- Department of Orthopaedic Surgery, Governador Celso Ramos Hospital, Florianopolis, Brazil,
- Clinical Laboratory for Bionic Extremity Reconstruction, Department of Plastic, Reconstructive and Aesthetic Surgery, Medical University of Vienna, Vienna, Austria
Correspondence Address:
Luana Caroline Miantti Ghellere Bonfim, Department of Orthopaedic Surgery, Governador Celso Ramos Hospital, Florianopolis, Brazil.
DOI:10.25259/SNI_570_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Luana Caroline Miantti Ghellere Bonfim1, Matthias E. Sporer2, Laura Poeta1, Gabriela Rezende R. Carvalho1, Jayme A. Bertelli1. Complete tibial nerve lesion secondary to postoperative popliteal pseudoaneurysm following anterior cruciate ligament arthroscopic reconstruction: A series of two patients. 01-Dec-2023;14:409
How to cite this URL: Luana Caroline Miantti Ghellere Bonfim1, Matthias E. Sporer2, Laura Poeta1, Gabriela Rezende R. Carvalho1, Jayme A. Bertelli1. Complete tibial nerve lesion secondary to postoperative popliteal pseudoaneurysm following anterior cruciate ligament arthroscopic reconstruction: A series of two patients. 01-Dec-2023;14:409. Available from: https://surgicalneurologyint.com/surgicalint-articles/12656/
Abstract
Background: Complications following arthroscopic anterior cruciate ligament reconstruction (ACLR) are rare, but injuries to the popliteal artery can occur. Popliteal pseudoaneurysms are a potential complication and can cause significant morbidity if not diagnosed and treated promptly.
Cases Description: We describe the cases of two patients who developed nerve injuries following arthroscopic ACLR, with subsequent diagnosis of a popliteal pseudoaneurysm. The peroneal nerve recovered spontaneously in both cases, while the tibial nerve was reconstructed using autologous nerve grafting. Satisfying, functional recoveries were observed 24 months postoperatively.
Conclusion: Prompt diagnosis and effective treatment of popliteal pseudoaneurysms are crucial to prevent further complications. However, timely diagnosis can be challenging due to inconsistent clinical presentations and a low index of suspicion. This case report highlights the need for increased awareness of this uncommon complication and provides insights into its pathophysiological mechanisms.
Keywords: Anterior cruciate ligament reconstruction, Autologous nerve grafting, Peripheral nerve injury, Popliteal pseudoaneurysm, Postoperative complication, Tibial nerve lesion
INTRODUCTION
Anterior cruciate ligament reconstruction (ACLR) is one of the most common orthopedic procedures, with approximately 100,000 patients undergoing reconstructive surgery in the US annually.[
Pseudoaneurysms of the popliteal artery are usually present with repeated hemarthrosis and a pulsatile mass within days to weeks after ACLR.[
In this article, we present two unique cases featuring neurotmesis of the tibial nerve and axonotmeses of the peroneal nerve caused by a postoperative, popliteal pseudoaneurysm following ACLR.
CASE DESCRIPTION
Case 1
A healthy, 34-year-old male patient had sustained a valgus trauma to his left knee, which resulted in a complete ACL rupture. A delayed arthroscopic reconstruction was scheduled 1 year after the injury. Immediately after surgery, the patient complained about severe pain and paresthesia, which irradiated to the popliteal fossa, his left calf, and foot. Some days later, a complete loss of dorsiflexion and plantar flexion of the ankle and foot manifested. First, a DVT was excluded by Doppler ultrasonography. A compartment syndrome was then suspected, and an emergency fasciotomy of the left leg was performed. Subsequently, the patient was discharged on the 10th postoperative day in an improved general condition, yet significantly restricted ankle and foot movement (overall M1 – British Medical Research Council [BMRC] scale).
On the 18th postoperative day, his pain worsened again, and complete paralysis of the dorsiflexion and plantar flexion of the foot arose. Moreover, a tingling sensation and numbness on the dorsal left leg and the plantar surface of the left foot persisted. An iatrogenic pseudoaneurysm of the popliteal artery was confirmed by angiography. An endovascular repair of the popliteal pseudoaneurysm was successfully performed with seven covered stents. The patient was discharged from the hospital without pain, yet no visible movement of his ankle or foot.
Approximately 3 months later, the patient was referred to our clinic due to ongoing neurologic symptoms. Clinical assessment revealed M0 ankle plantar flexion, M1 ankle eversion, dorsiflexion, and inversion (BMRC). In addition, the absence of foot sensation (S0) and a positive Tinel’s sign in the popliteal fossa were noted. Electrodiagnostic tests confirmed absent sensory potentials (superficial peroneal and sural nerve) and loss of motor function (peroneal and tibial nerve). These findings strongly indicated severe axonal injury, specifically of the neurotmesis variant, affecting the left tibial and common peroneal nerves at the juncture of the popliteal fossa. Consequently, a surgical nerve revision was scheduled.
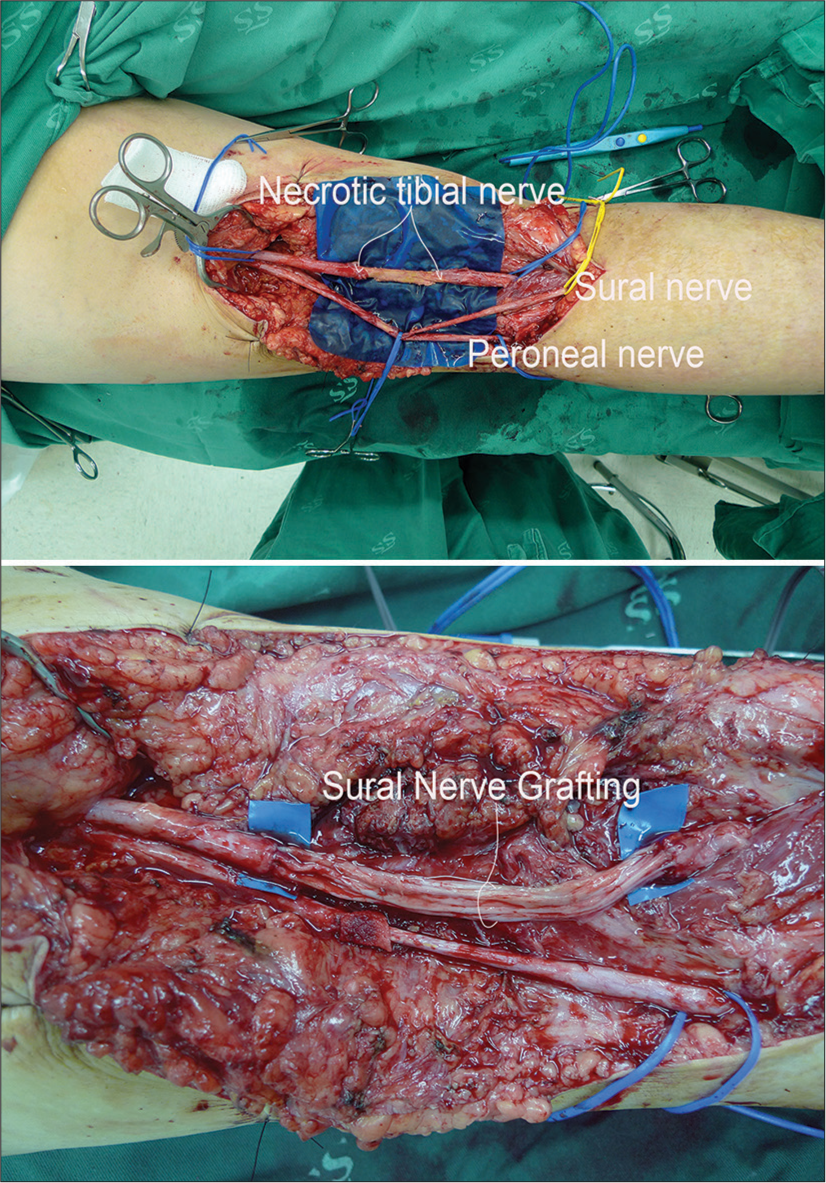
Intraoperatively, we confirmed the continuity of the peroneal and tibial nerves. However, a segment of the tibial nerve in the popliteal fossa was necrotic [
Figure 1:
Intraoperative pictures of case 1. First, the division of the sciatic nerve into its three branches (tibial, peroneal, and ultimately sural nerve) was dissected, and the nerves neurolyzed within the scar tissue of the popliteal fossa. The necrotic segment of the tibial nerve (upper panel) was resected until an intact fascicular structure was observed. The lower panel shows nerve repair using four, 11 cm strands of sural nerve grafts.
At the final follow-up, 24-month post nerve reconstruction, sensory improvements within the tibial nerve area were noted (S1). However, he also experienced dysesthesia while walking barefoot. Motor function exhibited recovery in ankle plantar flexion to M4 (BMRC), through toe plantar flexion remained absent. Dorsiflexion of both the foot and toes had improved to M4 and M2 (BMRC), respectively. Furthermore, visual inspection revealed persistent atrophy of the calf muscles.
Case 2
A 19-year-old female and healthy patient had sustained a valgus mechanism trauma on her left knee during skiing. As she was suffering from constant knee instability, the patient received an ACLR 3 years after the injury. Two days postoperatively, the patient started experiencing continuous popliteal pain radiating to the left leg and foot. Moreover, a pulsating mass and blister were noted at the popliteal fossa, and marked tenderness and swelling of the leg and foot [
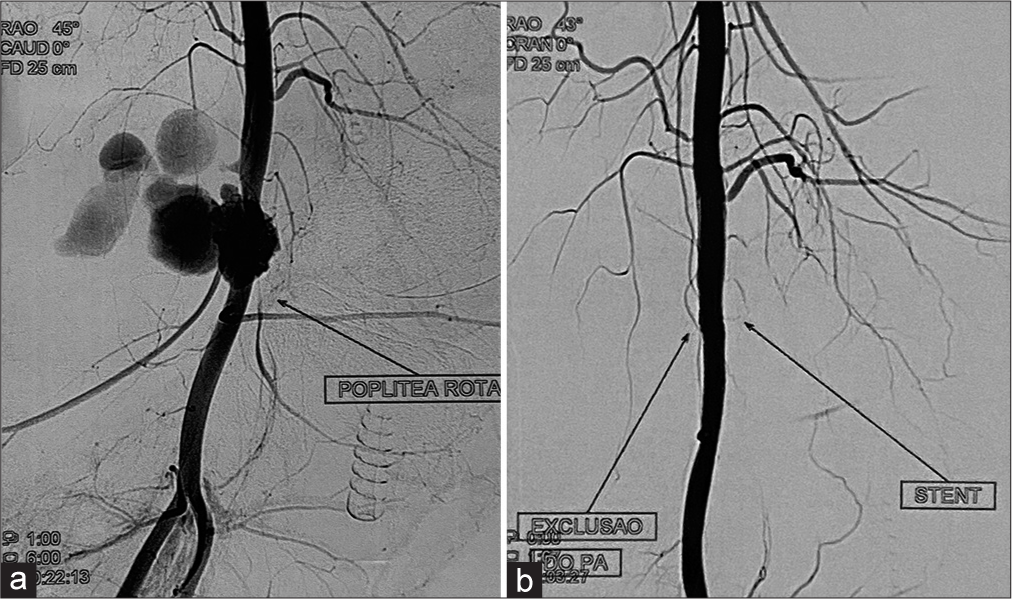
Figure 3:
(a) Magnetic resonance (MR) angiography confirmed a popliteal pseudoaneurysm. A laceration of the anterolateral wall resulted in the formation of a large unencapsulated and partially thrombosed pseudoaneurysm measuring 45 by 52 mm. The postoperative pseudoaneurysm caused secondary ischemic damage to the peroneal and tibial nerves. (b) MR angiography postintervention: following endovascular stent placement, showing normal flow across the popliteal artery.
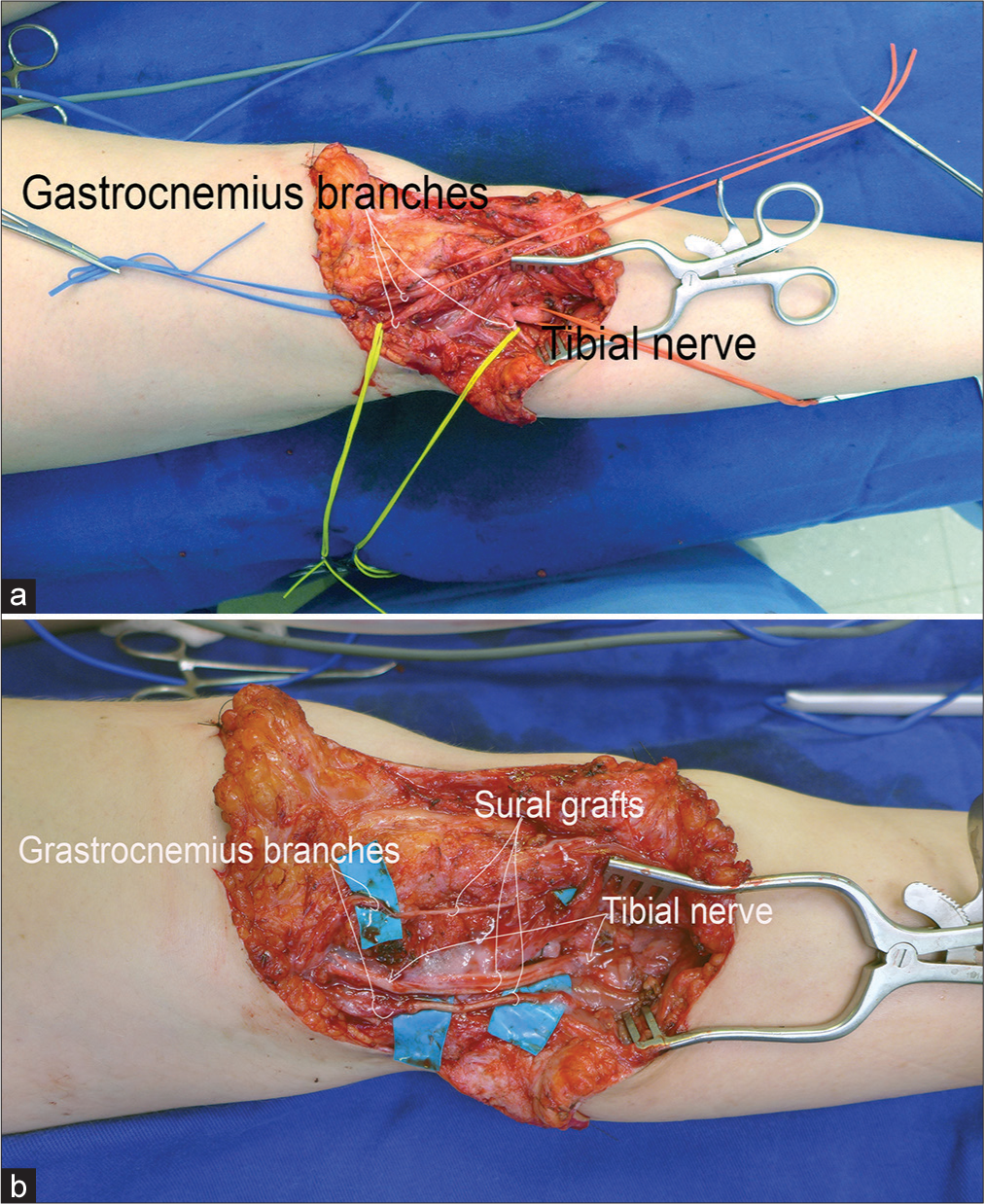
Because of persistent paralysis, electrodiagnostic studies were performed 3 and 9 months postoperatively. Twelve months after injury, the peroneal nerve recovered spontaneously (dorsiflexion of the foot and toes M3, S3), but paralysis of the tibial nerve persisted. Atrophy of the gastrocnemius muscles was evident, and the plantar flexion remained M0 (BMRC). Hence, an operative repair was scheduled. Intraoperatively, a complete tibial nerve rupture was verified and reconstructed with four strands of 6 cm sural nerve grafts harvested from the contralateral side [
Figure 4:
Intraoperative pictures of case 2. (a) Through a dorsal zigzag incision in the popliteal fossa, the tibial nerve and its branches to the gastrocnemius muscle were individually dissected. (b) The severed tibial nerve and both muscular branches were reconstructed by a sural nerve graft harvested from the contralateral leg.
At the last follow-up 24 months after the nerve reconstruction, the patient reported significant improvements in sensory disturbances related to the tibial nerve area. She could perceive tactile sensations, with heightened unpleasant sensations when encountering certain stimuli like uneven surfaces (S2). Her motor recovery demonstrated improvements in plantar and dorsi flexion to M4 (BMRC), while toe flexion was still absent. Notably, inspection revealed the persistence of calf muscle atrophy.
DISCUSSION
We present two secondary tibial nerve injuries following ACLR as a long-term complication. The delayed diagnosis of popliteal pseudoaneurysms resulted in prolonged compression, which caused permanent nerve damage in the discussed cases. Hence, we especially emphasize the importance of considering this potential complication after ACLR.
Although ACLR is considered a safe procedure with low complication rates,[
Clinical presentation of popliteal pseudoaneurysms usually involves pain, paresthesia, pulsating calf edema, and/or a palpable mass in the popliteal fossa.[
Although nerves are relatively resistant to ischemia, sustained stretch and compressive forces can result in secondary ischemic damage.[
Injury to the peroneal nerve results in characteristic foot drop and sensory deficits of the dorsal foot. However, as in the presented cases, spontaneous recovery is observed in 76%–87% of peroneal nerve injuries within 4–6 months.[
Considering that both patients achieved satisfying ankle plantar flexion, whether the age difference (19 vs. 34 years) or the delay in reconstruction (3 vs. 12 months) significantly influenced regeneration remains unsolved.
CONCLUSION
Although complications following ACLR are rare, a profound understanding of the pathophysiologic processes is essential for adequate management of potential sequelae. Due to ambiguous clinical presentation, prolonged compression by the popliteal pseudoaneurysms resulted in secondary peroneal and tibial nerve damage. The correct and timely diagnosis was a major challenge in both cases. Especially the combination of vascular and neurologic symptoms might have been misleading.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Amadei F, Basile G, Leigheb M. Nerve lesions during arthroscopic procedure: A literature overview. Orthop Rev (Pavia). 2021. 13: 24441
2. Ammori MB, Evans AR, Mclain AD. Popliteal artery pseudoaneurysm after total knee arthroplasty. J Arthroplasty. 2016. 31: 2004-7
3. Bernardi G, Tudisco C. Transient common peroneal and tibial nerve palsy following knee arthroscopy for the treatment of discoid lateral meniscus. Joints. 2017. 5: 118-20
4. Complications in arthroscopy: The knee and other join. Committee on Complications of the Arthroscopy Association of North America. Arthroscopy. 1986. 2: 253-8
5. De Lee J. Complications of arthroscopy and arthroscopic surgery: Results of a national survey. Arthroscopy. 1985. 1: 214-20
6. Grant GA, Goodkin R, Kliot M. Evaluation and surgical management of peripheral nerve problems. Neurosurgery. 1999. 44: 825-39
7. Jameson SS, Dowen D, James P, Serrano-Pedraza I, Reed MR, Deehan D. Complications following anterior cruciate ligament reconstruction in the English NHS. Knee. 2012. 19: 14-9
8. Janssen RP, Reijman M, Janssen DM, van Mourik JB. Arterial complications, venous thromboembolism and deep venous thrombosis prophylaxis after anterior cruciate ligament reconstruction: A systematic review. World J Orthop. 2016. 7: 604-17
9. Janssen RP, Sala HA. Embolism of the popliteal artery after anterior cruciate ligament reconstruction: A case report and literature review. Knee Surg Sports Traumatol Arthrosc. 2007. 15: 1449-51
10. Janssen RP, Scheltinga MR, Sala HA. Pseudoaneurysm of the popliteal artery after anterior cruciate ligament reconstruction with bicortical tibial screw fixation. Arthrosc J Arthrosc Relat Surg. 2004. 20: E4-6
11. Johnson DS, Sharma DP, Bangash IH. Common peroneal nerve palsy following knee arthroscopy. Arthroscopy. 1999. 15: 773-4
12. Kim DH, Ryu S, Tiel RL, Kline DG. Surgical management and results of 135 tibial nerve lesions at the Louisiana State University Health Sciences Center. Neurosurgery. 2003. 53: 1114-24
13. Kim TK, Savino RM, McFarland EG, Cosgarea AJ. Neurovascular complications of knee arthroscopy. Am J Sports Med. 2017. 30: 619-29
14. Krivić A, Stanec S, Zic R, Budi S, Milanović R, Stanec Z. Lesion of the common peroneal nerve during arthroscopy. Arthroscopy. 2003. 19: 1015-8
15. Lundborg G, editors. Nerve injury and repair. New York: Churchill Livingstone; 1988. p. 64-101
16. Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: Trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009. 91: 2321-8
17. Noorpuri BS, Maxwell-Armstrong CA, Lamerton AJ. Pseudo-aneurysm of a geniculate collateral artery complicating total knee replacement. Eur J Vasc Endovasc Surg. 1999. 18: 534-5
18. Peicha G, Pascher A, Schwarzl F, Pierer G, Fellinger M, Passler JM. Transsection of the peroneal nerve complicating knee arthroscopy: Case report and cadaver study. Arthroscopy. 1998. 14: 221-3
19. Qiu CS, Hanwright PJ, Khavanin N, Tuffaha SH. Functional reconstruction of lower extremity nerve injuries. Plast Aesthetic Res. 2022. 9: 19
20. Rodeo SA, Sobel M, Weiland AJ. Deep peroneal-nerve injury as a result of arthroscopic meniscectomy. A case report and review of the literature. J Bone Joint Surg Am. 1993. 75: 1221-4
21. Roganović Z, Misović S, Kronja G, Savić M. Peripheral nerve lesions associated with missile-induced pseudoaneurysms. J Neurosurg. 2007. 107: 765-75
22. Small NC. Complications in arthroscopic surgery of the knee and shoulder. Orthopedics. 1993. 16: 985-8
23. Soto JA, Múnera F, Morales C, Lopera JE, Holguín D, Guarín O. Focal arterial injuries of the proximal extremities: Helical CT arteriography as the initial method of diagnosis. Radiology. 2001. 218: 188-94
24. Wendt MC, Spinner RJ, Shin AY. Iatrogenic transection of the peroneal and partial transection of the tibial nerve during arthroscopic lateral meniscal debridement and removal of osteochondral fragment. Am J Orthop (Belle Mead NJ). 2014. 43: 182-5