- Department of Neurosurgery, Faculty of Medicine Universitas Airlangga - Dr. Soetomo General Academic Hospital, Surabaya, East Java, Indonesia.
Correspondence Address:
Joni Wahyuhadi, Department of Neurosurgery, Faculty of Medicine Universitas Airlangga - Dr. Soetomo General Academic Hospital, Surabaya, East Java, Indonesia.
DOI:10.25259/SNI_948_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Irwan Barlian Immadoel Haq, Andhika Tomy Permana, Rahadian Indarto Susilo, Joni Wahyuhadi. Deadly complication of sacrificing superior petrosal vein during cerebellopontine angle tumor resection: A case report and literature review. 28-Jun-2021;12:306
How to cite this URL: Irwan Barlian Immadoel Haq, Andhika Tomy Permana, Rahadian Indarto Susilo, Joni Wahyuhadi. Deadly complication of sacrificing superior petrosal vein during cerebellopontine angle tumor resection: A case report and literature review. 28-Jun-2021;12:306. Available from: https://surgicalneurologyint.com/surgicalint-articles/10930/
Abstract
Background: Tumors of the cerebellopontine angle (CPA) are challenging to resect and have been proven difficult for neurosurgeons to manage optimally. Superior petrosal vein complex (SPVC) as the main drainage system and close proximity to CPA could be an obstacle during operation. There is an incidence ranging from 55% to 84% of injury to one part of the SPVC during CPA tumor surgery.
Case Description: We report a case of 65-year-old woman with CPA tumor, who complained of unilateral hearing loss, dizziness, and facial pain. During tumor resection, one part of SPV complex was injured, then cerebellar edema develops.
Conclusion:
Keywords: Cerebellopontine angle, Meningioma, Sacrifice, Superior petrosal vein, Tumor resection
INTRODUCTION
Meningiomas account for 26% of primary intracranial neoplasms. Among intracranial meningiomas, 5–10% are located in the cerebellopontine angle (CPA).[
CPA often enabling complete surgical removal. However, complete removal can carry potential risks that may be significant, especially when the tumor has invaded brain tissue or surrounding veins.[
Attention has been paid to SPVs during surgeries for tumor in the upper CPA, and the number of reports on associated complications, especially during meningioma surgeries, has recently increased.[
Subsequently, sacrifice of veins is common practice to gain surgical exposure.[
ILLUSTRATIVE CASE
History and examination
A 65-year-old woman was referred from the previous hospital with some symptoms of a CPA tumor. She reported a history of pain on her cheeks and lower jaw. She also complained about left ear hearing loss and dizziness. These symptoms have appeared for 6 months and are getting worse. Neurological examination revealed cranial nerve V, VII, and VIII abnormalities. The patient had already been informed and consent regarding the publication of her data.
Radiological findings
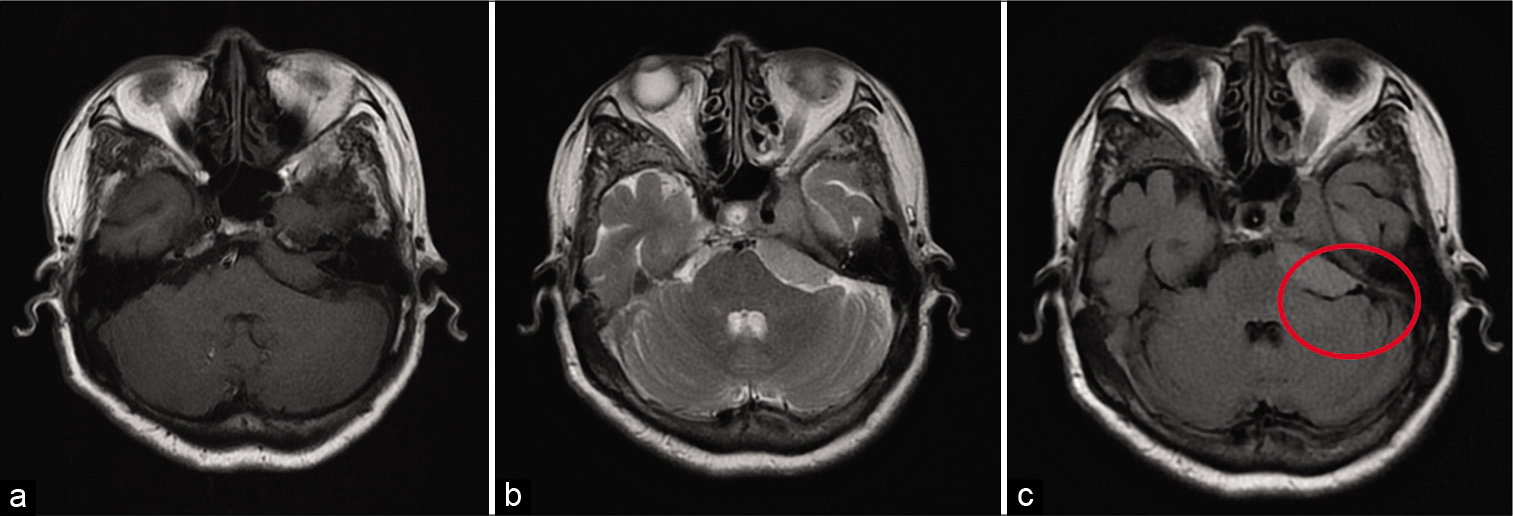
Magnetic resonance imaging without contrast was performed at previous hospital and showed a lesion at left CPA [
Operation and postoperative reports
Surgery was initiated with park-bench position, retrosigmoid craniotomy, and exploration of the CPA. It appears that the cerebellum relaxes and the left cerebellopontine exposes after the cisterna magna was opened and cerebrospinal fluid was released.
Arachnoid detachment was performed to separate the tumor from the cerebellar tissue. During surgical debulking of tumor, the left SPV attached to the tumor was cut off. Coagulation technique with bipolar cautery to stop bleeding was given immediately. The surgeon noticed progressive cerebellar swelling and the CPA becomes inaccessible a 15 min later. Cerebellar tissue begins to swell and extends beyond the border of the craniotomy. In consequence, the craniotomy was widened so that we could remove the rest of tumor. Bone flap was not put back in place. Dural graft was chosen to be placed over the cerebellar tissue followed by closure of the muscle, fascia, and skin.
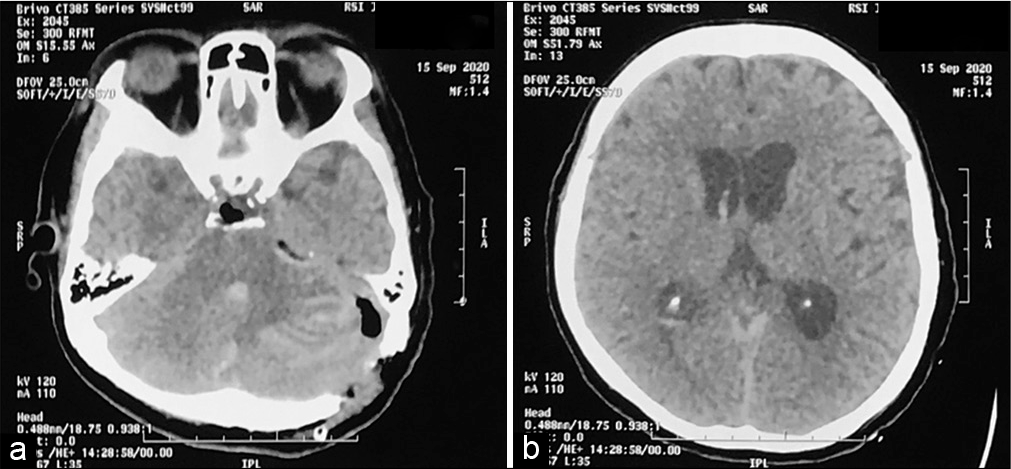
The patient was transferred in radiology for an emergency computed tomography (CT) scan and the results showed left cerebellar edema and hemorrhage with concomitant developing hydrocephalus [
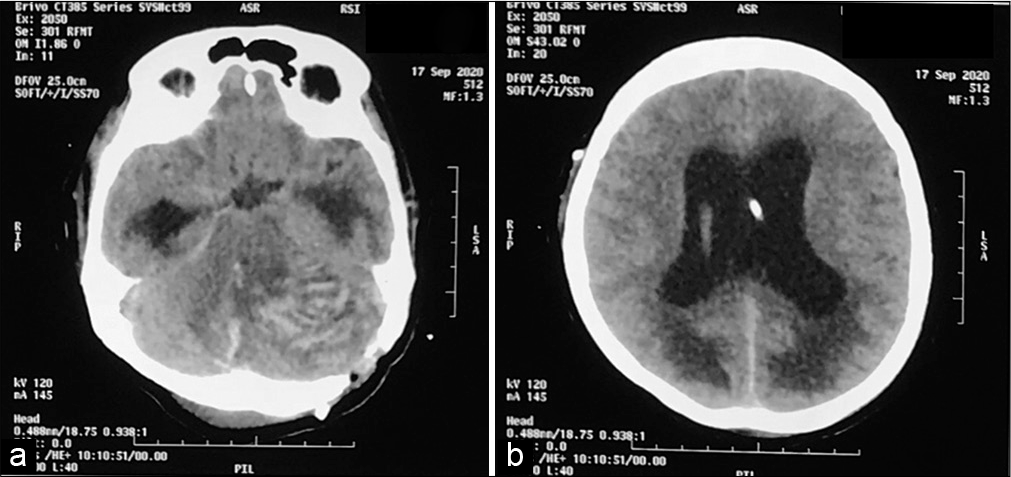
The patient was transferred back to the operating room and the Kocher’s point for the right external ventricular drainage was positioned. The patient was then transferred to the intensive care unit and remained sedated for 24 h. Another head CT scan was performed and showed an advancement of hemorrhage [
When sedation is stopped, the pupils are small and unreactive. The patient does not respond to pain, verbal, and eye stimulation. Glasgow Coma Scale is 3. No corneal reflex. The patient died 24 h later.
DISCUSSION
Anatomical perspective of SPV
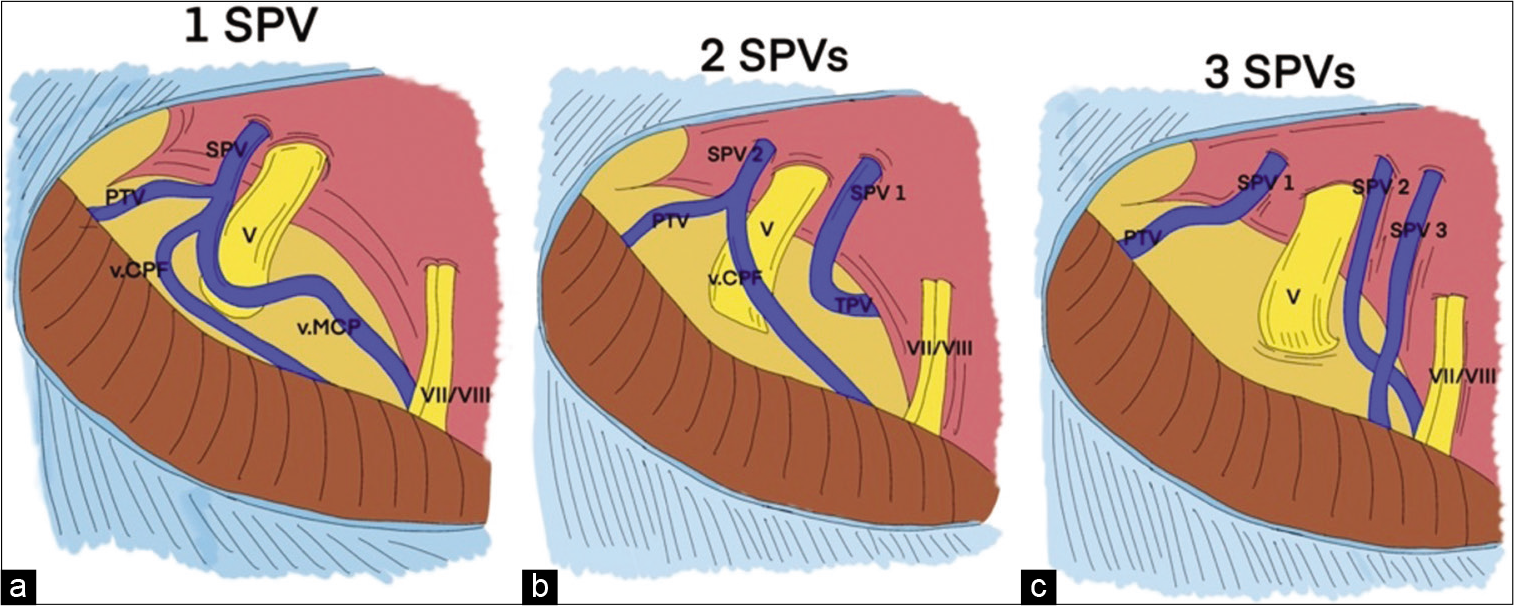
The venous drainage of the SPV has many variations. These veins are among the largest and the most frequent veins in the posterior fossa. The SPVs drain the anterior and lateral surfaces of the brainstem, the petrosal surface, and some lateral parts of the tentorial and suboccipital surfaces.[
After SPV obliteration, compensatory venous blood drainage seems to occur through anastomotic pathways directed to the ipsilateral supratentorial deep veins. Anastomoses to the contralateral petrosal vein system do not suffice to install an adequate outflow.[
Clinical implication of SPV occlusion
CPA has always proven difficult for neurosurgeons to optimally manage,[
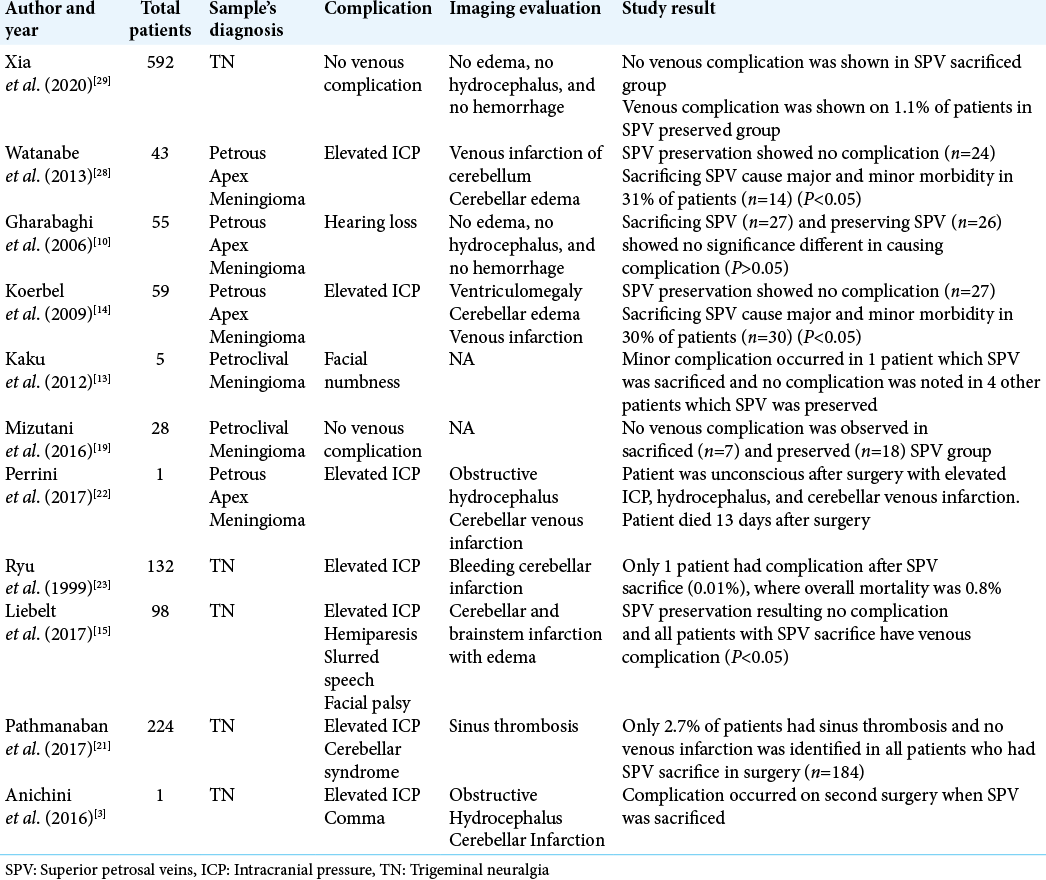
Coagulation and dissection of the SPV do not frequently cause adverse sequelae. Several large series study of sacrificing SPV in petrous tumor showed negligible complication, in a study of 55 patients with petrous meningioma surgery, the SPV was sacrificed in 49% of the case and only 3 patients had hearing loss complication, compared with other group which SPV was preserved, 3 patients also had hearing loss complication (P > 0.05).[
Another study conducted in sacrificing SPV showed the benefit of venography before surgery to identify SPV type and its tributary, helping surgeon decision to preserve or to sacrifice the SPV. This study described no venous complication for all patient who underwent surgery with sacrificing or preserving SPV with 1 patient as SPV Type 1, 2 patients as SPV Type 2 and 4 patients as SPV Type 3 in sacrificed group, and 17 patients as SPV Type 2 and 1 patient as SPV Type 3.[
Larger study supporting the safety of sacrificing SPV was conducted in microvascular decompression (MVD) procedure for trigeminal neuralgia (TN). A study in 4400 patients underwent MVD procedure for TN showed that SPV is safe to be sectioned without causing major morbidity or mortality.[
In the opposite hand, several studies reported some devastating effect due to sacrificing of SPV [
In general, one out of several tributaries of the SPV or tentorial veins was considered safe to occlude, although most surgeon considered certain risks of infarction and edema with any venous occlusion [
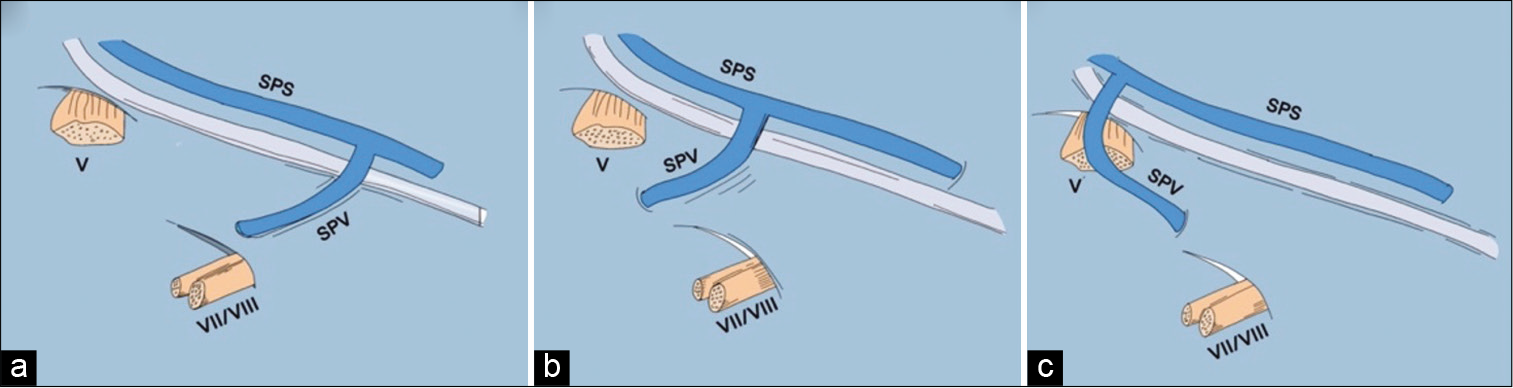
Figure 5:
The three main patterns of an SPVC. (a) An SPVC with single SPV, (b) an SPVC with 2 SPVs, (c) an SPVC with 3 SPVs. ALMv: Anterior lateral marginal vein, PTv: Pontotrigeminal vein, SPS: Superior petrosal sinus, SPV: Superior petrosal vein, SPVC: Superior petrosal vein complex, SPV1: First superior petrosal vein, SPV2: Second superior petrosal vein, SPV3: Third superior petrosal vein, TPv: Transverse pontine vein, v.CPF: Vein of cerebellopontine fissure, v.MCP: Vein of the middle cerebellar peduncle, V: Trigeminal nerve, VII/ VIII: Seventh and eighth cranial nerves.[
Sacrifice of veins rarely leads to complications (1.6% on average, according to reports). Nevertheless, some may be severe and even life threatening and necessitate emergency management.[
Neurosurgeons commonly sacrifice SPV to widen the operative exposure at the apex.[
Effort should be made to avoid the complication of sectioned SPV. Although not always possible, radiological study of venous anatomical variation through venography in each patient could tell the surgeon whether it is safe or not to sacrifice the SPV and its tributaries.[
Another way of assessing the safety of SPV sacrifice can also be done intraoperatively with temporary clamping of SPV. Assessment can be made in plain view to assess the edema, but a more objective report by monitoring the auditory potential of the brain stem has been reported.[
Surgical technique with combined petrosal approach, SPV preservation, and dural incision approach described in previous report could be used to increase the probability to preserve SPV.[
Similarly, the use of fully endoscopic and endoscope-assisted microsurgery with and without angled optics may minimize the extent of venous sacrifice required to obtain optimum visualization. The risk of inadvertent injury to a preserved SPV with resultant bleeding into the CPA seems unlikely to be improved with this approach however and may be worse due to loss of vision for structures superficial to the tip of the endoscope. Furthermore, management of such bleeding in the CPA may be problematic with an endoscope, where a clear view of the field can be lost. Subsequently, although the problem is often not discussed in the endoscopic literature, some authors describe sacrifice of the SPV when it is encountered to improve endoscopic exposure as with the microscopic technique.[
CONCLUSION
The surgeon must fully understand the essential anatomical knowledge of the veins to assess surgical risk and assess feasibility of venous sacrifice. The decision not to sacrifice SPV should be made during CPA tumor resection or other intracanal case surgery because of the potentially lethal complication. According to this case, there are several options that could be made, that is, preservation of the veins, temporary vein clamping followed by intraoperative evaluation, preoperative venography to consider the safety of sacrificing SPV complex, and avoiding long and continuous retraction of cerebellum.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agarwal V, Babu R, Grier J, Adogwa O, Back A, Friedman AH. Cerebellopontine angle meningiomas: Postoperative outcomes in a modern cohort. Neurosurg Focus. 2013. 35: E10
2. Alaoui-Ismaili A, Krogager ME, Jakola AS, Poulsgaard L, Couldwell W, Mathiesen T. Surgeons’ experience of venous risk with CPA surgery. Neurosurg Rev. 2020. 2020: 01365-5
3. Anichini G, Iqbal M, Rafiq NM, Ironside JW, Kamel M. Sacrificing the superior petrosal vein during microvascular decompression. Is it safe? Learning the hard way. Case report and review of literature. Surg Neurol Int. 2016. 7: S415-20
4. Basamh M, Sinning N, Kehler U. Individual variations of the superior petrosal vein complex and their microsurgical relevance in 50 cases of trigeminal microvascular decompression. Acta Neurochir (Wien). 2020. 162: 197-209
5. Belachew A, Chowdhury T, Spiriev T, Sandu N, Schaller B. Classification of Meningiomas. Springer Sci Media. 2015. 14: 43-53
6. Dumot C, Sindou M. Veins of the cerebellopontine angle and specific complications of sacrifice, with special emphasis on microvascular decompression surgery. A review. World Neurosurg. 2018. 117: 422-32
7. Elhammady MS, Heros RC. Cerebral veins: To sacrifice or not to sacrifice, that is the question. World Neurosurg. 2015. 83: 320-4
8. Ferroli P, Nakaji P, Acerbi F, Albanese E, Broggi G. Indocyanine green (ICG) temporary clipping test to assess collateral circulation before venous sacrifice. World Neurosurg. 2011. 75: 122-5
9. Gao K, Ma H, Cui Y, Chen X, Ma J, Dai J. Meningiomas of the cerebellopontine angle: Radiological differences in tumors with internal auditory canal involvement and their influence on surgical outcome. PLoS One. 2015. 10: e0122949
10. Gharabaghi A, Koerbel A, Löwenheim H, Kaminsky J, Samii M, Tatagiba M. The impact of petrosal vein preservation on postoperative auditory function in surgery of petrous apex meningiomas. Neurosurgery. 2006. 59: ONS68-74
11. Haq IB, Susilo RI, Goto T, Ohata K. Dural incision in the petrosal approach with preservation of the superior petrosal vein. J Neurosurg. 2016. 124: 1074-8
12. He X, Liu W, Wang Y, Zhang J, Liang B, Huang JH. Surgical management and outcome experience of 53 cerebellopontine angle meningiomas. Cureus. 2017. 9: e1538
13. Kaku S, Miyahara K, Fujitsu K, Hataoka S, Tanino S, Okada T. Drainage pathway of the superior petrosal vein evaluated by CT venography in petroclival meningioma surgery. J Neurol Surg B Skull Base. 2012. 73: 316-20
14. Koerbel A, Gharabaghi A, Safavi-Abbasi S, Samii A, Ebner FH, Samii M. Venous complications following petrosal vein sectioning in surgery of petrous apex meningiomas. Eur J Surg Oncol. 2009. 35: 773-9
15. Liebelt BD, Barber SM, Desai VR, Harper R, Zhang J, Parrish R. Superior Petrosal vein sacrifice during microvascular decompression: Perioperative complication rates and comparison with venous preservation. World Neurosurg. 2017. 104: 788-94
16. Matsushima T, Kawashima M, Inoue K, Matsushima K. Anatomy of the superior petrosal veins and their exposure and management during petrous apex meningioma surgery using the lateral suboccipital retrosigmoid approach. Neurosurg Rev. 2014. 37: 535-456
17. Matsushima T, Rhoton AL, de Oliveira E, Peace D. Microsurgical anatomy of the veins of the posterior fossa. J Neurosurg. 1983. 59: 63-105
18. McLaughlin MR, Jannetta PJ, Clyde BL, Subach BR, Comey CH, Resnick DK. Microvascular decompression of cranial nerves: Lessons learned after 4400 operations. J Neurosurg. 1999. 90: 1-8
19. Mizutani K, Toda M, Yoshida K. The Analysis of the petrosal vein to prevent venous complications during the anterior transpetrosal approach in the resection of petroclival meningioma. World Neurosurg. 2016. 93: 175-82
20. Narayan V, Savardekar AR, Patra DP, Mohammed N, Thakur JD, Riaz M. Safety profile of superior petrosal vein (the vein of Dandy) sacrifice in neurosurgical procedures: A systematic review. Neurosurg Focus. 2018. 45: E3
21. Pathmanaban ON, O’Brien F, Al-Tamimi YZ, Hammerbeck-Ward CL, Rutherford SA, King AT. Safety of superior petrosal vein sacrifice during microvascular decompression of the trigeminal nerve. World Neurosurg. 2017. 103: 84-7
22. Perrini P, Di Russo P, Benedetto N. Fatal cerebellar infarction after sacrifice of the superior petrosal vein during surgery for petrosal apex meningioma. J Clin Neurosci. 2017. 35: 144-5
23. Ryu H, Yamamoto S, Sugiyama K, Yokota N, Tanaka T. Neurovascular decompression for trigeminal neuralgia in elderly patients. Neurol Med Chir (Tokyo). 1999. 39: 226-9
24. Samii M, Tatagiba M, Carvalho GA. Retrosigmoid intradural suprameatal approach to Meckel’s cave and the middle fossa: Surgical technique and outcome. J Neurosurg. 2000. 92: 235-41
25. Spena G, Sorrentino T, Altieri R, Zinis LR, Stefini R, Panciani PP. Early-career surgical practice for cerebellopontine angle tumors in the era of radiosurgery. J Neurol Surg B Skull Base. 2018. 79: 269-81
26. Strauss C, Neu M, Bischoff B, Romstöck J. Clinical and neurophysiological observations after superior petrosal vein obstruction during surgery of the cerebellopontine angle: Case report. Neurosurgery. 2001. 48: 1157-9
27. Tanriover N, Abe H, Rhoton AL, Kawashima M, Sanus GZ, Akar Z. Microsurgical anatomy of the superior petrosal venous complex: New classifications and implications for subtemporal transtentorial and retrosigmoid suprameatal approaches. J Neurosurg. 2007. 106: 1041-50
28. Watanabe T, Igarashi T, Fukushima T, Yoshino A, Katayama Y. Anatomical variation of superior petrosal vein and its management during surgery for cerebellopontine angle meningiomas. Acta Neurochir (Wien). 2013. 155: 1871-8
29. Xia Y, Kim TY, Mashouf LA, Patel KK, Xu R, Casaos J. Absence of ischemic injury after sacrificing the superior petrosal vein during microvascular decompression. Oper Neurosurg (Hagerstown). 2020. 18: 316-20
30. Zhong J, Li ST, Xu SQ, Wan L, Wang X. Management of petrosal veins during microvascular decompression for trigeminal neuralgia. Neurol Res. 2008. 30: 697-700