- Department of Neurosurgery, University of California, Los Angeles, CA, USA
Correspondence Address:
Daniel C. Lu
Department of Neurosurgery, University of California, Los Angeles, CA, USA
DOI:10.4103/2152-7806.156603
Copyright: © 2015 Yew A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Yew A, Lu D, Lu DC. CT-based morphometric analysis of C1 laminar dimensions: C1 translaminar screw fixation is a feasible technique for salvage of atlantoaxial fusions. Surg Neurol Int 07-May-2015;6:
How to cite this URL: Yew A, Lu D, Lu DC. CT-based morphometric analysis of C1 laminar dimensions: C1 translaminar screw fixation is a feasible technique for salvage of atlantoaxial fusions. Surg Neurol Int 07-May-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/ct%e2%80%91based-morphometric-analysis-c1-laminar-dimensions-c1/
Abstract
Background:Translaminar screw fixation has become an alternative in the fixation of the axial and subaxial cervical spine. We report utilization of this approach in the atlas as a salvage technique for atlantoaxial stabilization when C1 lateral mass screws are precluded. To assess the feasibility of translaminar fixation at the atlas, we have characterized the dimensions of the C1 lamina in the general adult population using computed tomography (CT)-based morphometry.
Methods:A 46-year-old male with symptomatic atlantoaxial instability secondary to os odontoideum underwent bilateral C1 and C2 translaminar screw/rod fixation as C1 lateral mass fixation was precluded by an anomalous vertebral artery. The follow-up evaluation 2½ years postoperatively revealed an asymptomatic patient without recurrent neck/shoulder pain or clinical signs of instability. To better assess the feasibility of utilizing this approach in the general population, we retrospectively analyzed 502 consecutive cervical CT scans performed over a 3-month period in patients aged over 18 years at a single institution. Measurements of C1 bicortical diameter, bilateral laminar length, height, and angulation were performed. Laminar and screw dimensions were compared to assess instrumentation feasibility.
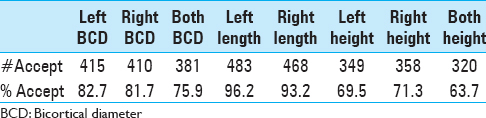
Results:Review of CT imaging found that 75.9% of C1 lamina had a sufficient bicortical diameter, and 63.7% of C1 lamina had sufficient height to accept bilateral translaminar screw placement.
Conclusions:CT-based measurement of atlas morphology in the general population revealed that a majority of C1 lamina had sufficient dimensions to accept translaminar screw placement. Although these screws appear to be a feasible alternative when lateral mass screws are precluded, further research is required to determine if they provide comparable fixation strength versus traditional instrumentation methods.
Keywords: Atlantoaxial fusion, translaminar fixation, C1-C2 fusion
INTRODUCTION
Previous literature has focused on the utilization of C2 translaminar screws.[
MATERIALS AND METHODS
Case report
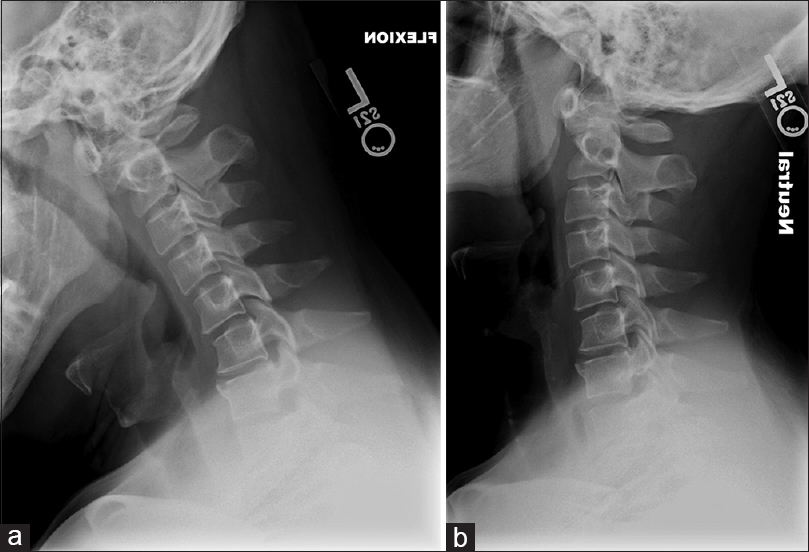
After a motor vehicle accident, a 46-year-old male presented with upper cervical midline tenderness and symptoms of a whiplash injury, but without myelopathy or radiculopathy. Plain and dynamic X-rays demonstrated an os odontoideum with 8 mm of C1/2 subluxation [Figure
CT based morphometric study
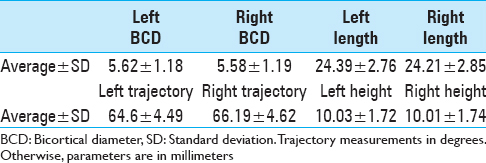
At UCLA Ronald Reagan Medical Center, 532 consecutive noncontrast CT scans of the cervical spine performed for any indication in patients aged >18 years were reviewed; 30 patients were excluded due to congenital C1 deformity, history of C1 fracture or laminectomy, or inadequate image quality. On axial CT images, bilateral C1 minimum bicortical diameters, laminar lengths, laminar angulation from the midline, and C1 laminar heights were measured (e.g., from mid-sagittal CT images). Laminar length measurements were directed from the midline along the axis of the lamina toward the lateral mass/laminar junction. Laminar angulation was defined as the angle between midline and the long axis of the lamina utilized in the length measurement. Lamina was deemed acceptable for translaminar screw placement if they possessed a minimum bicortical diameter of 4.5 mm, laminar height of 9 mm, and length of 20 mm. The difference in rate of screw acceptance by gender was analyzed using Fisher's exact test.
RESULTS
The 502 patients ranged from age 18 to 99 years with a mean age of 52.8 years, and included 303 males and 199 females. The average bicortical diameters, laminar lengths, laminar heights, and angulation from the midline are shown in
DISCUSSION
C2 translaminar screws have been documented to be a useful method of upper cervical fixation.[
Further, C2 translaminar screws have the advantage of decreased risk of vertebral artery injury as compared with C2 pars or pedicle screws. In fact, there are reports of groups using this method specifically in patients with prior unilateral occlusion of the vertebral artery for avoidance of vascular complications.[
We believe that translaminar fixation of the atlas has similar potential, and therefore undertook to measure average laminar dimensions in the general population in order to assess the feasibility of this approach. The measurement methods utilized in this study to assess C1 morphometric parameters are similar to methods described in the literature for measurement of lamina at other levels of the cervical spine.[
Our criterion for minimum diameter necessary to place translaminar screws is comparable with previous studies. There have been varying reports in the literature regarding the minimum diameter needed to safely place translaminar screws in the cervical spine.[
CONCLUSION
C1 lateral mass screws as described by Harms et al.[
ACKNOWLEDGMENT
This research was made possible with the generous support from J. Yang and Family Foundation. D.C.L. is a 1999 Paul and Daisy Soros New American Fellow.
References
1. Aepli M, Mannion AF, Grob D. Translaminar screw fixation of the lumbar spine: Long-term outcome. Spine. 2009. 34: 1492-8
2. Ahmed R, Traynelis VC, Menezes AH. Fusions at the craniovertebral junction. Childs Nerv Syst. 2008. 24: 1209-24
3. Alvin MD, Abdullah KG, Steinmetz MP, Lubelski D, Nowacki AS, Benzel EC. Translaminar screw fixation in the subaxial cervical spine: Quantitative laminar analysis and feasibility of unilateral and bilateral translaminar virtual screw placement. Spine. 2012. 37: E745-51
4. Cassinelli EH, Lee M, Skalak A, Ahn NU, Wright NM. Anatomic considerations for the placement of C2 laminar screws. Spine. 2006. 31: 2767-71
5. Chern JJ, Chamoun RB, Whitehead WE, Curry DJ, Luerssen TG, Jea A. Computed tomography morphometric analysis for axial and subaxial translaminar screw placement in the pediatric cervical spine. J Neurosurg Pediatr. 2009. 3: 121-8
6. Dmitriev AE, Lehman RA, Helgeson MD, Sasso RC, Kuhns C, Riew DK. Acute and long-term stability of atlantoaxial fixation methods: A biomechanical comparison of pars, pedicle, and intralaminar fixation in an intact and odontoid fracture model. Spine. 2009. 34: 365-70
7. Dorward IG, Wright NM. Seven years of experience with C2 translaminar screw fixation: Clinical series and review of the literature. Neurosurgery. 2011. 68: 1491-9
8. Grob D, Bartanusz V, Jeszenszky D, Kleinstuck FS, Lattig F, O’Riordan D. A prospective, cohort study comparing translaminar screw fixation with transforaminal lumbar interbody fusion and pedicle screw fixation for fusion of the degenerative lumbar spine. J Bone Joint Surg Br. 2009. 91: 1347-53
9. Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine. 2001. 26: 2467-71
10. Hong JT, Sung JH, Son BC, Lee SW, Park CK. Significance of laminar screw fixation in the subaxial cervical spine. Spine. 2008. 33: 1739-43
11. Jacobson ME, Khan SN, An HS. C1-C2 posterior fixation: Indications, technique, and results. Orthop Clin North Am. 2012. 43: 11-8
12. Jea A, Johnson KK, Whitehead WE, Luerssen TG. Translaminar screw fixation in the subaxial pediatric cervical spine. J Neurosurg Pediatr. 2008. 2: 386-90
13. Kretzer RM, Sciubba DM, Bagley CA, Wolinsky JP, Gokaslan ZL, Garonzik IM. Translaminar screw fixation in the upper thoracic spine. J Neurosurg Spine. 2006. 5: 527-33
14. Mandel IM, Kambach BJ, Petersilge CA, Johnstone B, Yoo JU. Morphologic considerations of C2 isthmus dimensions for the placement of transarticular screws. Spine. 2000. 25: 1542-7
15. Matsubara T, Mizutani J, Fukuoka M, Hatoh T, Kojima H, Otsuka T. Safe atlantoaxial fixation using a laminar screw (intralaminar screw) in a patient with unilateral occlusion of vertebral artery: Case report. Spine. 2007. 32: E30-3
16. McGirt MJ, Sutter EG, Xu R, Sciubba DM, Wolinsky JP, Witham TF. Biomechanical comparison of translaminar versus pedicle screws at T1 and T2 in long subaxial cervical constructs. Neurosurgery. 2009. 65: S167-72
17. Menezes AH. Craniocervical fusions in children. J Neurosurg Pediatr. 2012. 9: 573-85
18. Molina C, Sciubba DM, Chaput C, Tortolani PJ, Jallo GI, Kretzer RM. A computed tomography-based feasibility study of translaminar screw placement in the pediatric thoracic spine. J Neurosurg Pediatr. 2012. 9: 27-34
19. Parker SL, McGirt MJ, Garces-Ambrossi GL, Mehta VA, Sciubba DM, Witham TF. Translaminar versus pedicle screw fixation of C2: Comparison of surgical morbidity and accuracy of 313 consecutive screws. Neurosurgery. 2009. 64: S343-8
20. Patel RD, Rosas HG, Steinmetz MP, Anderson PA. Repair of pars interarticularis defect utilizing a pedicle and laminar screw construct: A new technique based on anatomical and biomechanical analysis. J Neurosurg Spine. 2012. 17: 61-8
21. Pelton MA, Schwartz J, Singh K. Subaxial cervical and cervicothoracic fixation techniques--indications, techniques, and outcomes. Orthop Clin North Am. 2012. 43: 19-28
22. Wang MY. C2 crossing laminar screws: Cadaveric morphometric analysis. Neurosurgery. 2006. 59: ONS84-8
23. Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: Case series and technical note. J Spinal Disord Tech. 2004. 17: 158-62
24. Xia DD, Lin SL, Chen W, Shen ZH, Li Y, Wang XY. Computed tomography morphometric analysis of C2 translaminar screw fixation of Wright's technique and a modified technique in the pediatric cervical spine. Eur Spine J. 2014. 23: 606-12