- Department of Neurosurgery, Mohammed V Military Teaching Hospital of Rabat, Rabat, Morocco
- Department of Neurosurgery, Faculté de Médecine, Université Catholique de Bukavu, Democratic Republic of Congo, Université Catholique de Bukavu, South-Kivu, Democratic Republic of the Congo
- Department of Research, Sub-Saharan Africa Future Neurosurgeon Association, Cotonou, Benin
- Department of Neurosurgery, Faculty of Medicine and Pharmacy of Mohammed V University of Rabat, Rabat, Morocco
Correspondence Address:
Yao Christian Hugues Dokponou, Mohammed V Military Teaching Hospital of Rabat, Rabat,
DOI:10.25259/SNI_68_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yao Christian Hugues Dokponou1, Arsene Daniel Nyalundja2, Arsene Desire Ossaga Madjoue3, Mèhomè Wilfried Dossou3, Omar Badirou3, Nicaise Agada3, Katib Lasssissi3, Fritzell Marc adjovi3, Laté dzidoula Lawson3, Nourou Dine Adeniran Bankole4. COVID-19 impact on the global neurosurgery resident training course and admission: A scoping review. 24-Mar-2023;14:96
How to cite this URL: Yao Christian Hugues Dokponou1, Arsene Daniel Nyalundja2, Arsene Desire Ossaga Madjoue3, Mèhomè Wilfried Dossou3, Omar Badirou3, Nicaise Agada3, Katib Lasssissi3, Fritzell Marc adjovi3, Laté dzidoula Lawson3, Nourou Dine Adeniran Bankole4. COVID-19 impact on the global neurosurgery resident training course and admission: A scoping review. 24-Mar-2023;14:96. Available from: https://surgicalneurologyint.com/surgicalint-articles/12217/
Abstract
Background: This study looks at how COVID-19 affected the admission and training of neurosurgical residents worldwide.
Methods: From 2019 to 2021, we reviewed multiple databases (i.e., Google Scholar, Science Direct, PubMed, and Hinari) to evaluate the impact of the COVID-19 pandemic on neurosurgery resident training and admission in low middle-income countries (LMICs) and high-income countries (HICs). We then utilized a Wilcoxon signed-rank test to evaluate the difference between the two LMIC/HICs and employed Levene’s test to assess the homogeneity of variances.
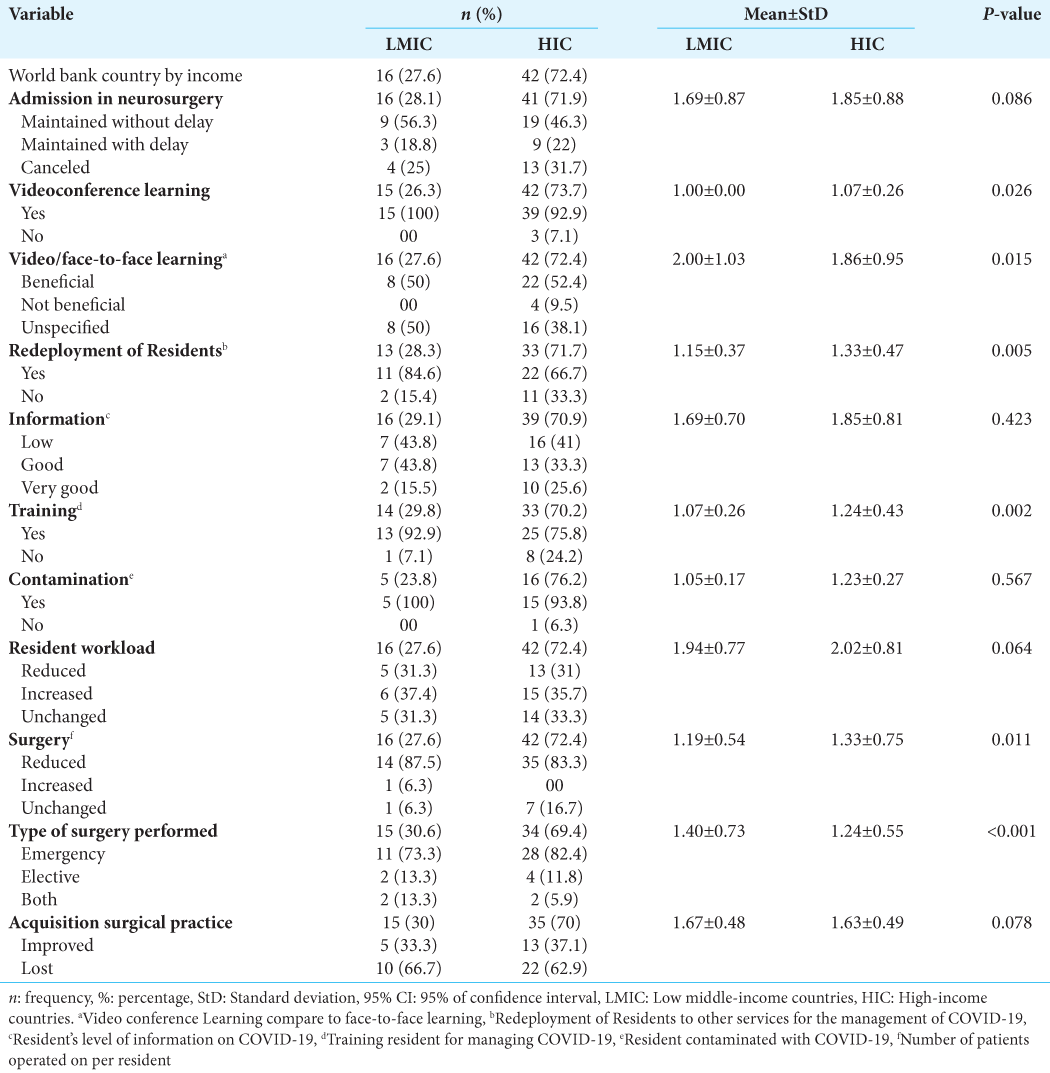
Results: There were 58 studies that met our inclusion criteria; 48 (72.4%) were conducted in HIC and 16 (27.6%) in LMIC. The admission of new residents was mostly canceled in HIC (31.7%; n = 13) and in LMIC (25%; n = 4) from 2019 to 2021 due to COVID-19. Learning modalities changed to include predominantly video conferencing (i.e., 94.7% [n = 54] of cases). Further, neurosurgery was largely restricted to emergency cases alone (79.6% [n = 39]), with only 12.2% (n = 6) elective cases. The result was a marked reduction in resident surgical training (i.e., 66.7% [n = 10] in LMIC and 62.9% [n = 22] in HIC), despite increased workloads in (i.e., LMIC [37.4%; n = 6] and HIC [35.7%; n = 15]). This was attributed to the marked reduction in the number of surgical patients allotted to each resident (i.e., LMIC [87.5%; n = 14] than HIC [83.3%; n = 35]).
Conclusion: The COVID-19 pandemic markedly disrupted neurosurgical education globally. Although differences have been found between LMICs and HICs training, the reduction of neurosurgical case-loads and surgical procedures has significantly impacted neurosurgical training. The question remains, how can this “loss of experience” be redressed in the future?
Keywords: High-income countries (HICs), Impact of COVID-19, Low middle-income countries (LMICs), Neurosurgery, Residency training
INTRODUCTION
Many studies have focused on COVID-19-related delays and even global cancellations of neurosurgery residency training programs in low middle-income countries (LMICs) and high-income countries (HICs). Even with fewer working hours, neurosurgery residents showed a 26.1% burnout, and reduced 73.9% career satisfaction rate.[
Further, there have been significant reductions in conventional training opportunities (i.e., cancellation of educational/multidisciplinary subspecialty meetings, and outpatient clinics) in LMIC versus HIC.
METHODS IN INCLUDING PATIENT SELECTION
We reviewed how the COVID-19 pandemic impacted the admission and training of neurosurgical residents worldwide, that is, including assessment from the EQUATOR Network.[
Data analysis
Data analysis was conducted with JAMOVI 2.3.18 for statistical analysis of univariable (i.e., frequencies and percentages for qualitative variables, 95% confidence intervals [95% CI] for quantitative variables) and bivariable (i.e., odds ratios and their 95% CI, Chi-square test, and ANOVA), and multinomial regression analyses. Interregional and intraregional comparisons were made using bivariate correlations for the World Bank Country by Income (LMICs and HICs). A Wilcoxon signed-rank test was used to evaluate whether there was a significant difference between them (i.e., P < 0.05). Levene’s test (Independent samples t-test) was used to evaluate the assumption of homogeneity of variances (i.e., low P-value indicated violation of the assumption of equal variances).
RESULTS
58 Articles from four continents
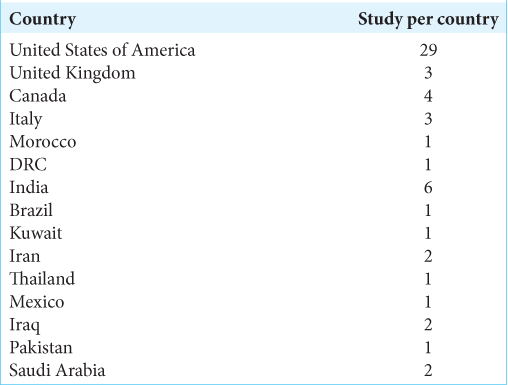
We ultimately used 58 articles for data extraction (i.e., just 4.75 % of those originally identified, published between January 2020 and August 2021). Half were from the USA (n = 29, 50%), fifteen (25.86%) from Asian countries, six (10.34%) from Europe, and two from Africa (3.44%) [
Data for HIC versus LMIC neurosurgical residency admissions and training
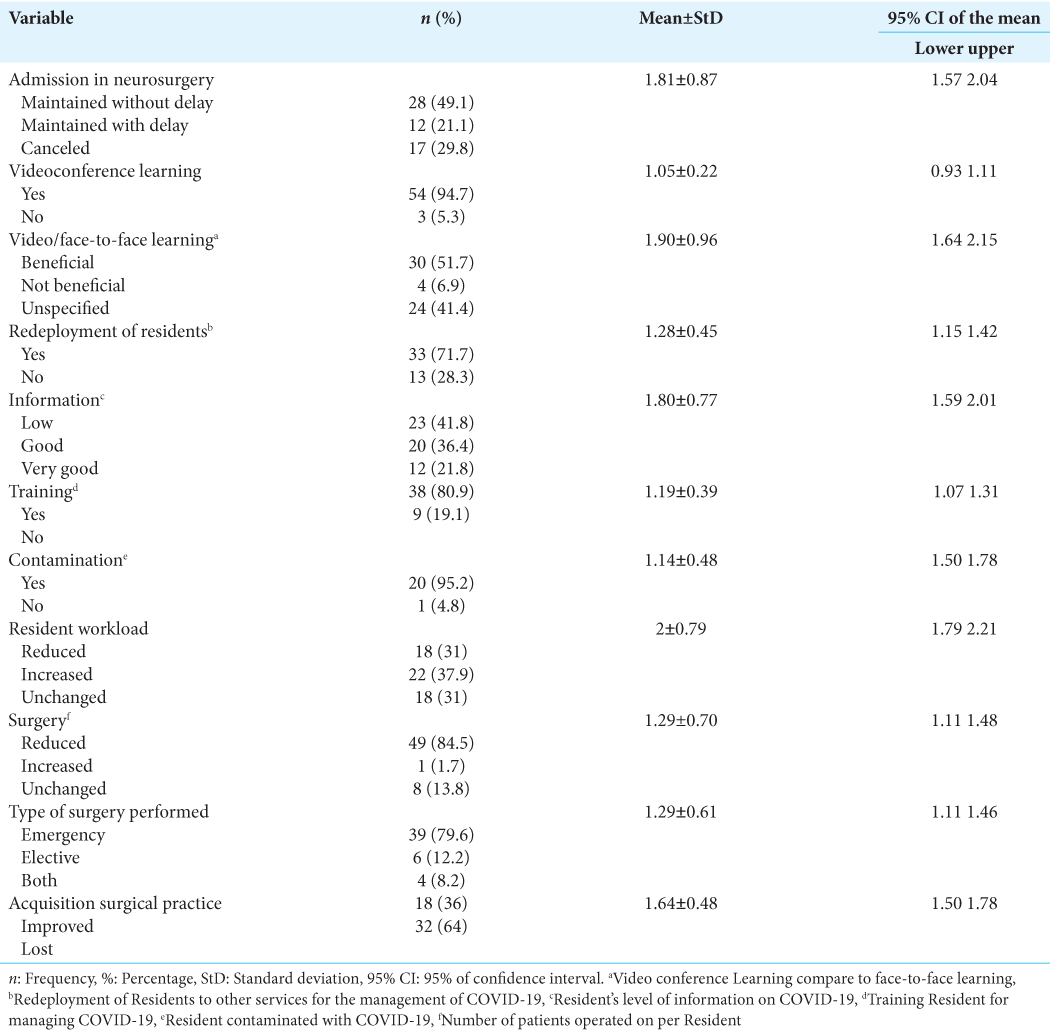
Seventy-two-point four percentages (n = 42) of the included studies were conducted in HIC and 27.6% (n = 16) in LMIC. The admission for neurosurgery residency was canceled in 13 centers of HIC (31.7%) versus four centers (25%) in LMIC. The COVID-19 impact worldwide; admission rates for neurosurgery residents were maintained at 49.1% (n = 28; without delays), but was canceled in 29.8% (n = 17) of cases. Learning was converted 94.7% (n = 54) of the time to videoconference with 51.7% (n = 30) of satisfaction (i.e., benefice vs. face-to-face learning). Notably, 71.7% (n = 33) reported neurosurgery residents’ redeployment to other departments for the management of COVID-19 patients, with a workload increased by 37.9% (n = 22) [
DISCUSSION
Reductions in neurosurgical admissions, training, and surgical experience
We identified that from the 58 studies on the impact COVID-19 had on neurosurgery resident training and admission was maintained in the vast majority of cases 70.2% [n = 40]) around the world. Fourty two of the studies were from HIC (72.4%) and 16 (27.6%) were conducted in LMIC. Worldwide, the admissions for neurosurgery residencies were maintained without delay in almost half of the cases 49.1% (n = 28), while they were delayed in 21.1% (n = 12), and canceled only in 29.8% (n = 17) of cases. Nonetheless COVID-19 reduced technical neurosurgical experience by 64%, dealing mainly with emergency cases (79.6%) with very little elective surgery 12.2%. Moreover, the number of patients operated on per resident was reportedly reduced by 84.5%.
Implications
Saad et al.[
Redistribution of hospital resources
This redistribution of hospital resources to combat COVID-19 depleted the neurosurgical staff due to interim deployment to other services/functions and training. Fortunately, many training centers utilizing virtual meetings to discuss weekly case rounds and allow for didactic presentations.
Keeping neurosurgery residents safe from COVID-19 by developing two teams: Inpatient versus remote
Neurosurgery residents and fellows during the pandemic were utilized as front-line providers in Academic Medical Centers. Nevertheless, to keep them “safe,” we found some institutions adopted a two-team approach: “active-duty inpatient” and “remotely working.” These two teams remained completely isolated from each other to decrease the exposure to the virus. They worked in 2-week cycles, allowing the team-work from active duty to self-isolate, while the others looked out for the onset of symptoms in the hospital setting (i.e., during the potential incubation periods). This two-team method appeared to reduce the chance of transmitting the infection to other team members or patients.[
COVID-19 harm to neurosurgery training
COVID-19 harmed neurosurgical training; 64% reported the loss of resident experience, coupled with the reduction of exposure to surgery (84.5%), and exposure to mainly emergency (79.6%) versus elective cases.
CONCLUSION
Neurosurgery residents around the world have faced serious and ongoing challenges due to the COVID-19 pandemic. It disrupted the training, and specifically, hands-on surgical experience. Strategies to minimize the disruption of neurosurgical education in low and HICs should be developed to tackle future similar events.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Al-Ahmari AN, Ajlan AM, Bajunaid K, Alotaibi NM, Al-Habib H, Sabbagh AJ. Perception of neurosurgery residents and attendings on online webinars during COVID-19 pandemic and implications on future education. World Neurosurg. 2021. 146: e811-6
2. Aljuboori Z, Ding D, Williams B. The effects of COVID 19 pandemic on neurosurgical training in the United States. Neurosurgery. 2020. 67:
3. Aljuboori ZS, Young CC, Srinivasan VM, Kellogg RT, Quon JL, Alshareef MA. Early effects of COVID-19 pandemic on neurosurgical training in the United States: A case volume analysis of 8 programs. World Neurosurg. 2021. 145: e202-8
4. Dash C, Venkataram T, Goyal N, Chaturvedi J, Raheja A, Singla R. Neurosurgery training in India during the COVID-19 pandemic: Straight from the horse’s mouth. Neurosurg Focus. 2020. 49: E16
5. Khalafallah AM, Lam S, Gami A, Dornbos DL, Sivakumar W, Johnson JN. A national survey on the impact of the COVID-19 pandemic upon burnout and career satisfaction among neurosurgery residents. J Clin Neurosci. 2020a. 80: 137-42
6. Lee KS, Zhang JJ, editors. Letter to the editor: “Medical student concerns relating to neurosurgery education during COVID-19”. World Neurosurg. 2020. 140: 484-5
7. Miranda SP, Glauser G, Wathen C, Blue R, Dimentberg R, Welch WC, editors. Letter to the editor “incorporating telehealth to improve neurosurgical training during the COVID-19 pandemic”. World Neurosurg. 2020. 139: 728-31
8. Pennington Z, Lubelski D, Khalafallah AM, Ehresman J, Sciubba DM, Witham TF, editors. Letter to the editor “changes to neurosurgery resident education since onset of the COVID-19 Pandemic”. World Neurosurg. 2020. 139: 734-40
9. Ramos O, Mierke A, Eastin M, Morrison MJ, Wongworawat DM, Danisa O. COVID-19 pandemic and the implications for orthopaedic and neurosurgery residents and fellows on spine rotations. N Am Spine Soc J. 2020. 1: 100006
10. Saad H, Alawieh A, Oyesiku N, Barrow DL, Olson J. Sheltered neurosurgery during COVID-19: The emory experience. World Neurosurg. 2020. 144: e204-9
11. Scullen T, Mathkour M, Maulucci CM, Dumont AS, Bui CJ, Keen JR, editors. Letter to the editor impact of the COVID-19 pandemic on neurosurgical residency training in New Orleans. World Neurosurg. 2020. 139: 718-9
12. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews EQUATOR Network. n.d. Available from: https://www.equator-network.org/reporting-guidelines/prisma [Last accessed on 2022 Nov 14].
13. Tomlinson SB, Hendricks BK, Cohen-Gadol AA, editors. Editorial, Innovations in neurosurgical education during the COVID-19 pandemic: Is it time to reexamine our neurosurgical training models?. J Neurosurg. 2020. 133: 14-5