. The arrow indicates the burr hole, filled by autologous bone dust mixed with a bone substitute, too close to the orbital wall. (d) Magnetic resonance imaging image confirming the herniation of brain matter into the left orbit
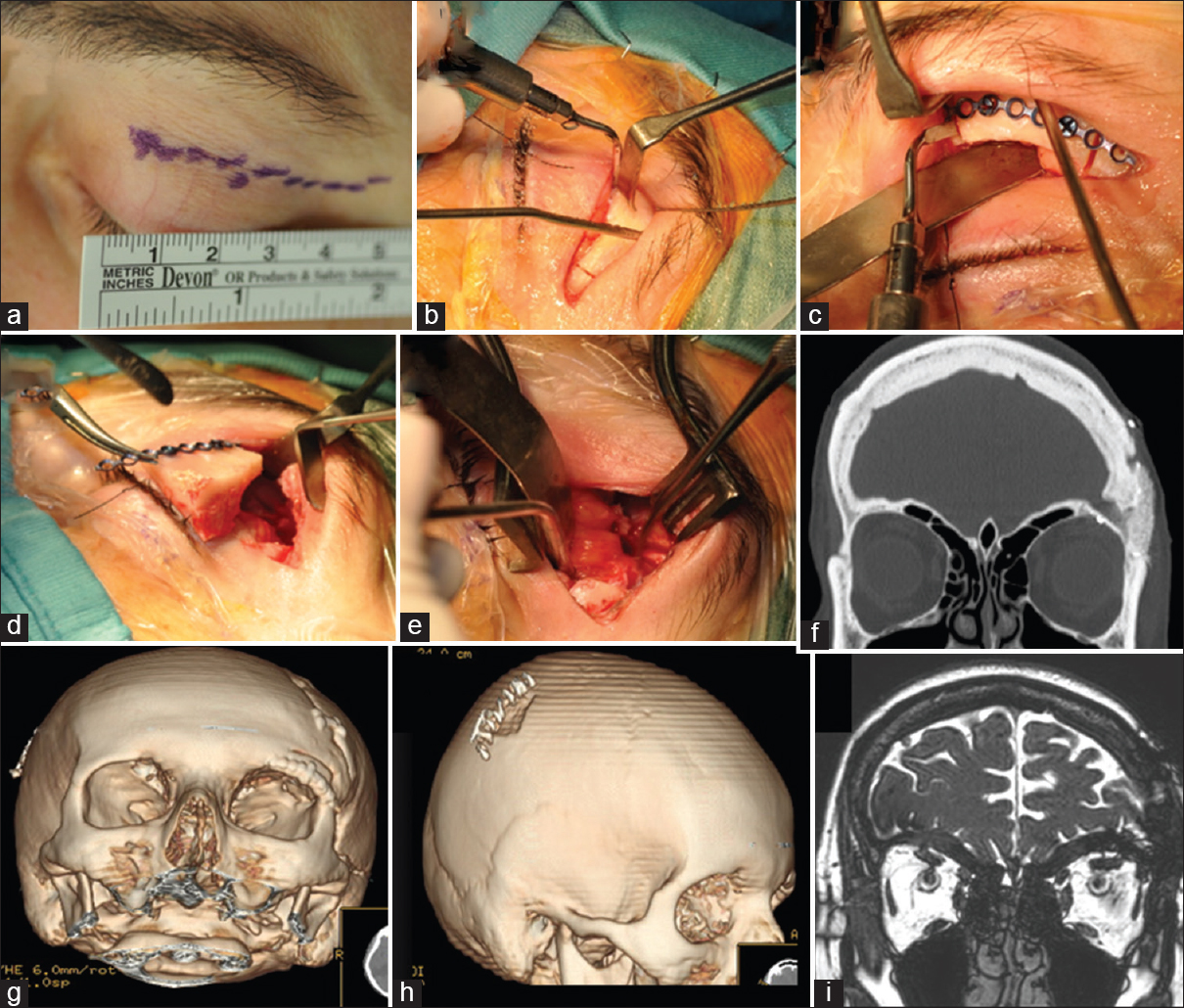
Figure 3
Abcdefghi: Intraoperative images and postoperative thin-slice computed tomography scan with three-dimensional reconstruction. (a) Left superior blepharoplasty incision. (b and c) Supra-transorbital keyhole approach with the combination of an orbital osteotomy with a supraorbital minicraniotomy. The use of piezoelectric scalpel allows to realize precise and thin osteotomies, for better future bone healing and better aesthetic result. (c and d) The one-piece bone flap includes the frontal bone, and the orbital rim using the defect of the orbital roof as the posterior edge of the orbitotomy. The one-piece bone flap was then fixed by titanium low-profile miniplate and screws. (e) Intraoperative working area with the exposure of both orbital and intracranial compartments. (f-i) Postoperative thin-slice computed tomography scan with three-dimensional reconstruction and magnetic resonance imaging showing left orbital roof reconstruction with autologous bone, obtained from the split calvarial parietal bone contralateral to the cranioplasty
DISCUSSION
Orbital encephalocele is a rare entity, and it is characterized by the herniation of part of the brain through a congenital, traumatic, neoplastic, or iatrogenic orbital roof defect.[
The main symptoms and signs of intraorbital encephalocele are diplopia, exophthalmos, orbital edema, subconjunctival hemorrhage, restricted movements of the eye, and loss of vision. Among these, pulsatile exophthalmos is the most reported symptom after traumatic intraorbital encephalocele in the literature.[
Excision of the herniated brain tissue, duraplasty, and reconstruction of the orbital roof are the key steps of surgery.[
CONCLUSIONS
The peculiarities of this case are the development of intraorbital encephalocele without evidence of traumatic orbital roof fracture and the combined supra-transorbital minimally invasive approach. The delayed intraorbital encephalocele is probably a complication related to an unintentional opening of the orbit during decompressive craniectomy through which the brain herniated following the restoration of physiological ICP gradients after the bone flap repositioning. The reconstruction of the orbital roof was performed by using a combined supra-transorbital minimally invasive approach aiming at achieving adequate surgical exposure while preserving the autologous cranioplasty, already osteointegrated. To the best of our knowledge, this approach has not been previously used to address intraorbital encephalocele.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Antonelli V, Cremonini AM, Campobassi A, Pascarella R, Zofrea G, Servadei F. Traumatic encephalocele related to orbital roof fractures: Report of six cases and literature review. Surg Neurol. 2002. 57: 117-25
2. Bruzek A, Shepherd D, Van Gompel J, Jentoft M. Pilocytic astrocytoma presenting as an orbital encephalocele: A case report. Case Rep Neurol. 2015. 7: 90-4
3. Cayli SR, Kocak A, Alkan A, Kutlu R, Tekiner A, Ates O. Intraorbital encephalocele: An important complication of orbital roof fractures in pediatric patients. Pediatr Neurosurg. 2003. 39: 240-5
4. Gazioglu N, Ulu MO, Ozlen F, Uzan M, Ciplak N. Acute traumatic orbital encephalocele related to orbital roof fracture: Reconstruction by using porous polyethylene. Ulus Travma Acil Cerrahi Derg. 2008. 14: 247-52
5. Iacoangeli M, Di Rienzo A, di Somma LG, Moriconi E, Alvaro L, Re M. Improving the endoscopic endonasal transclival approach: The importance of a precise layer by layer reconstruction. Br J Neurosurg. 2014. 28: 241-6
6. Iacoangeli M, Di Rienzo A, Nocchi N, Balercia P, Lupi E, Regnicolo L. Piezosurgery as a further technical adjunct in minimally invasive supraorbital keyhole approach and lateral orbitotomy. J Neurol Surg A Cent Eur Neurosurg. 2015. 76: 112-8
7. Iacoangeli M, Neri P, Balercia P, Lupi E, Di Rienzo A, Nocchi N. Piezosurgery for osteotomies in orbital surgery: Our experience and review of the literature. Int J Surg Case Rep. 2013. 4: 188-91
8. Jaiswal M, Sundar IV, Gandhi A, Purohit D, Mittal RS. Acute traumatic orbital encephalocele: A case report with review of literature. J Neurosci Rural Pract. 2013. 4: 467-70
9. Mohindra S, Mukherjee KK, Chhabra R, Gupta R. Orbital roof growing fractures: A report of four cases and literature review. Br J Neurosurg. 2006. 20: 420-3
10. Mokal NJ, Desai MF. Titanium mesh reconstruction of orbital roof fracture with traumatic encephalocele: A case report and review of literature. Craniomaxillofac Trauma Reconstr. 2012. 5: 11-8
11. Morihara H, Zenke K, Shoda D, Fujiwara S, Suehiro S, Hatakeyama T. Intraorbital encephalocele in an adult patient presenting with pulsatile exophthalmos.Case report. Neurol Med Chir (Tokyo). 2010. 50: 1126-8
12. Sahoo SK, Salunke PS, Ghuman MS. Traumatic orbital encephalocele in an infant: Using the fracture line to our advantage. Acta Neurochir (Wien). 2014. 156: 1357-9