- Department of Neurosurgery, Japanese Red Cross Medical Center, Tokyo, Japan.
Correspondence Address:
Toshikazu Kimura, Department of Neurosurgery, Japanese Red Cross Medical Center, Tokyo, Japan.
DOI:10.25259/SNI_430_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Akihiko Teshigawara, Toshikazu Kimura, Shunsuke Ichi. Critical cerebellar hemorrhage due to pilocytic astrocytoma in a child: A case report. 06-Sep-2021;12:448
How to cite this URL: Akihiko Teshigawara, Toshikazu Kimura, Shunsuke Ichi. Critical cerebellar hemorrhage due to pilocytic astrocytoma in a child: A case report. 06-Sep-2021;12:448. Available from: https://surgicalneurologyint.com/surgicalint-articles/11093/
Abstract
Background: Cerebellar hemorrhage is rare in children, and its cause is usually vascular disorders such as arteriovenous malformations or hematological disorders.
Case Description: A previously healthy 10-year-old girl presented with a loss of consciousness following sudden headache and vomiting. A non-contrast brain computed tomography (CT) scan revealed a massive cerebellar hemorrhage with obstructive hydrocephalus; however, subsequent CT angiography (CTA) showed no vascular abnormalities. An emergency craniotomy was performed to evacuate the hematoma, and histological analysis of the specimen obtained from the tissue surrounding the hematoma revealed a pilocytic astrocytoma (PA). Six months after the ictus, her recovery was scored at 2 on the modified Rankin Scale.
Conclusion: PA can be a cause of critical cerebellar hemorrhage. In this case of life-threatening massive hematoma, CTA was useful to exclude a major vascular pathology and to save time.
Keywords: Cerebellar hemorrhage, Computed tomography angiography, Intratumoral hemorrhage, Pediatric stroke, Pilocytic astrocytoma
INTRODUCTION
Hemorrhagic stroke in the cerebellum is rare in children, and the main causes are vascular lesions such as arteriovenous malformations (AVMs) and coagulopathy/thrombocytopenia related to hematological disorders.[
CASE PRESENTATION
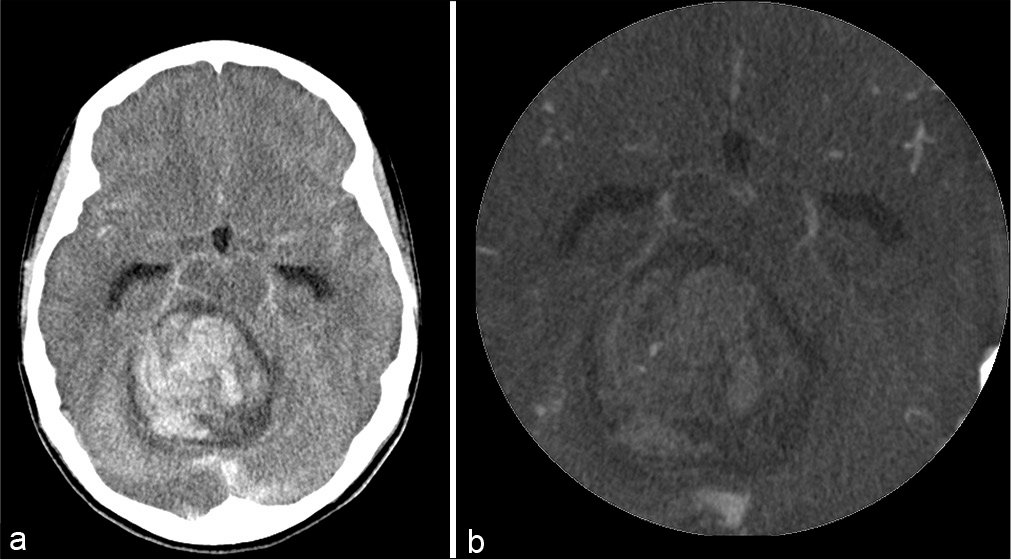
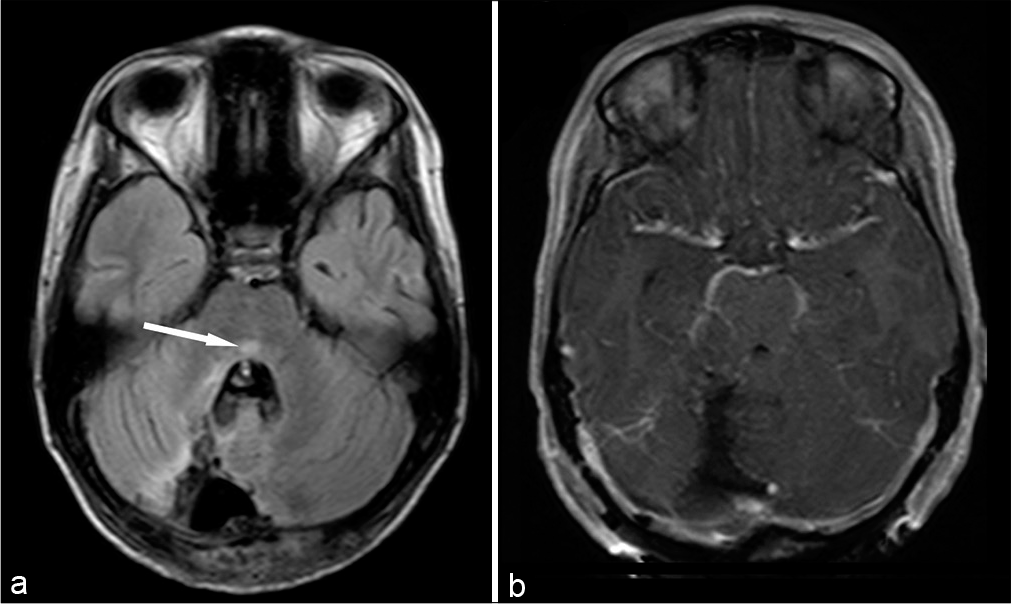
A previously healthy 10-year-old girl presented with a sudden loss of consciousness following sudden headache and vomiting. There were no antecedent symptoms, such as headache or ataxic gait, according to the parents. On admission, she was comatose, with a Glasgow coma scale (GCS) score of 6 and a blood pressure of 113/84 mmHg. Her pupils were isocoric, and the light reflex was maintained. She was intubated for respiratory assistance and sedated. Brain computed tomography (CT) revealed a cerebellar hemorrhage 5 cm in size with slight obstructive hydrocephalus [
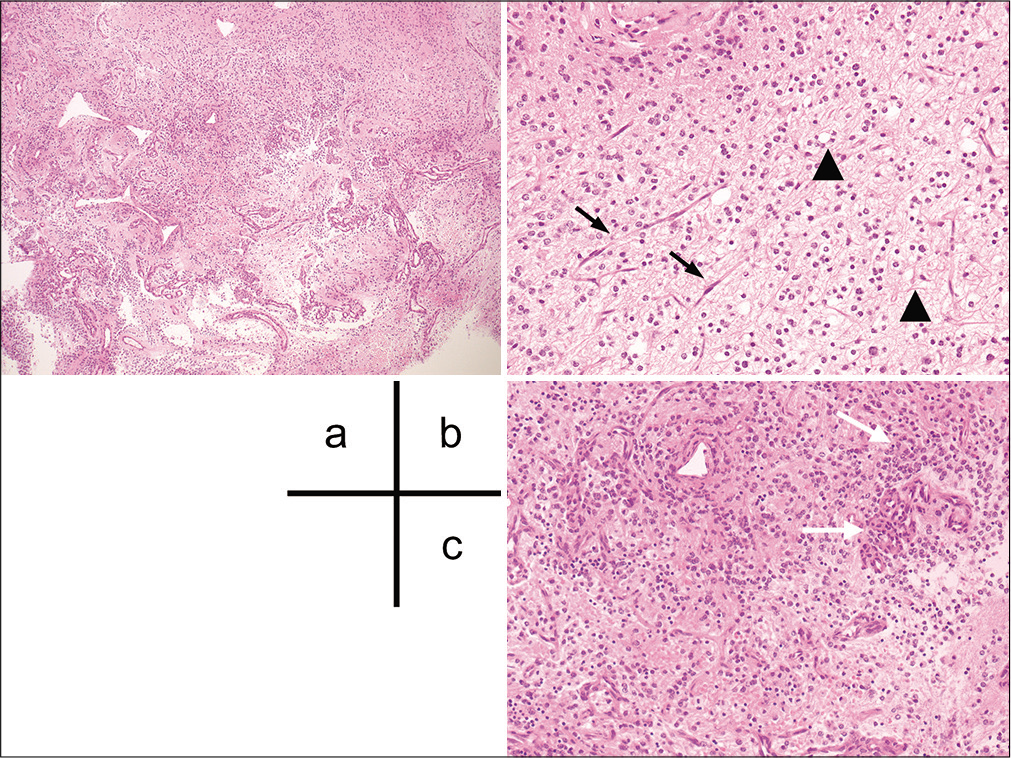
Figure 2:
Histopathological examination of the specimen. (a) Hematoxylin-eosin (HE) staining shows a biphasic pattern with varying proportions of piloid areas alternating with spongy areas with high vascularity. (b) Bipolar neoplastic cells with elongated hair-like processes (black arrow) and oligodendroglioma-like cells with cytoplasmic vacuoles (arrowhead). (c) Glomeruloid-like vascular proliferation (white arrows) is visible.
DISCUSSION
A rare case of massive cerebellar hemorrhage in a child due to PA was presented. CTA was useful to exclude a major vascular disorder and to save time in the treatment of this critical condition.
Hemorrhagic stroke accounts for approximately one-half of all cases of pediatric stroke, with an annual incidence of 1.2–13 cases/100,000;[
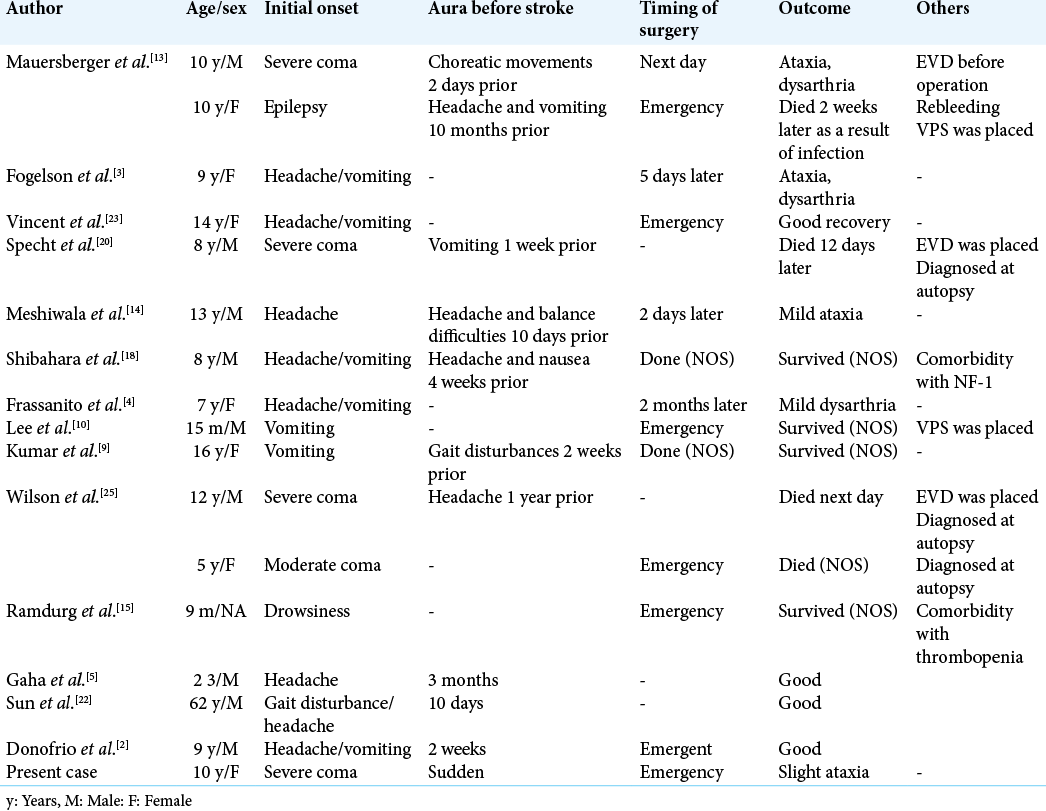
According to a previous report, initial GCS is the prognostic factor of cerebellar hemorrhage from PA.[
In the operation, there was marked hemorrhage, presumably due to the fragile microvasculature of the tumor, while we could distinguish soft, yellowish tissue during evacuation of the hematoma, which could have been removed easily with suction. Although CTA showed no vascular anomaly, we suspected that there was a vascular origin of the hemorrhage, such as a small AVM or hemorrhagic tumor. Close inspection and biopsy are important not only after hemostasis but also during hematoma evacuation for definitive diagnosis. It is not usually easy to distinguish small pathology while controlling the hemorrhage and finding the origin, but meticulous control of the suction pressure is important to identify the etiology of a hemorrhage that is difficult to explain. On the other hand, as the purpose of an emergent surgery is to save the patient’s life and to minimize neurological deficits. As past reports have shown [
CONCLUSION
A case of a patient with pediatric PA presenting with massive cerebellar hemorrhage was presented. CTA was useful to exclude the diagnosis of major vascular disorder and to save time, and close inspection and biopsy of the hematoma cavity were important for establishing a definitive diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We appreciate Dr. Toshihide Tanaka, Department of Neurosurgery, Jikei University School of Medicine, Kashiwa Hospital, for helpful advice regarding manuscript editing.
References
1. Araki T, Akaike Y, Sakamoto M, Maeda K, Takagi M, Tabuchi K. Spontaneous cerebellar hemorrhages in children: Report of 2 cases. Jpn J Neurosurg. 2000. 9: 375-80
2. Donofrio CA, Gagliardi F, Callea M, da Passano CF, Terreni MR, Cavalli A. Pediatric cerebellar pilocytic astrocytoma presenting with spontaneous intratumoral hemorrhage. Neurosurg Rev. 2018. 22: 18-969
3. Fogelson MH, Oppenheim RE, McLaurin RL. Childhood cerebellar astrocytoma presenting with hemorrhage. Neurology. 1980. 30: 669-70
4. Frassanito P, Massimi L, Caldarelli M, Di Rocco C. Cerebellar mutism after spontaneous intratumoral bleeding involving the upper cerebellar vermis: A contribution to the physiopathogenic interpretation. Childs Nerv Syst. 2009. 25: 7-11
5. Gaha M, Bouzayen F, Limam Y, Mokni M, Jemni-Gharbi H, Tlili-Graiess K. Pilocytic astrocytoma mimicking cavernous angioma: Imaging features and histological characteristics. Neurochirurgie. 2017. 63: 330-3
6. Johnson DR, Brown PD, Galanis E, Hammack JE. Pilocytic astrocytoma survival in adults: Analysis of the surveillance, epidemiology, and end results program of the national cancer institute. J Neurooncol. 2012. 108: 187-93
7. Kapoor A, Savardekar A, Tewari MK, Chatterjee D, Radotra BD. Spontaneous hemorrhages in pediatric supratentorial pilocytic astrocytomas. Malignant presentation of a benign entity. Childs Nerv Syst. 2015. 31: 1617-20
8. Kim MS, Kim SW, Chang CH, Kim OL. Cerebellar pilocytic astrocytomas with spontaneous intratumoral hemorrhage in adult. J Korean Neurosurg Soc. 2011. 49: 363-6
9. Kumar A, Deopujari CE, Biyani N, Mhatre MV. Pediatric cerebellar pilocytic astrocytoma presenting with hemorrhage. Neurol India. 2010. 58: 972-4
10. Lee CS, Huh JS, Sim KB, Kim YW. Cerebellar pilocytic astrocytoma presenting with intratumor bleeding, subarachnoid hemorrhage, and subdural hematoma. Childs Nerv Syst. 2009. 25: 125-8
11. Lo WD. Childhood hemorrhagic stroke: An important but understudied problem. J Child Neurol. 2011. 26: 1174-85
12. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007. 114: 97-109
13. Mauersberger W, Cuevas-Solorzano JA. Spontaneous intracerebellar hematoma during childhood caused by spongioblastoma of the IVth ventricle. Neuropadiatrie. 1977. 8: 443-50
14. Mesiwala AH, Avellino AM, Roberts TS, Ellenbogen RG. Spontaneous cerebellar hemorrhage due to a juvenile pilocytic astrocytoma: Case report and review of the literature. Pediatr Neurosurg. 2001. 34: 235-8
15. Ramdurg SR, Maitra J. A rare case of infantile cerebellar pilocytic astrocytoma and thrombocytopenia presenting with intratumoral hemorrhage. J Pediatr Neurosci. 2016. 11: 249-51
16. Rosen RS, Armbrustmacher V, Sampson BA. Spontaneous cerebellar hemorrhage in children. J Forensic Sci. 2003. 48: 177-9
17. Sgouros S, Fineron PW, Hockley AD. Cerebellar astrocytoma of childhood: Long-term follow-up. Childs Nerv Syst. 1995. 11: 89-96
18. Shibahara I, Kanamori M, Kumabe T, Endo H, Sonoda Y, Ogawa Y. Hemorrhagic onset of pilocytic astrocytoma and pilomyxoid astrocytoma. Brain Tumor Pathol. 2009. 26: 1-5
19. Shibao S, Kimura T, Sasaki H, Fujiwara H, Akiyama T, Ueno M. Hemorrhagic onset of cerebellar pilocytic astrocytoma in an adult: A case report and review of the literature implying a possible relation of degenerative vascular changes to the massive intratumoral hemorrhage. Brain Tumor Pathol. 2012. 29: 96-102
20. Specht CS, Pinto-Lord C, Smith TW, DeGirolami U, Suran E, Marshall PC. Spontaneous hemorrhage in a mixed glioma of the cerebellum: Case report. Neurosurgery. 1986. 19: 278-81
21. Srinivasan VM, Gressot LV, Daniels BS, Jones JY, Jea A, Lam S. Management of intracerebral hemorrhage in pediatric neurosurgery. Surg Neurol Int. 2016. 7: S1121-6
22. Sun S, Zhou H, Ding ZZ, Shi H. Cerebellar pilocytic astrocytomas with spontaneous intratumoral hemorrhage in the elderly: A case report and review of the literature. Medicine (Baltimore). 2018. 97: e11329
23. Vincent FM, Bartone JR, Jones MZ. Cerebellar astrocytoma presenting as a cerebellar hemorrhage in a child. Neurology. 1980. 30: 91-3
24. White JB, Piepgras DG, Scheithauer BW, Parisi JE. Rate of spontaneous hemorrhage in histologically proven cases of pilocytic astrocytoma. J Neurosurg. 2008. 108: 223-6
25. Wilson MP, Johnson ES, Hawkins C, Atkins K, Alshaya W, Pugh JA. Hemorrhagic presentations of cerebellar pilocytic astrocytomas in children resulting in death: Report of 2 cases. J Neurosurg Pediatr. 2016. 17: 446-52
26. Yoo H, Jung E, Gwak HS, Shin SH, Lee SH. Surgical outcomes of hemorrhagic metastatic brain tumors. Cancer Res Treat. 2011. 43: 102-7