- Department of Neurosurgery, Henry Ford Health System, Detroit, Michigan, United States.
DOI:10.25259/SNI_513_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Seokchun Lim, Sameah Haider, Hesham Zakaria, Victor Chang. Comparison of 30-day outcome following anterior cervical discectomy and fusion with or without instrumentation for cervical spondylosis: A review of 2352 elective cases. 13-Dec-2019;10:246
How to cite this URL: Seokchun Lim, Sameah Haider, Hesham Zakaria, Victor Chang. Comparison of 30-day outcome following anterior cervical discectomy and fusion with or without instrumentation for cervical spondylosis: A review of 2352 elective cases. 13-Dec-2019;10:246. Available from: https://surgicalneurologyint.com/surgicalint-articles/9801/
Abstract
Background: Anterior cervical discectomy and fusion (ACDF) is a commonly performed procedure to address cervical myeloradiculopathy. However, 30-day outcomes after additional plating/instrumentation are not very clear.
Methods: The authors reviewed The National Surgical Quality Improvement Program database to identify all elective ACDF cases with or without instrumentation for patients having cervical spondylosis with or without myelopathy from 2011 to 2013 using current procedural terminology and International Classification of Disease-9 codes. We identified 2352 cases and subdivided these into two cohorts based on instrumentation procedures (588 cases without instrumentation and 1764 cases with instrumentation). Baseline differences in two cohorts were adjusted by propensity score matching analysis, yielding well-matched 583 pairs.
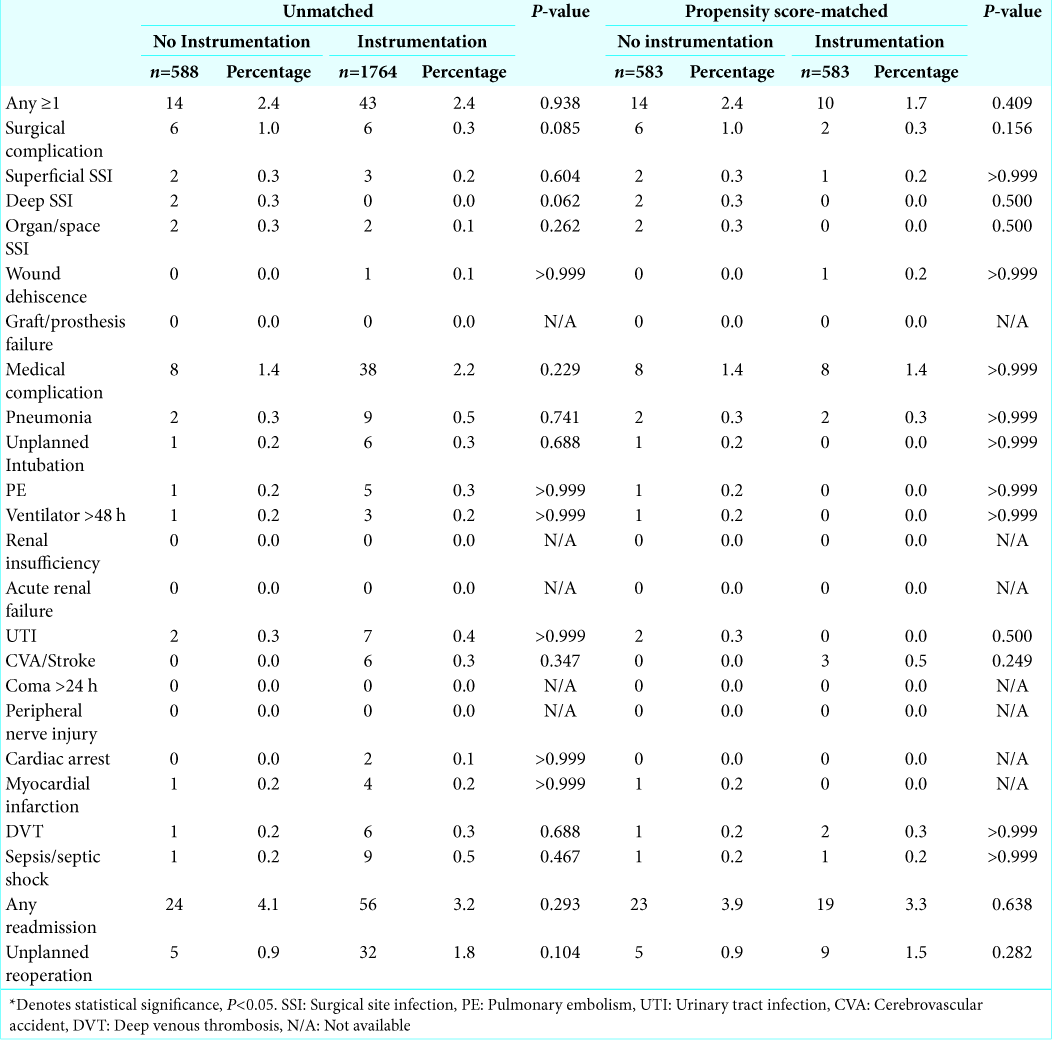
Results: Following propensity matching, the authors observed no significant difference in 30-day complication rates (prematch, 2.4% vs. 2.4%; and postmatch, 2.4% vs. 1.7%), readmission (prematch, 4.1% vs. 3.2%; and postmatch, 3.9% vs. 3.3%), and reoperation (prematch 0.9% vs. 1.8%; and postmatch 0.9% vs. 1.5%).
Conclusion: Our results demonstrate similar 30-day outcomes in both cohorts and suggest that instrumentation can be safely implemented in the setting of ACDF.
Keywords: Anterior cervical discectomy and fusion, Cervical spondylosis, Complication, Instrumentation, National Surgical Quality Improvement Program
INTRODUCTION
Cervical spondylosis is a common degenerative condition of the spine. It often correlates clinically with radiculopathy and less commonly, myelopathy. Anterior cervical discectomy and fusion (ACDF) is commonly utilized to address cervical myeloradiculopathy, although the role of additional plating/instrumentation is less clear.[
MATERIALS AND METHODS
Data acquisition
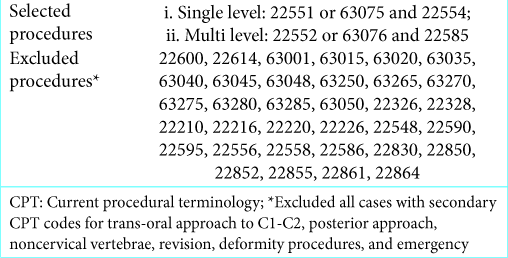
The authors reviewed the NSQIP database to identify all elective ACDF cases with or without instrumentation for patients with cervical spondylosis with or without myelopathy from 2011 to 2013. We utilized Current Procedural Terminology (CPT) and International Classification of Disease (ICD-9) codes to capture 2352 elective ACDF procedures [
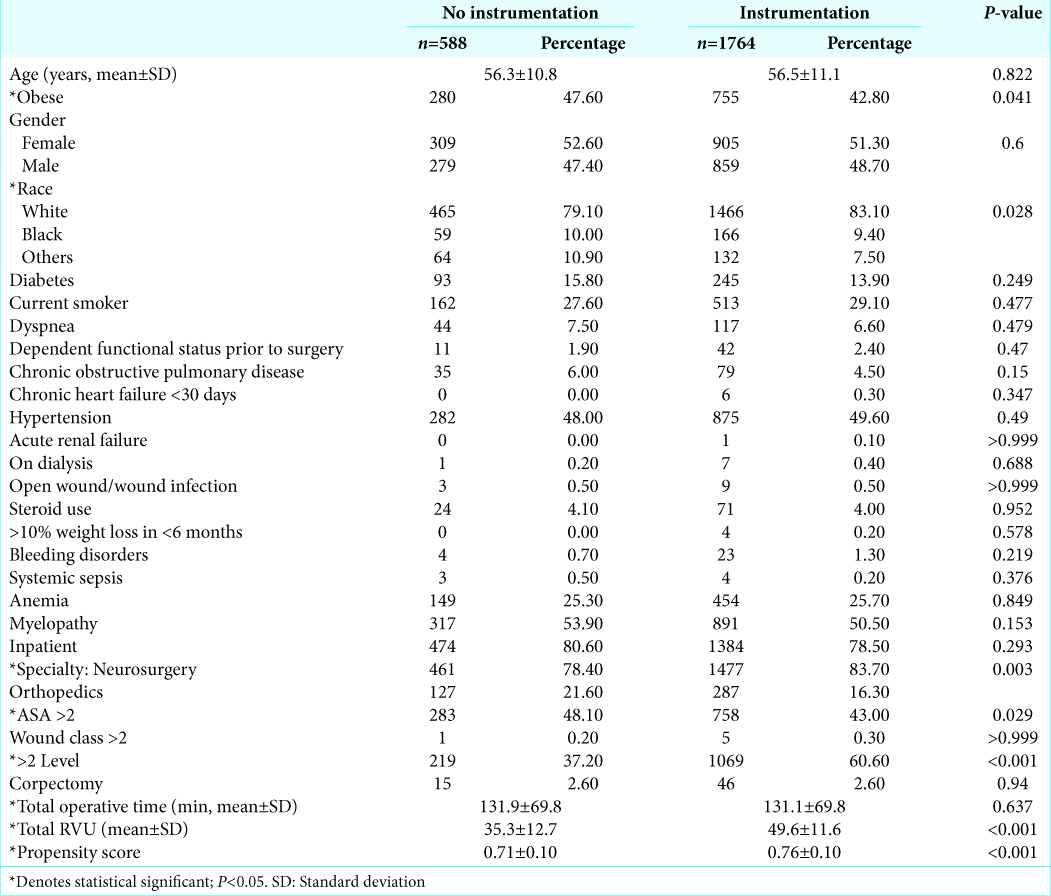
We tracked multiple demographic and operative variables for adequate propensity score matching analysis to compare 30-day postoperative outcomes following instrumented versus noninstrumented ACDF procedures [
Statistical analysis
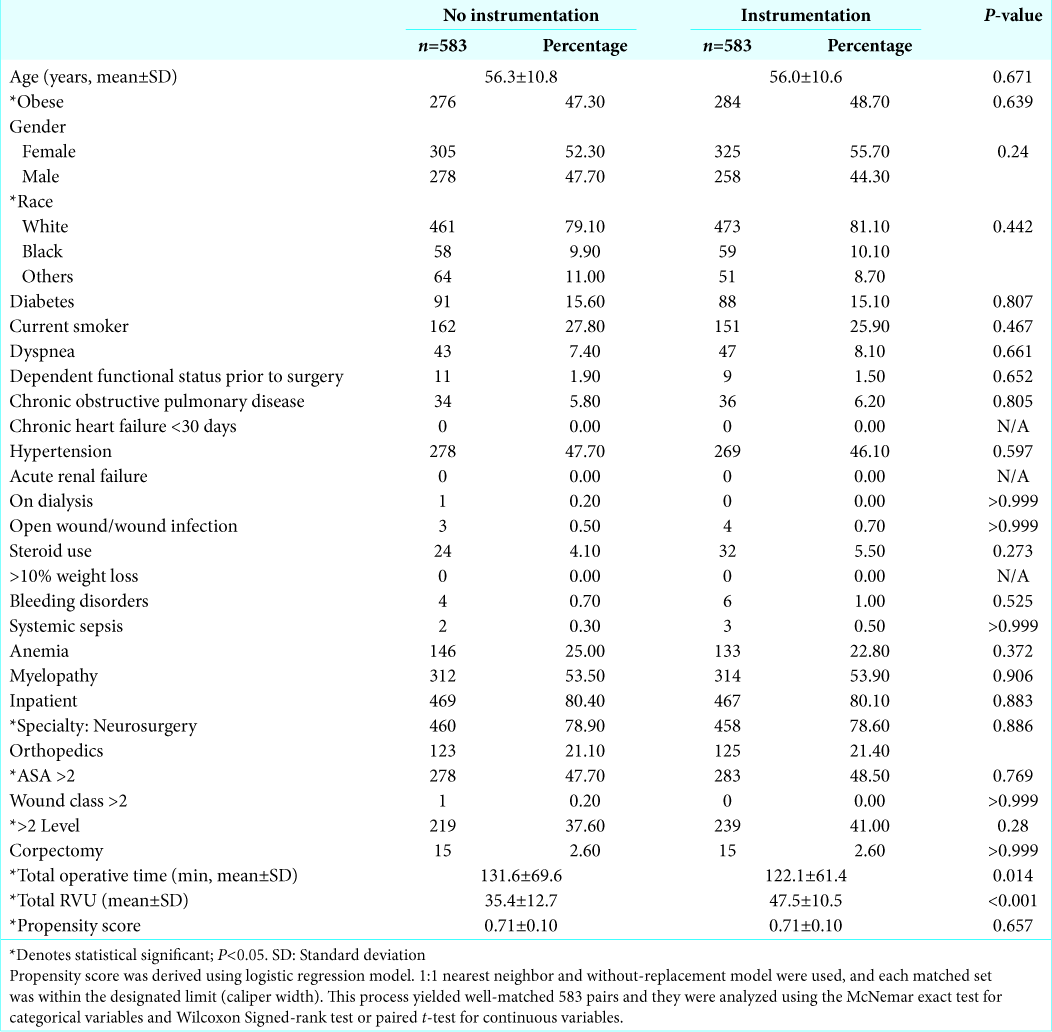
Continuous variables were compared using student t-test or Manny–Whitney U-test based on normality test. For categorical variables, we used Pearson’s Chi-square test or Fischer’s exact test. We also utilized propensity score matching analysis to adjust for baseline difference between two cohorts. This process yielded well-matched 583 pairs and they were analyzed using the McNemar exact test for categorical variables, and Wilcoxon Signed-rank test or paired t-test for continuous variables [
For all analyses performed in this study, we used IBM SPSS Statistics version 22.0 (IBM Corp., Armonk, NY).
RESULTS
Unadjusted dataset
Of the 2352 patients included in this study, 588 were in the noninstrumentation cohort and 1764 in the instrumentation cohort. Patients who had instrumentation were more likely to be obese, Caucasian, were neurosurgical cases, had lower ASA classifications, involved two or more levels, and had a higher total RVU value [
Propensity score-matched dataset
Propensity score matching yielded 583 well-matched cases. After matching, there was no significant baseline difference other than total operative duration and total RVU. The mean difference propensity scores between the two cohorts before and after matching were 0.05 and <0.001, respectively [
DISCUSSION
The authors relied on a prospectively maintained, national surgical database to assess how instrumentation may influence short-term postoperative outcome following single- and multi-level, elective ACDF for cervical spondylosis. This study sought to eliminate the baseline differences by utilizing a propensity score matching algorithm, which adjusted patient demographic profile, comorbidities, and major operative variables such as corpectomy or multi- level procedures. We further minimized procedural bias by selecting elective cases and tracking both individual CPT and ICD-9 codes.
Here, we demonstrated that patients in both noninstrumentation and instrumentation cohorts had comparable adverse outcome rates 30-day complication rates (prematch, 2.4% vs. 2.4%; and postmatch, 2.4% vs. 1.7%), readmission (prematch, 4.1% vs. 3.2%; and postmatch, 3.9% vs. 3.3%), and reoperation (prematch 0.9% vs. 1.8%; and postmatch 0.9% vs. 1.5%).
Complication and reoperation rates in this study were lower than previously reported rates, which were as high as 10%–13%.[
Our matched analysis also demonstrated that average operative duration was significantly longer than the noninstrumentation cohort (131.6 ± 69.6 vs. 122.1 ± 61.4; P = 0.014). However, 9-min difference in operative duration likely does not have any meaningful clinical influence despite the statistical difference arising from narrow standard deviation. This difference likely occurred during the matching process where operative duration was purposely not accounted for.
Here, we present a short-term multicenter analysis of outcomes following elective instrumented versus noninstrumented ACDF. We found similar 30-day outcomes in both cohorts which suggest that instrumentation can be safely implemented for ACDF resulting in comparable outcomes without incurring significant morbidity or adverse events.
CONCLUSION
Our analyses demonstrate similar 30-day outcomes in both cohorts, and suggest an additional instrumentation step can be safely implemented in the setting of cervical spondylosis with little concern for postoperative complication.
References
1. Adogwa O, Elsamadicy A, Reiser E, Ziegler C, Freischlag K, Cheng J. Comparison of surgical outcomes after anterior cervical discectomy and fusion: Does the intra-operative use of a microscope improve surgical outcomes. J Spine Surg. 2016. 2: 25-30
2. Bono CM, Ghiselli G, Gilbert TJ, Kreiner DS, Reitman C, Summers JT. An evidence-based clinical guideline for the diagnosis and treatment of cervical radiculopathy from degenerative disorders. Spine J. 2011. 11: 64-72
3. Bose B. Anterior cervical fusion using Caspar plating: Analysis of results and review of the literature. Surg Neurol. 1998. 49: 25-31
4. Cauthen JC, Kinard RE, Vogler JB, Jackson DE, DePaz OB, Hunter OL. Outcome analysis of noninstrumented anterior cervical discectomy and interbody fusion in 348 patients. Spine (Phila Pa 1976). 1998. 23: 188-92
5. Connolly PJ, Esses SI, Kostuik JP. Anterior cervical fusion: Outcome analysis of patients fused with and without anterior cervical plates. J Spinal Disord. 1996. 9: 202-6
6. Grob D, Peyer JV, Dvorak J. The use of plate fixation in anterior surgery of the degenerative cervical spine: A comparative prospective clinical study. Eur Spine J. 2001. 10: 408-13
7. Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002. 50: 229-36
8. Lad SP, Patil CG, Berta S, Santarelli JG, Ho C, Boakye M. National trends in spinal fusion for cervical spondylotic myelopathy. Surg Neurol. 2009. 71: 66-9
9. Mobbs RJ, Rao P, Chandran NK. Anterior cervical discectomy and fusion: Analysis of surgical outcome with and without plating. J Clin Neurosci. 2007. 14: 639-42
10. Randle MJ, Wolf A, Levi L, Rigamonti D, Mirvis S, Robinson W. The use of anterior Caspar plate fixation in acute cervical spine injury. Surg Neurol. 1991. 36: 181-9
11. Schneeberger AG, Boos N, Schwarzenbach O, Aebi M. Anterior cervical interbody fusion with plate fixation for chronic spondylotic radiculopathy: A 2-to 8-year follow-up. J Spinal Disord. 1999. 12: 215-20
12. Shapiro S. Banked fibula and the locking anterior cervical plate in anterior cervical fusions following cervical discectomy. J Neurosurg. 1996. 84: 161-5
13. Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP. The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine (Phila Pa 1976). 2009. 34: 2886-92
14. Wang JC, McDonough PW, Endow K, Kanim LE, Delamarter RB. The effect of cervical plating on single-level anterior cervical discectomy and fusion. J Spinal Disord. 1999. 12: 467-71
15. Wang JC, McDonough PW, Endow KK, Delamarter RB. Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2000. 25: 41-5
16. Xie JC, Hurlbert RJ. Discectomy versus discectomy with fusion versus discectomy with fusion and instrumentation: A prospective randomized study. Neurosurgery. 2007. 61: 107-16
17. Zoëga B, Kärrholm J, Lind B. One-level cervical spine fusion. A randomized study, with or without plate fixation, using radiostereometry in 27 patients. Acta Orthop Scand. 1998. 69: 363-8