- Department of Neurological Surgery, The Aga Khan University Hospital, Karachi, Sindh, Pakistan.
- Department of Pathology, The Aga Khan University Hospital, Karachi, Sindh, Pakistan.
Correspondence Address:
Syed Ather Enam, Department of Neurological Surgery, The Aga Khan University Hospital, Karachi, Sindh, Pakistan.
DOI:10.25259/SNI_684_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammad Hamza Bajwa1, Mohammad Yousuf Ul Islam1, Syed Sarmad Bukhari1, Ahsan Ali Khan1, Zubair Ahmad2, Syed Ather Enam1. Contralateral metastatic cerebellopontine angle glioblastoma: A rare manifestation. 30-Nov-2021;12:586
How to cite this URL: Mohammad Hamza Bajwa1, Mohammad Yousuf Ul Islam1, Syed Sarmad Bukhari1, Ahsan Ali Khan1, Zubair Ahmad2, Syed Ather Enam1. Contralateral metastatic cerebellopontine angle glioblastoma: A rare manifestation. 30-Nov-2021;12:586. Available from: https://surgicalneurologyint.com/surgicalint-articles/11255/
Abstract
Background: Glioblastoma is the most common glioma presenting within adults with an incidence of 10 per 100,000 people globally. These are mostly supratentorial tumors with rare cases of extra-axial spread. Even rarer is the presentation of glioblastoma within the cerebellopontine angle (CPA). Here, we present a case of a previously resected and irradiated glioblastoma metastasizing from the right temporal lobe region to the contralateral CPA.
Case Description: A 24-year-old female who previously underwent surgery and concurrent chemoradiotherapy for a right temporal glioblastoma in August 2020, presented to us 6 months later with headaches, vomiting, and dizziness for the past 6 days. She had left-sided dysmetria on examination. MRI of the brain showed an extra-axial, heterogeneously enhancing lesion within the left CPA. The patient subsequently underwent a left retrosigmoid craniotomy and maximum safe resection of the lesion. Histopathology reported the lesion as a glioblastoma.
Conclusion: Glioblastoma within the CPA is rarely reported within the literature. To date, our case is the first instance of an extra-axial contralateral metastasis of glioblastoma.
Keywords: Cerebellopontine angle, Extra axial, Glioblastoma, Infratentorial, Metastasis
INTRODUCTION
Glioblastomas are WHO grade IV neoplasms that account for 15–20% of all intracranial tumors and approximately 50 percent of all adult gliomas.[
Previous reviews have found only ten cases of primary glioblastoma extending into the CPA that were reported.[
CASE PRESENTATION
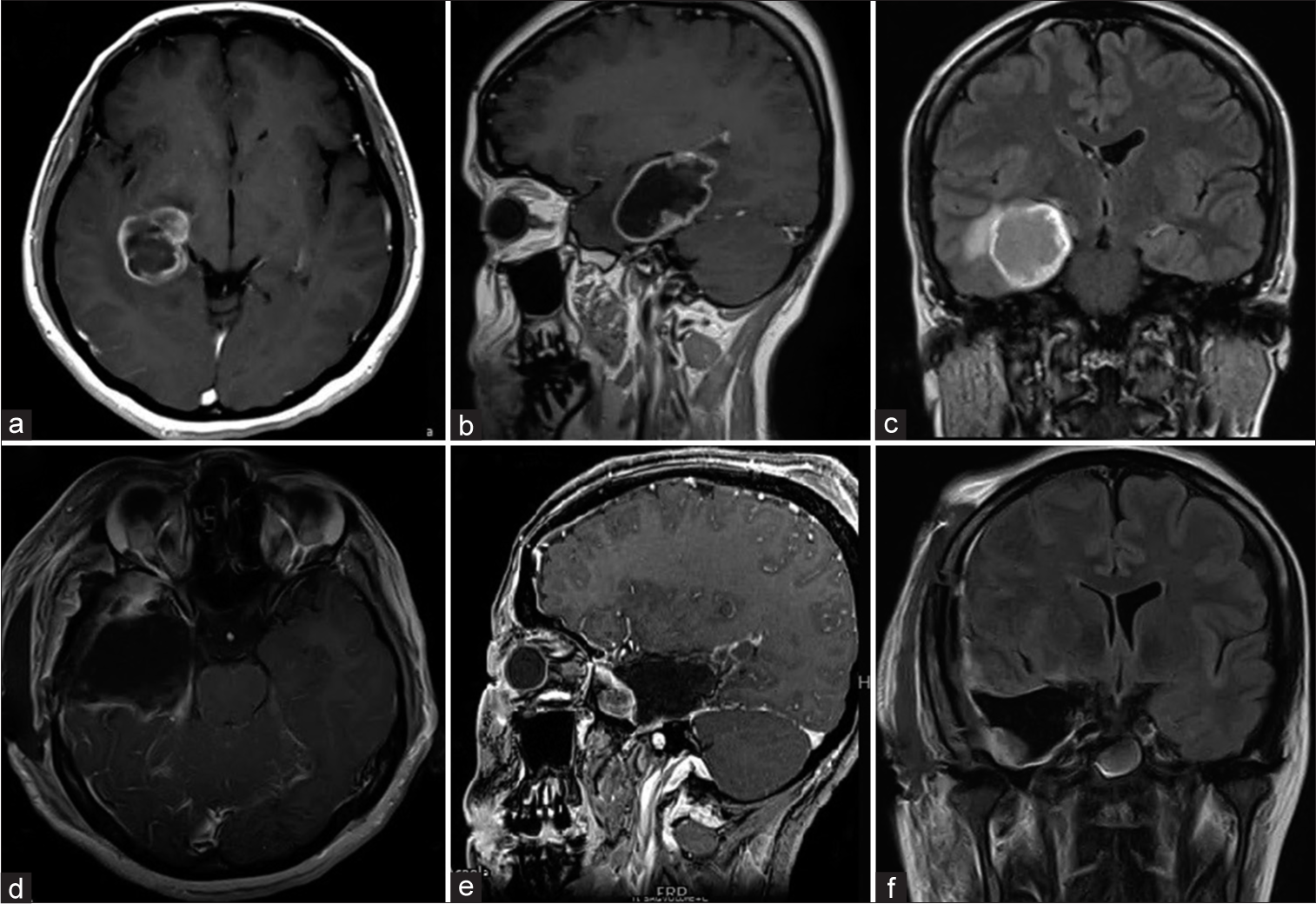
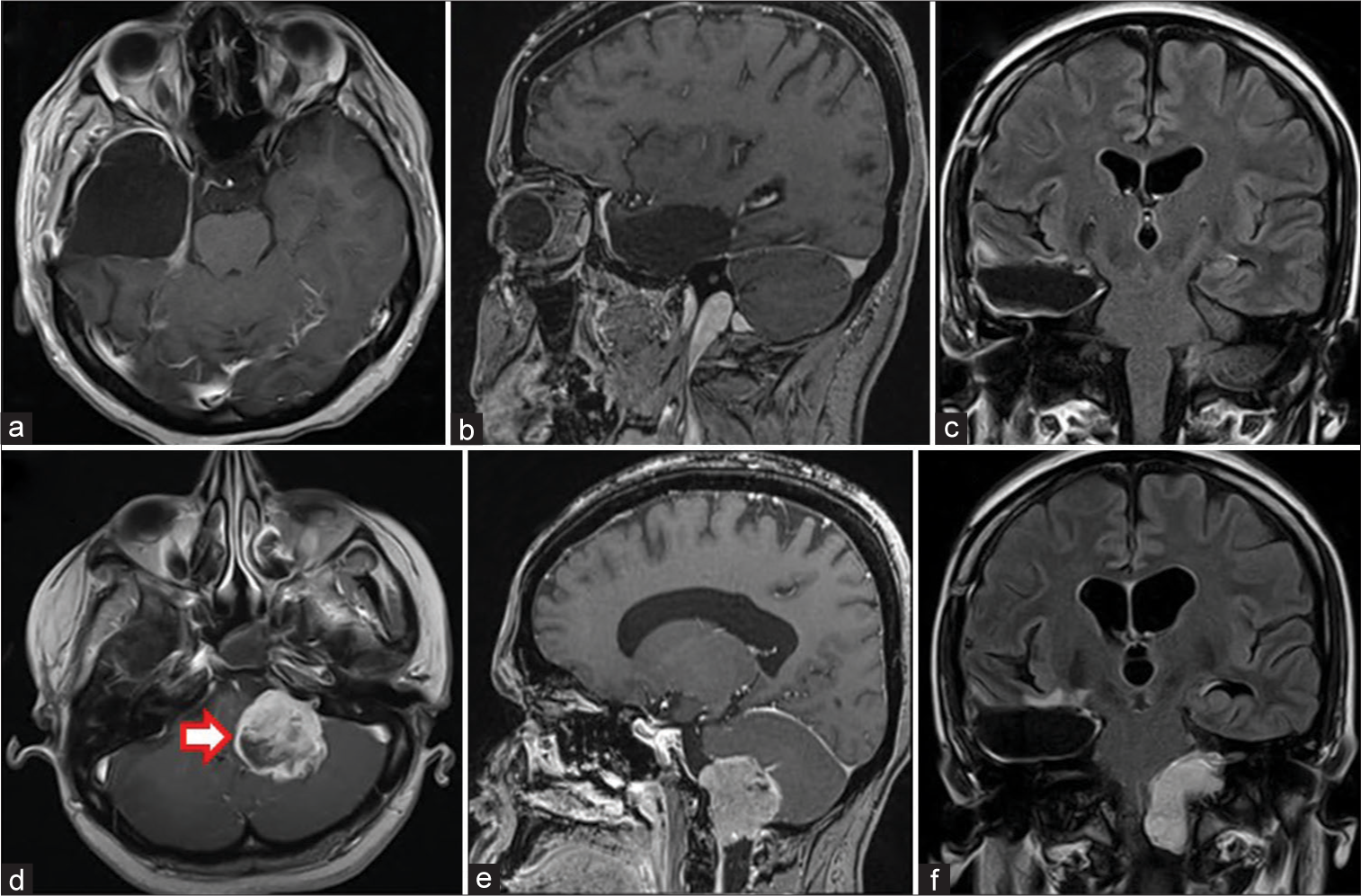
A 24-year-old right-handed female initially presented to our center in August 2020 with seizures for the past 1 week. Her MRI brain scan showed a right temporal heterogeneous lesion with a peripheral rim of contrast enhancement. Due to her symptoms and the suspicion this lesion was neoplastic, she underwent a right temporal lobectomy and gross total resection of the lesion [
Figure 1:
(a and b) Preoperative axial and sagittal T1 post contrast showing ring enhancing necrotic lesion in the right posterior temporal lobe. (c) Coronal FLAIR post-contrast showing central necrotic material. (d and e) T1 post-contrast axial and sagittal images showing gross total resection. (f) Coronal FLAIR post contrast image.
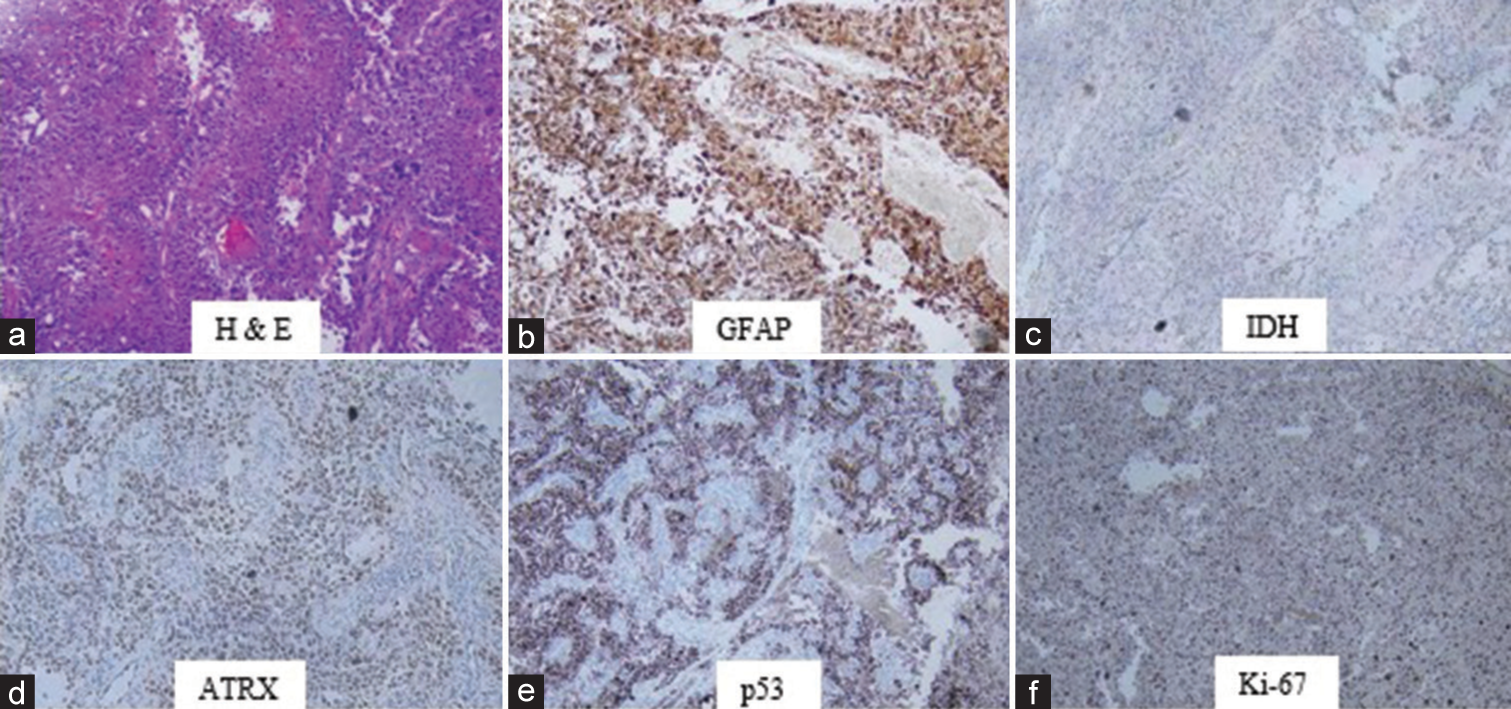
Figure 3:
(a-c) Postoperative MRI Brain at 6 months post-surgery showing no evidence of disease recurrence. The patient had received CCRT prior. (d-f) MRI Brain with contrast after symptom development. (d and e) T1 post-contrast axial and sagittal images demonstrating an extra-axial CPA lesion (red arrow) with extension into the internal acoustic meatus. (f) FLAIR coronal post contrast imaging demonstrating extent to the foramen magnum.
The patient presented to our emergency department in March 2021 with complaints of vomiting, headaches, and dizziness for the past 6 days. Her vomiting was non-projectile, two episodes per day, and associated with frontal headache. She also had complaints of imbalance and could not walk without support. She did not have any other associated history. Current medications included two anti-epileptic medications and temozolomide, 300 mg for 5 days every month, as prescribed by her primary oncologist. On examination, she was awake, alert, and oriented. Her pupils were bilaterally equal and reactive to light, and vision and speech were normal. She was found to be neurologically intact except for a mild left-sided lower motor neuron-type facial weakness. Her motor examination was normal. She had mild left-sided dysmetria and her gait could not be assessed due to severe dizziness. Her systemic examination was otherwise unremarkable. Preliminary lab investigations yielded no abnormalities.
MRI of the brain with contrast in this admission showed an extra-axial, abnormal signal intensity lesion in the left CPA [
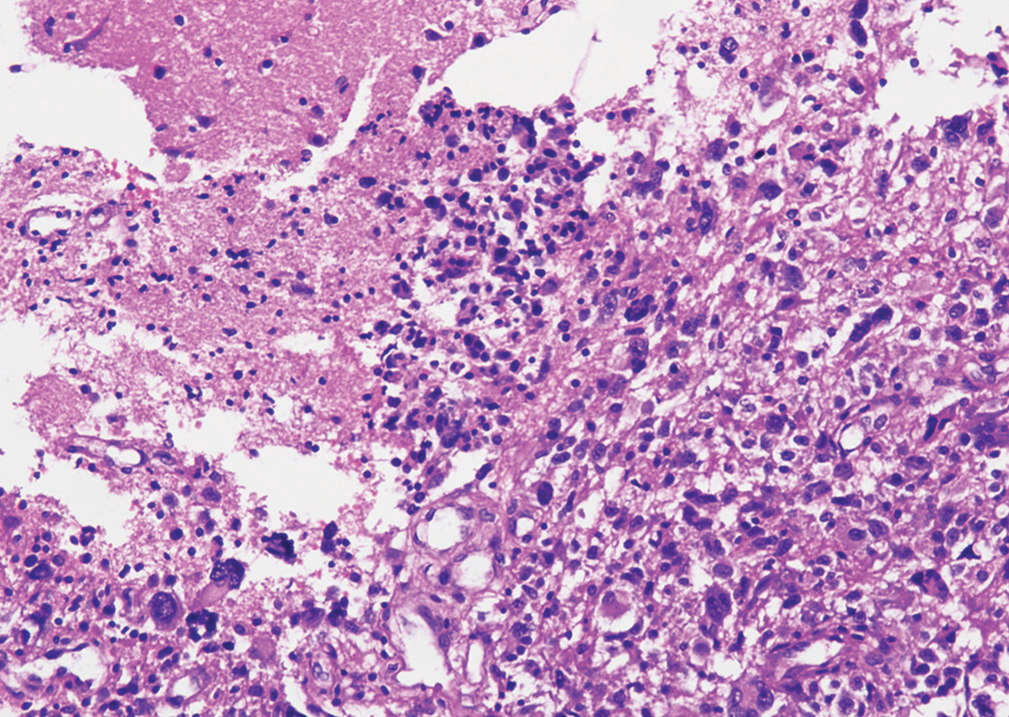
She underwent a left retrosigmoid craniotomy and resection of the lesion. Intraoperative findings showed a necrotic, soft, vascular lesion with matted lower cranial nerves passing through the bulk of the tumor. Maximum safe resection was done. Postoperative MRI with contrast showed near-total excision with a small residual. The patient was discharged from the hospital after 6 days, with mild cranial nerve deficits that were gradually improving. Final histopathology report showed a high-grade glial neoplasm with features favoring glioblastoma (WHO Grade IV) [
It was later decided by our radiation oncologists that radiation at this site near the brainstem carried significant risks and radiosurgery was advised along with intrathecal chemotherapy with a vascular endothelial growth factor inhibitor (Avastin).
DISCUSSION
Our case is a unique presentation of glioblastoma due to two reasons: glioblastoma in the CPA is a clinical rarity with few reported cases. Second, the presentation of glioblastoma metastasis is also uncommon within the literature, making the discussion of such a case necessary.
Ten cases of primary glioblastoma presenting in CPA have been previously published.[
The other unique feature of our report is metastasis occurring to the contralateral CPA, with no local recurrence at the primary lesion site. Recurrence of glioblastoma is almost always locally with rare distant intracranial metastasis. Gliomas metastasize through the CSF channels, yet highly malignant glioblastoma metastases are rarely seen. This is likely due to the early demise of patients from the primary disease before metastatic disease has manifested. Leptomeningeal metastasis has been seen in less than 2 percent of patients with glioblastoma, however, microscopic metastases have been detected in 6 percent of supratentorial lesions.[
Previous studies have looked at risk factors for metastasis of CNS tumors to the CPA, which increase the risk of dissemination from the CSF causing leptomeningeal involvement, and therefore further spread of disease.[
Intracranial metastasis of glioblastoma is rarely reported within the literature. The spread of cancer cells via the cerebrospinal fluid can potentially then create new foci of glioblastoma at a distant location, as seen in previous case reports.[
The management of metastatic glioblastoma includes repeat surgery, radiation (conventional and SRS), systemic chemotherapy, or combination therapies of the aforementioned. Particularly, radiosurgery has become an increasingly used salvage treatment modality for glioblastoma. This allows reduced treatment-related toxicity associated with other radiation oncology therapies and may provide benefit for cases of previously irradiated glioblastoma.[
CONCLUSION
Glioblastoma within the CPA is rare within the literature. Our case shows the possibility for extra-axial and contralateral metastasis from a previously irradiated glioblastoma, which has not been reported before.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
None.
References
1. Abdallah A, Uysal ML, Güler Abdallah B, Emel E. Intracranial metastasis of glioblastoma multiforme: A case report. J Nerv Syst Surg. 2015. 5: 97-100
2. Combs SE, Debus J, Schulz-Ertner D. Radiotherapeutic alternatives for previously irradiated recurrent gliomas. BMC Cancer. 2007. 7: 1-11
3. Hanif F, Muzaffar K, Perveen K, Malhi SM, Simjee SU. Glioblastoma multiforme: A review of its epidemiology and pathogenesis through clinical presentation and treatment. Asian Pac J Cancer Prev. 2017. 18: 3
4. Kalokhe G, Grimm SA, Chandler JP, Helenowski I, Rademaker A, Raizer JJ. Metastatic glioblastoma: Case presentations and a review of the literature. J Neurooncol. 2012. 107: 21-7
5. Kesari S, Batchelor TT. Leptomeningeal metastases. Neurol Clin. 2003. 21: 25-66
6. Lalwani AK. Meningiomas, epidermoids, and other nonacoustic tumors of the cerebellopontine angle. Otolaryngol Clin North Am. 1992. 25: 707-28
7. Lee JH, Kim JH, Kwon TH. Primary glioblastoma of the cerebellopontine angle: Case report and review of the literature. J Korean Neurosurg Soc. 2017. 60: 380
8. Mariniello G, Peca C, de Caro M, Corvino S, Orlando V. Cerebello-pontine angle glioblastoma with cervical spine metastasis: A case report. Neurosurg Cases Rev. 2019. 2: 12
9. Swaroop G, Whittle I. Exophytic pontine glioblastoma mimicking acoustic neuroma. J Neurosurg Sci. 1997. 41: 409-11
10. Yang DX, Jing Y, Xu ZM, Yuan F, Liu YL, Wang GS. Primary glioblastoma of cerebellopontine angle in adult mimicking acoustic neuroma. World Neurosurg. 2019. 122: 48-52
11. Zhang M, Wang Z, Zhang J, Zhang H, Gu C, Wang H. Metastases in cerebellopontine angle from the tumors of central nerve system. J Clin Neurosci. 2017. 42: 84-90