- Department of Spine, Sancheti Institute of Orthopaedics and Rehabilitation, Pune, Maharashtra, India.
Correspondence Address:
Siddharth Manik Katkade, Department of Spine, Sancheti Institute of Orthopaedics and Rehabilitation, Pune, Maharashtra, India.
DOI:10.25259/SNI_437_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ajay Ramesh Kothari, Siddharth Manik Katkade, Pramod Dashrath Bhilare, Siddharth Aiyer, Nishad Vipul Situt, Shailesh Ramakant Hadgaonkar, Ashok Shyam, Parag Kantilal Sancheti. “Critical pedicle wall” breaches analysis in complex spinal deformity using O-arm navigation. 01-Sep-2023;14:306
How to cite this URL: Ajay Ramesh Kothari, Siddharth Manik Katkade, Pramod Dashrath Bhilare, Siddharth Aiyer, Nishad Vipul Situt, Shailesh Ramakant Hadgaonkar, Ashok Shyam, Parag Kantilal Sancheti. “Critical pedicle wall” breaches analysis in complex spinal deformity using O-arm navigation. 01-Sep-2023;14:306. Available from: https://surgicalneurologyint.com/surgicalint-articles/12525/
Abstract
Background: Free-hand and fluoroscopic-guided pedicle screw placement has been associated with higher rates of pedicle breaches (frequency range 15–40% especially in deformed pedicles). Neurological complications are more “critical” (i.e., frequent and significant) with medial and inferior pedicle-wall breaches due to the proximity of the neural elements. Here, we analyzed the effectiveness of O-arm navigation in minimizing “critical” pedicle wall breaches and their complications in 21 complex spinal deformity cases.
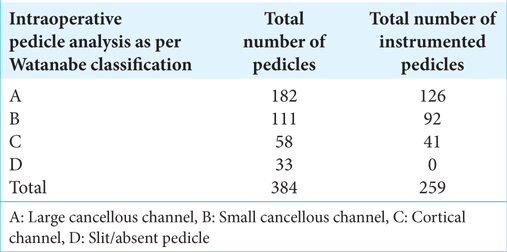
Methods: Twenty-one complex spinal deformity cases were prospectively managed with O-arm-navigated posterior-instrumented fusions. Preoperative assessment included; evaluation of the type of scoliosis, the magnitude of the deformity, and the anatomy of the pedicles – (i.e., classified using Watanabe et al.). The O-arm was used to confirm and grade both the intraoperative and postoperative location of screws. Other variables analyzed included; duration of surgery, estimated blood loss, complications, and radiation exposure.
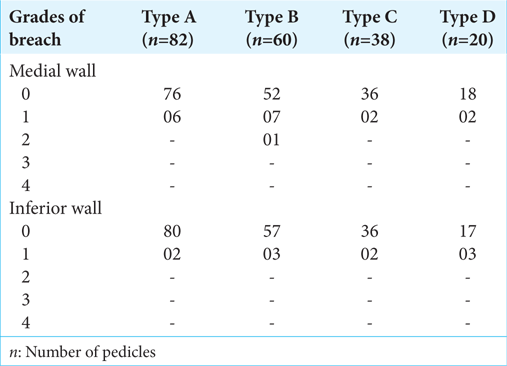
Results: In 21 patients, 259 (63.45%) of 384 pedicles were instrumented; we observed 22 of 259 pedicle screw breaches. Significant (>2 mm) breaches were observed in two medial and one inferior wall cases that required revision; the overall biomechanically significant screw breach rate was (3/259) 1.2% with an accuracy rate of 98.8%. Pedicle screw placement resulted in another 14 nonsignificant (
Conclusion: O-arm navigation decreased the incidence of medial and inferior (i.e., >2 mm “critical”) pedicle screw breaches applied in 21 patients with deformed pedicles due to scoliosis. Further, the O-arm minimized the operating time, decreased the estimated blood loss, and reduced the incidence of complications.
Keywords: Complex spinal deformity, Critical pedicle wall, Minimal complications, O-arm navigation, Pedicle breach
INTRODUCTION
Free-hand and fluoroscopic-guided pedicle screw placement has been associated with higher rates of pedicle breaches ranging from 15 to 40%, especially in patients with scoliosis and deformed pedicles. Neurological complications closely correlate critical medial and inferior wall breaches due to the proximity of the neural elements. Here, we evaluated whether O-arm navigation would increase the accuracy and safety of pedicle screw insertion in patients with complex scoliotic deformities.[
MATERIALS AND METHODS
In this Institutional Review Board-approved study, we evaluated 384 pedicles in 21 patients presenting with complex kyphoscoliosis (i.e., congenital scoliosis, neuromuscular scoliosis, syndromic scoliosis, and idiopathic scoliosis of Cobbs >60°) deformities (2021–2023). In this series, 259 pedicles were instrumented (63.45%) in 21 cases; seven had adolescent idiopathic scoliosis, five had congenital scoliosis, five had neuromuscular scoliosis, and four had syndromic scoliosis. The mean preoperative Cobb’s angle of major curve was 72.5° (Range: 65–103°).
Pedicle screw analysis
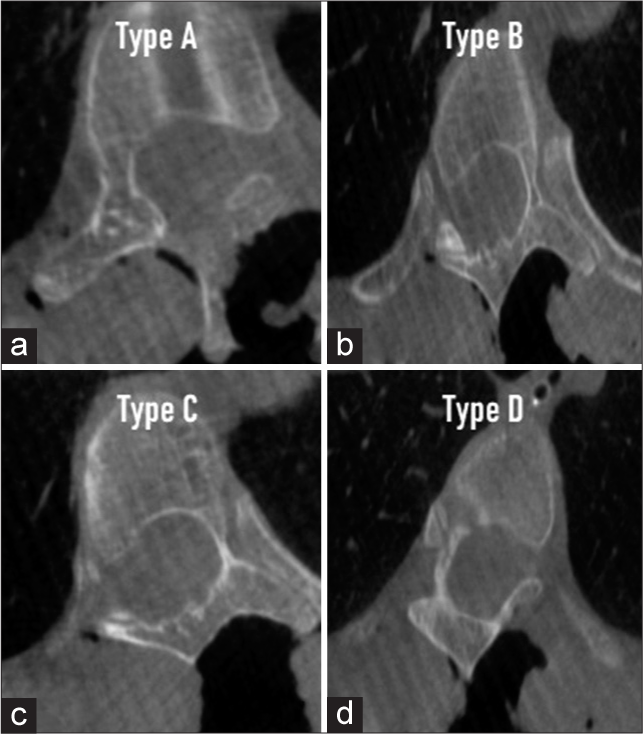
Intraoperatively after primary O-arm spin, computed tomography (CT) scan-based pedicle analysis was done and they were divided into type A–D (i.e., classified using Watanabe et al.)[
Devices
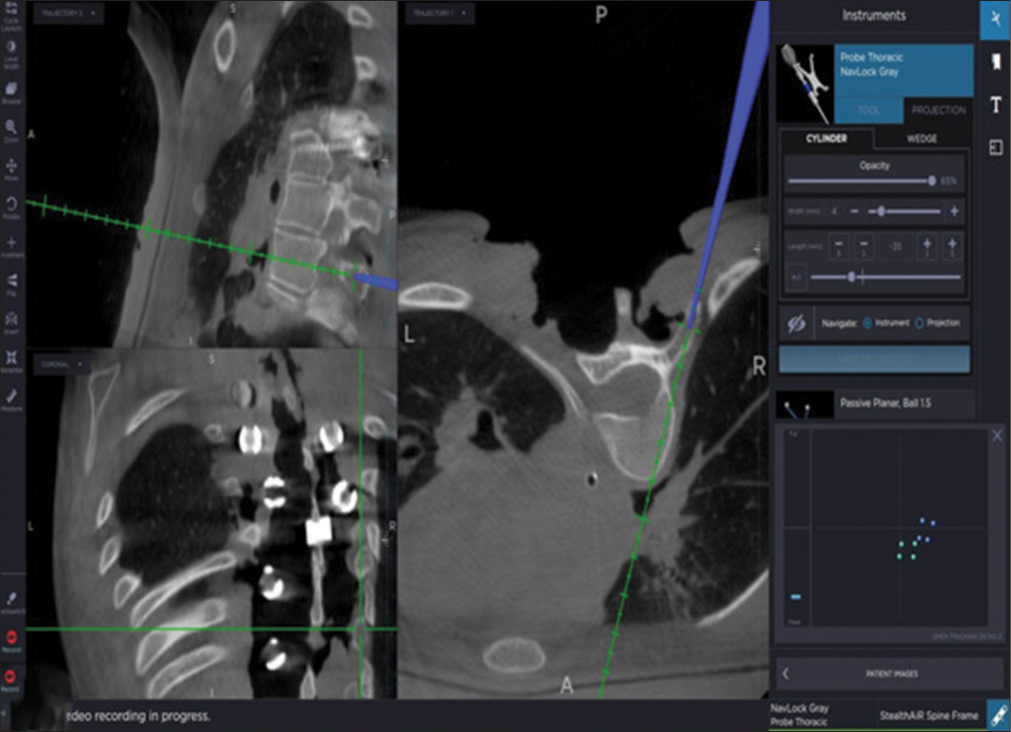
Third-generation intraoperative three-dimensional CT scan device, that is, O-arm, along with optical camera-based navigation, that is, S8 stealth station was used in this study for analysis and data storage. A dynamic reference array was attached to the spinous process based on levels of instrumentation [
Figure 2:
(a) Dynamic reference array frame attached in the middle of the surgical field for >6-level exposure, (b) demonstration of O-arm (at the foot end, not seen in the image) and stealth station (at the head end) setup in OR to ease triangulation between navigated instruments, dynamic reference array, and optical tracker.
Pedicle screw insertion
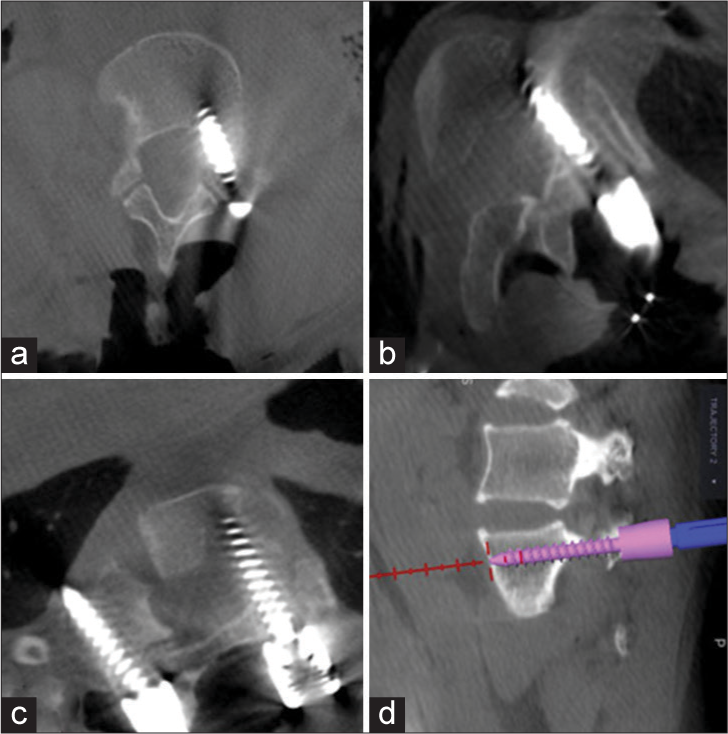
A standard posterior midline approach with standard techniques (i.e., intersection method) along with O-arm navigation aid was used to insert screws into the pedicles. The virtual dimensions (length and width) of the pedicles were displayed on O-arm navigation, and pedicular screws were inserted. In thinned, deformed, and sclerosed type C and D pedicles, where transpedicular screw fixation was not possible, an in-out-in technique [
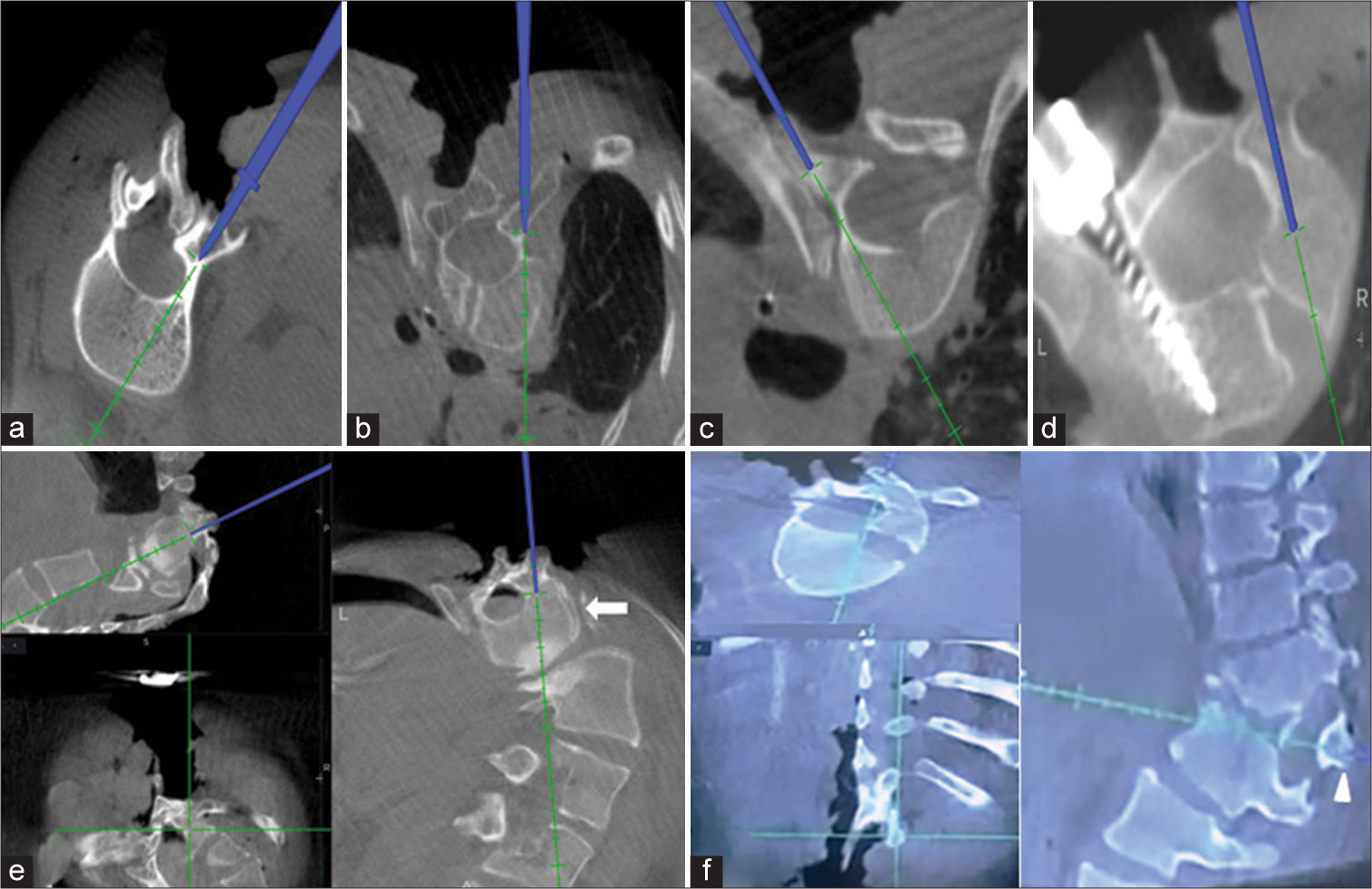
Figure 5:
Utility of O-arm navigation in intraoperative assessment of special situations which preoperative and other intraoperative modalities fail to address. (a-c) Intraoperative assessment of Watanabe et al. pedicle type B, C, and D pedicle, respectively, enabling safe placement or avoidance of pedicle screw, (d) limiting pedicle screw length in atypical vertebrae, that is, hemivertebrae, (e) demonstration of apical vertebrae in omega deformity which shows complete vertically oriented vertebrae(white arrow), and (f) identification of hemivertebrae and planning pedicle screw dimension avoid an anterior breach, assisting in planning hemivertebrae excision, predicting dimensions of hemivertebrae wedge resection (white arrowhead), and deformity correction.
RESULTS
Of the 259 instrumented pedicles, 38 pedicular screws were planned in-out-in trajectories screws (majority type C and D pedicles), and excluding in-out-in screws 22 pedicular screw breaches were noted. They occurred; medially in 12 cases, inferiorly in five cases, laterally in three cases, and anteriorly in two cases. There were ten medial and four inferior wall nonsignificant breaches versus significant breaches two medial and one inferior breach that needed revision [
DISCUSSION
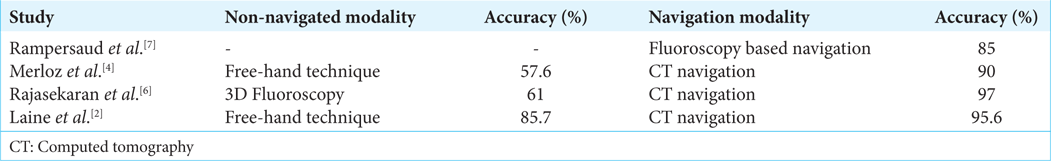
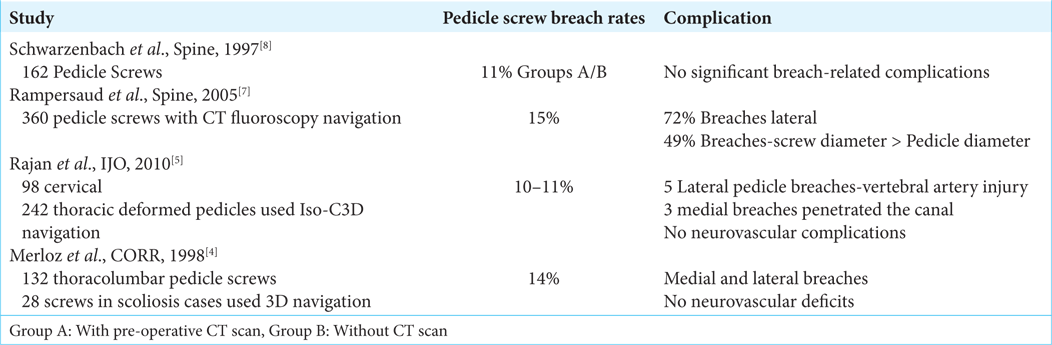
Several studies documented pedicle screw breach rates ranging from 10% to 15% using free-hand or fluoroscopic techniques [
Complications
Complications are typically seen with navigation-guided pedicular screw placement mainly in complex deformity/ dysplastic pedicle cases, for example, severe rigid idiopathic scoliosis, congenital scoliosis, neuromuscular scoliosis, and dystrophic scoliosis. If inferior and medial pedicular breaches (“critical”) are avoided, neurological complications will not occur. In select cases, we deliberately performed lateral wall breaches (i.e., an in-out-in technique in thoracic dysplastic pedicles), especially for type C and D pedicles [
CONCLUSION
Utilization of O-arm navigation with thorough knowledge of critical pedicle wall majorly in cases of complex spinal deformity helps in avoiding complications yielding favorable outcomes by decreasing surgical time, blood loss, patient radiation exposure, and early recovery. Further, the safety and efficacy are superior to the 10–15% incidence of pedicle screw breaches using free hand and other navigational techniques (i.e., 11–15%).[
Declaration of patient consent
The Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC. Accuracy of pedicle screw placement: A systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. 2012. 21: 247-55
2. Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D. Accuracy of pedicle screw insertion with and without computer assistance: A randomised controlled clinical study in 100 consecutive patients. Eur Spine J. 2000. 9: 235-40
3. Li G, Lv G, Passias P, Kozanek M, Metkar US, Liu Z. Complications associated with thoracic pedicle screws in spinal deformity. Eur Spine J. 2010. 19: 1576-84
4. Merloz P, Tonetti J, Pittet L, Coulomb M, Lavalleé S, Sautot P. Pedicle screw placement using image guided techniques. Clin Orthop Relat Res. 1998. 354: 39-48
5. Rajan VV, Kamath V, Shetty AP, Rajasekaran S. Iso-C3D navigation assisted pedicle screw placement in deformities of the cervical and thoracic spine. Indian J Orthop. 2010. 44: 163-8
6. Rajasekaran S, Bhushan M, Aiyer S, Kanna R, Shetty AP. Accuracy of pedicle screw insertion by AIRO® intraoperative CT in complex spinal deformity assessed by a new classification based on technical complexity of screw insertion. Eur Spine J. 2018. 27: 2339-47
7. Rampersaud YR, Pik JH, Salonen D, Farooq S. Clinical accuracy of fluoroscopic computer-assisted pedicle screw fixation: A CT analysis. Spine (Phila Pa 1976). 2005. 30: E183-90
8. Schwarzenbach O, Berlemann U, Jost B, Visarius H, Arm E, Langlotz F. Accuracy of computer-assisted pedicle screw placement. An in vivo computed tomography analysis. Spine (Phila Pa 1976). 1997. 22: 452-8
9. Watanabe K, Lenke LG, Matsumoto M, Harimaya K, Kim YJ, Hensley M. A novel pedicle channel classification describing osseous anatomy: How many thoracic scoliotic pedicles have cancellous channels?. Spine (Phila Pa 1976). 2010. 35: 1836-42