- Department of Neurosurgery, Salford Royal Hospital, Stott Lane, Salford, Manchester, M6 8HD, England, United Kingdom.
DOI:10.25259/SNI_43_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mazhar Iqbal, K. Joshi George. Considerations in revising occipitocervical fixation for dysphagia. 30-Mar-2021;12:135
How to cite this URL: Mazhar Iqbal, K. Joshi George. Considerations in revising occipitocervical fixation for dysphagia. 30-Mar-2021;12:135. Available from: https://surgicalneurologyint.com/surgicalint-articles/10672/
Abstract
Background: Dysphagia after occipitocervical fixation (OCF) is a complex phenomenon and revision surgery in this context involves difficult decision-making. The pathogenesis is explored and surgical strategies discussed. A surgical strategy that has not been described before in the management of this condition, is discussed with two illustrative cases.
Methods: Two cases are presented where dysphagia occurred after OCF for C1/C2 instability. The preoperative imaging was not available to determine whether the optimal craniocervical angle had been achieved. Both had revision surgery with removal of the cranial fixation and fusion to the atlas instead. One of the cases had the revision surgery more than 10 years after the original OCF.
Results: The dysphagia recovered after the revision surgery in both cases. The patients gained weight and reported more satisfaction with their posture and head movements compared to before the revision surgery. There was no head ptosis and instead, patients reported better forward gaze and head position.
Conclusion: In cases of C1/C2 instability, it is preferable to perform C1/C2 fusion rather than OCF. If performing an OCF, care must be taken to fix the head at the same O-C2 angle as preoperative. When an OCF done for C1 C2 instability ends up causing dysphagia, it is feasible and effective to shorten the rostral construct by removing the cranial fixation and fusing to C1 instead.
Keywords: Atlantoaxial fixation, Dysphagia, Occipitocervical fixation
INTRODUCTION
Occipitocervical fixation (OCF) is a commonly performed operation for rheumatoid arthritis, tumor, and trauma involving the upper cervical spine and craniocervical junction. Some surgeons prefer to perform the rostral fixation to the occiput rather than to the atlas even when the instability is between C1 and C2.[
Dysphagia after OCF is an uncommon but increasingly recognized complication. It is thought to arise from fixing the neck in flexed or chin tuck position which results in a decreased oropharyngeal space and the inability of the spine to move during the swallowing phase.
To fix the neck in the optimum position while performing OCF is not easy and there are reports of swallowing problems even when the OCF is done in an ideal position.[
It is unclear as to what the ideal strategy is when a patient develops swallowing problems after OCF. Some surgeons go for revision surgery with aim of recontouring the rod to fix the head in a more extended position. Unfortunately, even this does not effectively address the swallowing problems as one of our illustrative cases show. If the preoperative imaging is not available, then it is difficult to gauge the ideal position that the head must be fixed in.
Removing the cranial fixation part is an option to address this but has not been previously described. There is a theoretical danger that the posterior craniocervical extensor muscles would have weakened and can no longer support the head in an extended position.
This can result in head ptosis or dropped head.
We present two cases whereby revision surgery was done by removing the cranial fixation component and fusing instead to the atlas, which led to a successful resolution of the swallowing problem. One of the cases had the revision surgery more than 10 years after the original surgery.
CASE PRESENTATIONS
Case 1
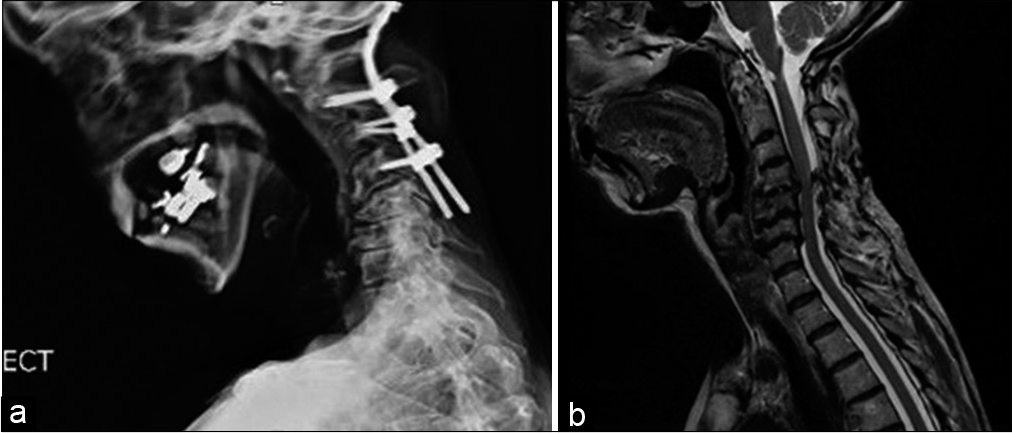
A 48-year-old lady was referred from another center. She had initially presented there with juvenile arthritis leading to C1/ C2 subluxation and basilar invagination. She had surgery in the form of an OCF with fixation from the occiput to C4 [
She presented to us 2 years later. She had difficulty in swallowing both solids and liquids but did not have any cranial nerve deficit. A barium swallow study did not find any obstructive pathology and showed moderate gastroesophageal reflux. Neurophysiology studies did not reveal any hypoglossal nerve injury. Initial strategy was to try and recontour the rods into a more favorable occipitocervical angle. However, the preoperative imaging was unavailable for us to calculate the optimal occipitocervical angle. Although there was concern about a postoperative head ptosis, after discussion with the patient, we decided to remove the cranial fixation and convert the construct to a C1/C2 fusion. An anomalous vertebral artery prevented a traditional C1 lateral mass fixation but allowed a transarticular screw trajectory.
We removed the OCF rod and inserted a C1/C2 transarticular screw with onlay of bone graft to provide fusion mass [
She was mobilized as able postoperatively without any collar. The patient’s swallowing problems improved immediately after the revision surgery. She put on 6 kilos of weight in 6 months after the surgery. She was also much happier about her head position and forward gaze. She revealed that she could now wear heels, enjoy a glass of wine, as well as look at her grandchild’s face when holding him, none of which she had been able to do before. She was discharged after 1 year of follow-up.
Case 2
A 71-year-old lady with rheumatoid arthritis and ischemic heart disease presented with neck pain, myelopathy, radiculopathy, and drooping of her head. She had OCF to C4 in 2006 for atlantoaxial instability. She developed severe dysphagia postoperative and needed nasogastric tube feeding. Three months later, she had revision surgery with realignment of the occipitocervical angle and fixation of the head in a more extended position than before. The dysphagia improved to the point that she was able to tolerate oral feed but she still had swallowing problems.
Twelve years later, she presented to us with difficulty in swallowing solids and liquids and drooping of the head. She also had brachalgia and paresthesia down both upper limbs with early myelopathic features on examination but no cranial nerve deficits. She weighed only 42 kilos. Imaging revealed that she had developed subluxation below the level of the OC fix at C4/5 with cord compression with foraminal stenosis at C5/6 and C6/7 levels [
A video fluoroscopy swallow study was performed. This showed no obstructive pathology but there was an abnormality in the pharyngeal stage of swallow. Hyoid tilt and elevation were reduced leading to incomplete laryngeal elevation, epiglottal flip, and cricopharyngeal sphincter opening. With thin fluids, laryngeal penetration was seen during the swallow under epiglottis.
We undertook a two-stage procedure to deal with cord compression, improve the brachalgia, and also to improve her dysphagia and dropped head.
She initially underwent an anterior procedure with C4 to C7 anterior cervical discectomy and fixation and plate.
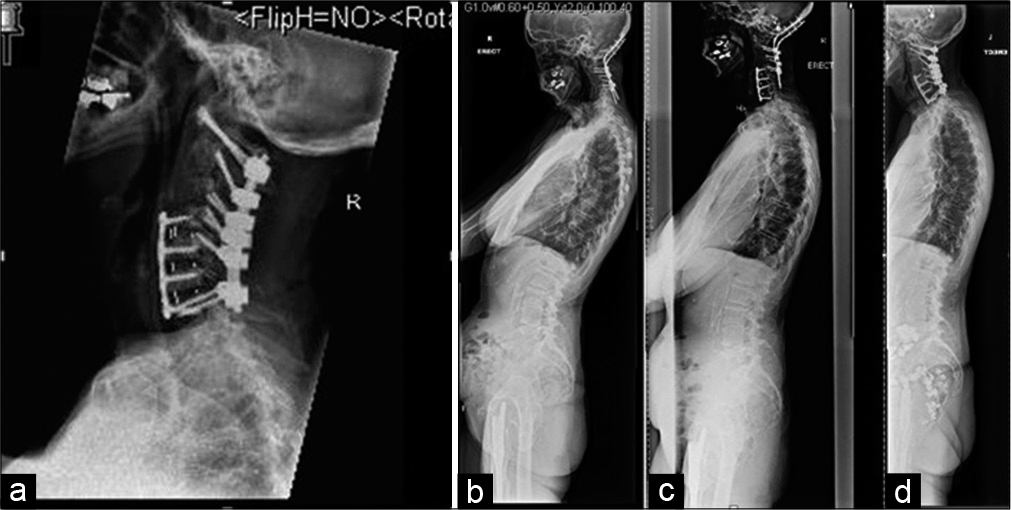
Two weeks later, she had the second-stage operation with a posterior approach. The cranial fixation was removed, and she had C1 to C7 instrumented fusion with onlay bone graft [
Figure 4:
(a) Case 2 postoperative lateral X-ray cervical spine showing removal of the cranial fixation and C4 to C7 anterior cervical discectomy and plate and posterior C1 to C7 fixation (b-d) Case 2 lateral X-ray whole spine showing how the alignment of the whole spine also improves from before revision surgery, after the first stage and then after the second stage. The head is also no longer drooped after the revision surgery.
She was mobilized with an Aspen postoperatively. Collar was gradually weaned off after recovery from surgery. However, a custom-made cervical orthoses were provided for use whenever she was out of the house.
Postoperatively, her myelopathy and brachalgia improved. Her dysphagia improved gradually and in fact she gained 8 kilos in 6 months after surgery. The patient also reported improved posture and much better head position and forward gaze [
DISCUSSION
As early as in 1927, Forester first performed occipitocervical reconstruction using a fibular strut graft.[
Dysphagia after OCF is an uncommon but increasingly recognized phenomenon.[
While dysphagia from most of the above causes fortunately resolves within a few weeks, dysphagia which results from fixed craniocervical malalignment tends to persist. Morishima et al.[
Takami et al.[
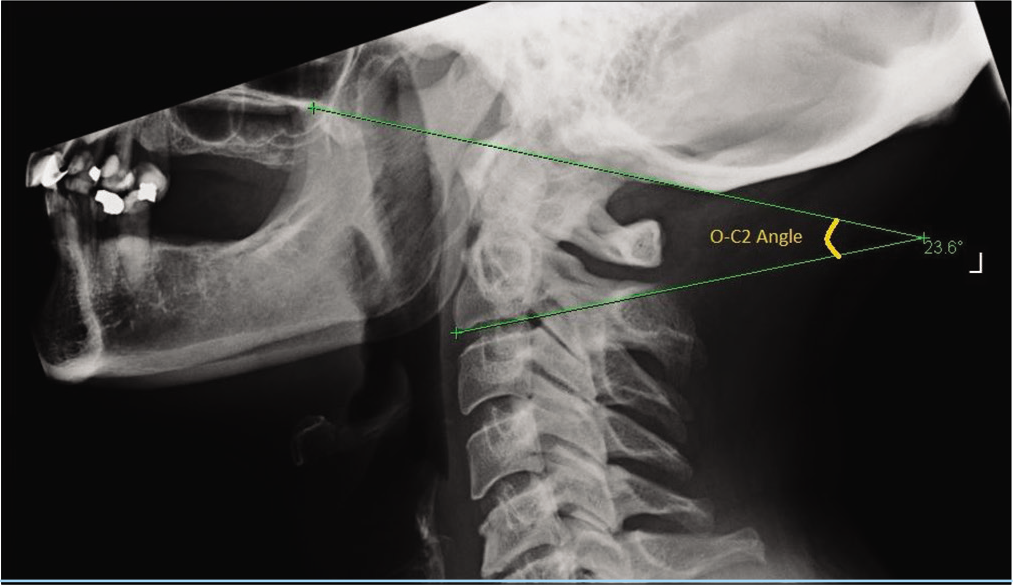
To increase exposure, the craniocervical junction may be malpositioned in a hyperflexed position for a better exposure and for a convenient angle for screw placement, which, in turn, results in a decrease of the O-C2 angle postoperatively.
Only a small decrease in O-C2A could result in an obvious reduction in the oropharyngeal space which, in turn, could impose a significant impact on the development of dysphagia.[
If the preoperative imaging is not available, then it becomes difficult to calculate the optimal O-C2 angle during the revision surgery. There is then a danger that revision surgery with just recontouring of the rod to fix the head in a different position may not improve the dysphagia.
There are also reports of swallowing problems even when the OCF is done in an ideal position.[
There are other disadvantages to an OCF. Long-term follow-up has indicated that improper occipitocervical angles not only caused clinical dissatisfaction among patients with neck stiffness and pain, limitation of neck activity, but may also cause poor fusion and abnormalities of the lower cervical curvature and accelerated degeneration.[
Some surgeons prefer occipitoaxial or OCF in atlantoaxial instability because it is technically relatively easier to perform and is relatively risk free compared with direct exposure of the facets of atlas and axis and atlantoaxial facet fixation.
However, Goel suggested that inclusion of the occipital bone for fixation of the atlantoaxial joint results in a suboptimally strong construct and should be avoided.[
The possibility of implant failure has been noted to be significantly higher in cases where OCF rather than atlantoaxial fixation was done.[
For all the above reasons, it seems reasonable to try and remove the cranial fixation if possible, during revision of OCF for atlantoaxial instability.
However, shortening the OCF to atlantoaxial fixation carries some risks. There may be degeneration which has developed in a previously fixed segment and this might cause severe pain when the segment then becomes mobile.
Furthermore, the posterior craniocervical muscles may have weakened and may not be strong enough to support the head in extension after removal of the cranial fixation.
However, the two cases we described have had a very good clinical result with improvement in their posture and head position in addition to improvement of their dysphagia, after removal of the cranial fixation. By allowing free movement of the head in relation to the cervical spine, the oropharyngeal space is restored and it is likely that the tongue and upper pharyngeal muscles can operate normally, all of which together improve dysphagia. No significant weakness of the head extensor muscles or head ptosis has been noticed by the patients and in fact both have good horizontal gaze.
We hope that this discussion will help the decision-making process if one faces this complex problem.
CONCLUSION
In cases of C1/C2 instability, it is preferable to perform C1/C2 fusion rather than OCF. If performing an OCF, care must be taken to fix the head at the same O-C2 angle as preoperative. When an OCF done for C1 C2 instability ends up causing dysphagia, it is feasible and effective to shorten the rostral construct by removing the cranial fixation and fusing to C1 instead.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Garrido BJ, Sasso RC. Occipitocervical fusion. Orthop Clin North Am. 2012. 43: 1-9
2. Goel A. Letter: Occipitocervical fixation: A single surgeon’s experience with 120 patients. Neurosurgery. 2017. 80: E263-4
3. Goel A. Occipitocervical fixation: Is it necessary?. J Neurosurg Spine. 2010. 13: 1-2
4. He B, Yan L, Xu Z, Chang Z, Hao D. The causes and treatment strategies for the postoperative complications of occipitocervical fusion: A 316 cases retrospective analysis. Eur Spine J. 2014. 23: 1720-4
5. Huang M, Gonda DD, Briceño V, Lam SK, Luerssen TG, Jea A. Dyspnea and dysphagia from upper airway obstruction after occipitocervical fusion in the pediatric age group. Neurosurg Focus. 2015. 38: E13
6. Inada T, Furuya T, Kamiya K, Ota M, Maki S, Suzuki T. Postoperative increase in occiput-C2 angle negatively impacts subaxial lordosis after occipito-upper cervical posterior fusion surgery. Asian Spine J. 2016. 10: 744-7
7. Izeki M, Neo M, Takemoto M, Fujibayashi S, Ito H, Nagai K. The O-C2 angle established at occipito-cervical fusion dictates the patient’s destiny in terms of postoperative dyspnea and/or dysphagia. Eur Spine J. 2014. 23: 328-36
8. Kaneyama S, Sumi M, Takabatake M, Kasahara K, Kanemura A, Hirata H. The prediction and prevention of dysphagia after occipitospinal fusion by use of the S-line (swallowing line). Spine (Phila Pa 1976). 2017. 42: 718-25
9. Matsuyama Y, Kawakami N, Yoshihara H, Tsuji T, Kamiya M, Yukawa Y. Long-term results of occipitothoracic fusion surgery in RA patients with destruction of the cervical spine. J Spinal Disord Tech. 2005. 18: S101-6
10. Meng Y, Chen H, Lou J, Rong X, Wang B, Deng Y. Posterior distraction reduction and occipitocervical fixation for the treatment of basilar invagination and atlantoaxial dislocation. Clin Neurol Neurosurg. 2016. 140: 60-7
11. Meng Y, Wu T, Liu Z, Wen D, Rong X, Chen H. The impact of the difference in O-C2 angle in the development of dysphagia after occipitocervical fusion: A simulation study in normal volunteers combined with a case-control study. Spine J. 2018. 18: 1388-97
12. Miyata M, Neo M, Fujibayashi S, Ito H, Takemoto M, Nakamura T. O-C2 angle as a predictor of dyspnea and/or dysphagia after occipitocervical fusion. Spine (Phila Pa 1976). 2009. 34: 184-8
13. Morishima N, Ohota K, Miura Y. The influences of halo-vest fixation and cervical hyperextension on swallowing in healthy volunteers. Spine (Phila Pa 1976). 2005. 30: E179-82
14. Ota M, Neo M, Aoyama T, Ishizaki T, Fujibayashi S, Takemoto M. Impact of the O-C2 angle on the oropharyngeal space in normal patients. Spine (Phila Pa 1976). 2011. 36: E720-6
15. Sindgikar P, Das KK, Sardhara J, Bhaisora KS, Srivastava AK, Mehrotra A. Craniovertebral junction anomalies: When is resurgery required?. Neurol India. 2016. 64: 1220-32
16. Takami T, Ichinose T, Ishibashi K, Goto T, Tsuyuguchi N, Ohata K. Importance of fixation angle in posterior instrumented occipitocervical fusion. Neurol Med Chir (Tokyo). 2008. 48: 279-82