- Department of Neurosurgery, National Institute of Neurology and Neurosurgery, Mexico City, Mexico,
- Department of Neurosurgery, Hospital Padilla de Tucuman, Tucuman, Argentina.
Correspondence Address:
Marcos V Sangrador-Deitos, Department of Neurosurgery, National Institute of Neurology and Neurosurgery, Mexico City, Mexico.
DOI:10.25259/SNI_349_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marcos V Sangrador-Deitos1, Gerardo Y Guinto-Nishimura1, Luis A Rodriguez-Hernandez1, Alvaro Campero2. Defining the limits of the anterior wall of the cavernous sinus through an endoscopic view: Cadaveric anatomical study. 21-Jul-2023;14:258
How to cite this URL: Marcos V Sangrador-Deitos1, Gerardo Y Guinto-Nishimura1, Luis A Rodriguez-Hernandez1, Alvaro Campero2. Defining the limits of the anterior wall of the cavernous sinus through an endoscopic view: Cadaveric anatomical study. 21-Jul-2023;14:258. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12447
Abstract
Background: The anterior wall of the cavernous sinus (CS) represents an important landmark for endoscopic surgery that although mentioned before, no precise anatomical boundaries have been described. We describe the anatomical landmarks that delimit the anterior wall of the CS, emphasizing its importance as a reference for accessing the CS through endoscopic approaches.
Methods: Six adult cadaveric heads fixed with formaldehyde and injected with colored silicone were studied. In all the heads, an endonasal endoscopic approach to the sellar and parasellar regions was performed and the anatomy of the anterior wall of the CS was studied.
Results: Four consistent anatomical landmarks that mark the limits of the anterior wall of the CS were found in all the specimens: anterosuperiorly, the lateral opticocarotid recess; posterosuperiorly, the medial opticocarotid recess; anteroinferiorly, the inferior part of the maxillary strut; and posteroinferiorly, the superolateral angle of the clival recess.
Conclusion: It is of paramount importance to recognize the anatomical landmarks that define the limits of the anterior wall of the CS to achieve a safe access to this so complex region.
Keywords: Anterior wall, Boundaries, Cavernous sinus, Endoscopic, Skull base
INTRODUCTION
The cavernous sinus (CS) is a paired structure located on each side of the sella, pituitary gland, and sphenoid sinus, extending from the superior orbital fissure rostrally to the dorsum sellae caudally. It is defined as the dural envelope through which the cavernous segment of the internal carotid artery (ICA) courses, as well as venous outflow from the orbital, sphenoidal, and temporal regions.[
The aim of the present study is to describe the endoscopic anatomy of the anterior wall of the CS, delimit its anatomical borders, and highlight its importance as an anatomical reference for endoscopic approaches to the CS and surrounding areas.
MATERIALS AND METHODS
Six heads (12 sides) of adult cadavers fixed with formaldehyde and injected with colored silicone (red for arterial system and blue for venous system) were dissected. All the specimens were dissected bilaterally through an endonasal approach (medial to lateral dissection) using neurosurgical endoscopic instruments, including 4-mm diameter and 18 cm length 0° and 30° endoscopes coupled to a high-definition camera Image1 S H3-Link system (Karl Storz, Germany). A Midas Rex high-speed drill was used to remove bone tissue (Medtronic, USA). Two-handed binostril techniques were used. The configuration of the anterior wall of the CS, its relationship with nearby neurovascular structures, and its anatomical boundaries were studied. Measurements of distances between predefined anatomical landmarks were performed in all specimens (12 sides), obtained by direct measurement with a scientific divider, and then calculated using a slide caliper in unit of 0.1 mm. All measurements were made by a single investigator. Data were analyzed as continuous variables in STATA 17 software package (College Station, TX, StataCorp LLC) obtaining means, medians, standard deviations, and ranges. No ethics committee approval was sought or required to complete this study.
RESULTS
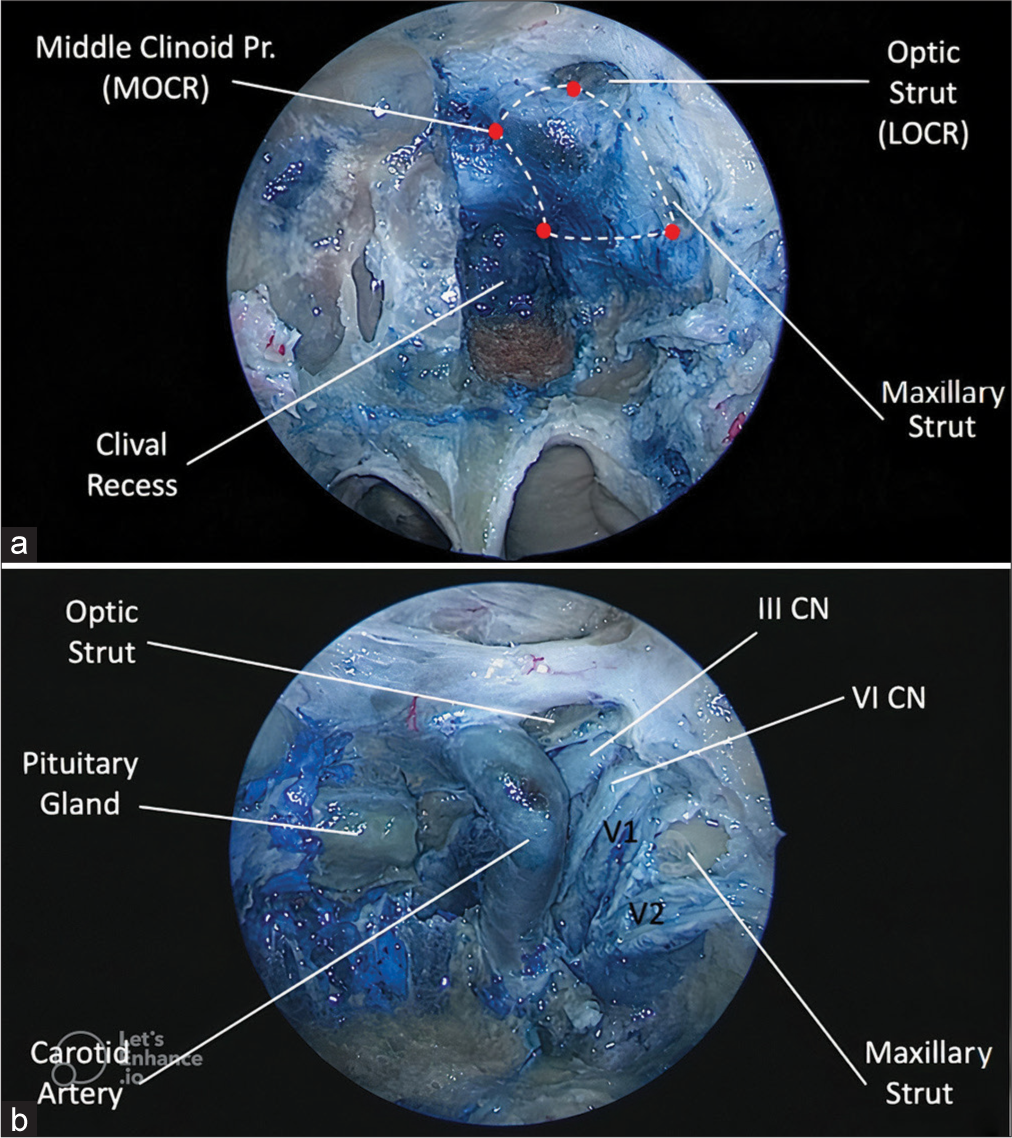
Surgical anatomy of the anterior wall of the CS
The anterior and inferior surfaces of the pituitary gland are covered by two layers of dura mater: the meningeal or inner layer, which adheres to the gland; and the periosteal or outer layer, which lies in contact with the sellar floor of the sphenoid bone. At the site where the sellar floor and the carotid sulcus transition, these dural layers split, the periosteal layer continues laterally to form the anterior wall of the CS, and the meningeal layer continues posteriorly at each side of the pituitary gland to form the medial wall of the CS.[
Defining the limits of the anterior wall of the CS
The standard endonasal endoscopic approach was performed as described elsewhere.[
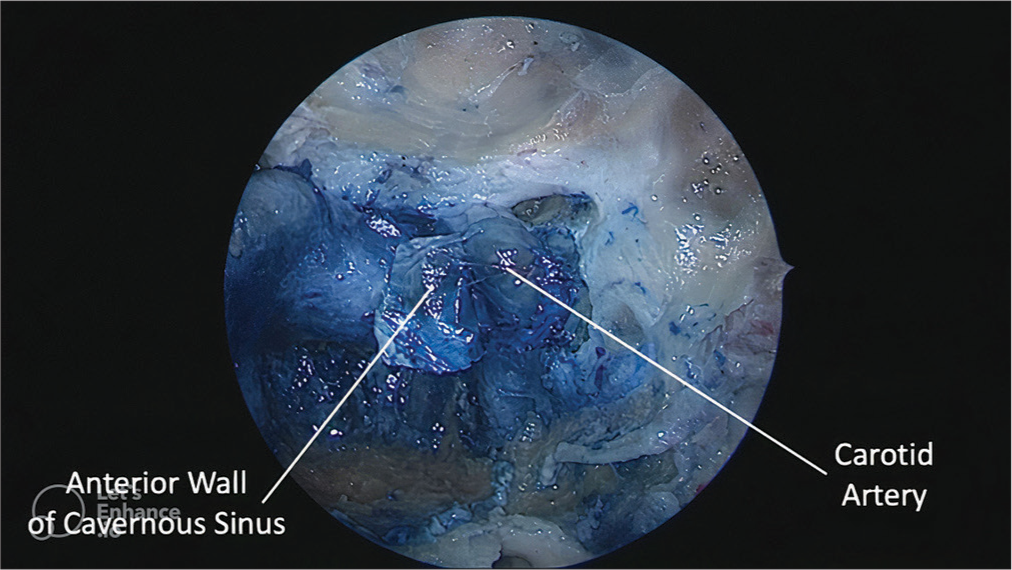
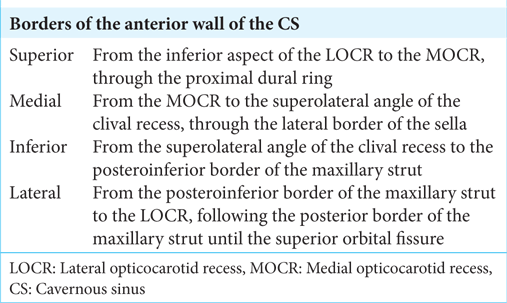
Figure 2:
Endoscopic view of the left anterior wall of the cavernous sinus (CS). (a) The bone overlying the pituitary gland and the internal carotid artery (ICA) has been removed in the left side. The limits of the anterior wall are defined as follows: anterosuperiorly, by the lateral opticocarotid recess; posterosuperiorly, by the medial opticocarotid recess; anteroinferiorly, by the posteroinferior margin of the maxillary strut; and posteroinferiorly, by the superolateral angle of the clival recess. (b) The single layer of dura covering the anterior wall has been removed and the neurovascular contents of the CS are exposed, including the parasellar segment of the ICA, and the medial margins of III CN, VI CN, V1, and V2. III CN: Oculomotor nerve, VI CN: Abducens nerve, LOCR: Lateral opticocarotid recess, MOCR: Medial opticocarotid recess, V1: Ophthalmic nerve, V2: maxillary nerve.
These anatomical landmarks and their intracranial relationship from a dorsolateral perspective possess significant surgical relevance. The LOCR corresponds to the optic strut base, which divides the optic canal superomedially from the superior orbital fissure inferolaterally, and forms the anterosuperior limit of the anterior wall of the CS.[
The MOCR is a teardrop-shaped osseous depression formed at the convergence point of the optic canal, carotid sulcus, CS, superior aspect of the sella, and anterior cranial base, located at each side of the tuberculum recess, and forms the posterosuperior limit of the anterior wall of the CS. Although not corresponding exactly with the middle clinoid process, this osseous prominence provides a useful and surgically relevant landmark.[
Four intervals were defined: distance A-B (from the LOCR to the MOCR); distance B-C (from the MOCR to the superolateral angle of the clival recess); C-D (from the superolateral angle of the clival recess to the posteroinferior margin of the maxillary strut); and D-A (from the posteroinferior margin of the maxillary strut to the LOCR) [
DISCUSSION
A proper understanding of the dural layers that form both the anterior and medial walls of the CS is of paramount importance. Although the concept of “anterior wall of the CS” has been previously mentioned in some publications, the exact anatomical landmarks that define this region have not been described before.[
Previously, the descriptions of the medial wall of the CS were made by visualizing it through transcranial approaches, which made it impossible to speak of an anterior wall of the CS, but now, with endoscopic endonasal approaches that project a direct vision of the CS from another perspective, it is possible to precisely describe the anterior wall of the CS in addition to the concept of the sphenoid segment of the medial wall.
However, a clarification of these two concepts is mandatory and particularly useful in endonasal endoscopic surgery. According to Yasuda et al.,[
Through a dorsolateral perspective, the anterior border of the medial wall of the CS has been classically described as being attached to the margins of the superior orbital fissure,[
Defining the borders of the anterior wall of the CS might improve the understanding of the extension of certain tumors that secondarily involve this structure. For instance, in cases of pituitary adenomas with important CS invasion, the limits of the anterior wall of the CS may guide the extent of the approach to achieve a complete resection, assuming that the tumor is located entirely within the CS.
Another potential application of the correct identification of the anterior wall of the CS is illustrated by Fernandez-Miranda et al.,[
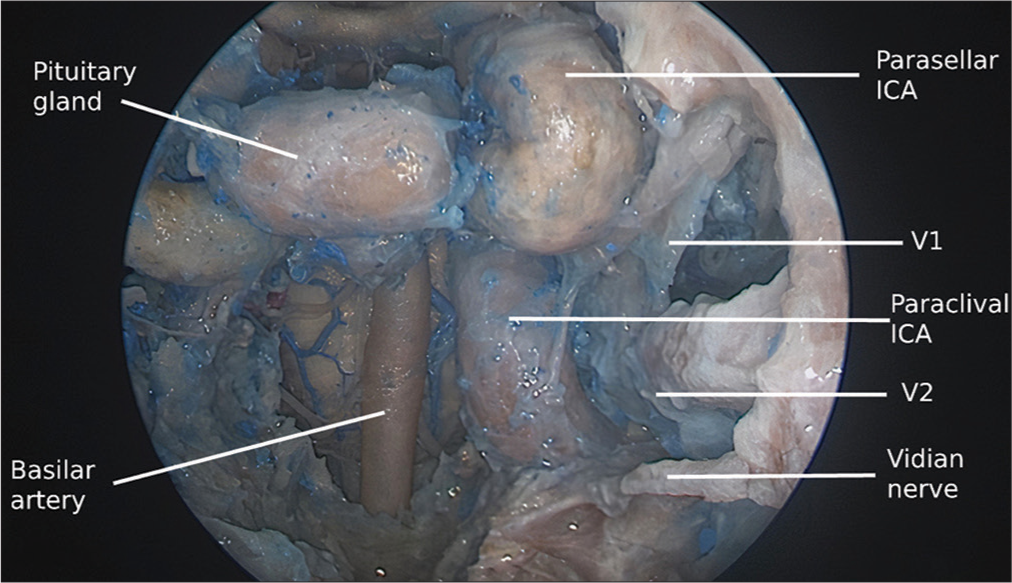
Figure 4:
Dural opening of the lateral portion of the anterior wall of the CS allows for access to the lateral compartment of the cavernous sinus (CS). The internal carotid artery is being retracted medially and the VI CN can be seen as it enters the posterior wall of the CS. VI CN: Abducens nerve, CS: Cavernous sinus, ICA: Internal carotid artery.
To enhance the understanding of the lateral border of the anterior wall of the CS, the anatomical landmarks can be extrapolated to the findings that are seen through dorsolateral microsurgical approaches to the CS and other transcavernous approaches. From a dorsolateral perspective, the anterior border of the CS has been described to attach to the superior orbital fissure, while the inferior border is described to course at the inferior border of the ophthalmic nerve.[
The identification of the lateral border of the anterior wall of the CS may also be useful for other nontumoral pathologies such as encephaloceles and CSF leaks. In these cases, the defect can be found anterior to this structure, thus guiding the extent of bone removal for an adequate exposure in the lateral recess of the sphenoid.[
It is important to note that the anatomy herein described should not be expected to be similar in cases of tumors extending to the CS. A tumor presenting cavernous invasion may bulge the anterior wall of the CS and significantly distort its usual appearance. Furthermore, these lesions may also displace the intracavernous structures depending on the origin and growth pattern of the tumor. For this reason, adjuvant tools (i.e., image-guidance systems, intraoperative Doppler, and recently, intraoperative ICG)[
We consider that a precise anatomical description and the definition of the endoscopic limits for the anterior wall of the CS are of paramount importance for the neurosurgeon as this provides a simple yet helpful landmark to guide a safe access to the CS and to other surrounding areas.
CONCLUSION
The anterior wall of the CS represents the most rostral access door to the CS and its contents through endoscopic approaches. It is necessary to describe its limits and adopt a uniform anatomical language to properly understand this so complex area.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alikhani P, Sivakanthan S, van Loveren H, Agazzi S. Paraclival or cavernous internal carotid artery: One segment but two names. J Neurol Surg B Skull Base. 2016. 77: 304-7
2. Barges-Coll J, Fernandez-Miranda JC, Prevedello DM, Gardner P, Morera V, Madhok R. Avoiding injury to the abducens nerve during expanded endonasal endoscopic surgery: Anatomic and clinical case studies. Neurosurgery. 2010. 67: 144-54
3. Campero A, Campero AA, Martins C, Yasuda A, Rhoton AL. Surgical anatomy of the dural walls of the cavernous sinus. J Clin Neurosci. 2010. 17: 746-50
4. Catapano G, Sgulò F, Laleva L, Columbano L, Dallan I, de Notaris M. Multimodal use of indocyanine green endoscopy in neurosurgery: A single-center experience and review of the literature. Neurosurg Rev. 2018. 41: 985-98
5. Drazin D, Wang JM, Alonso F, Patel DM, Granger A, Shoja MM. Intracranial anatomical triangles: A comprehensive illustrated review. Cureus. 2017. 9: e1741
6. Fernandez-Miranda JC, Gardner PA, Rastelli MM, Peris-Celda M, Koutourousiou M, Peace D. Endoscopic endonasal transcavernous posterior clinoidectomy with interdural pituitary transposition. J Neurosurg. 2014. 121: 91-9
7. Fernandez-Miranda JC, Zwagerman NT, Abhinav K, Lieber S, Wang EC, Snyderman CH. Cavernous sinus compartments from the endoscopic endonasal approach: Anatomical considerations and surgical relevance to adenoma surgery. J Neurosurg. 2018. 129: 430-41
8. Fernandez-Miranda JC, Tormenti M, Latorre F, Gardner P, Snyderman C. Endoscopic endonasal middle clinoidectomy: Anatomic, radiological, and technical note. Neurosurgery. 2012. 71: ons233-9
9. Gómez-Amador JL, Sangrador-Deitos MV, Guinto-Nishimura GY, Alvear-Quito NM. Middle transclival endoscopic endonasal resection of a ventral pontine cavernous malformation. World Neurosurg. 2022. 158: 34-5
10. Grewal SS, Kurbanov A, Anaizi A, Keller JT, Theodosopoulos PV, Zimmer LA. Endoscopic endonasal approach to the maxillary strut: Anatomical review and case series. Laryngoscope. 2014. 124: 1739-43
11. Krayenbühl N, Hafez A, Hernesniemi JA, Krisht AF. Taming the cavernous sinus: Technique of hemostasis using fibrin glue. Neurosurgery. 2007. 61: E52
12. Kirtane MV, Lall A, Chavan K, Satwalekar D. Endoscopic repair of lateral sphenoid recess cerebrospinal fluid leaks. Indian J Otolaryngol Head Neck Surg. 2012. 64: 188-92
13. Kassam AB, Prevedello DM, Carrau RL, Snyderman CH, Gardner P, Osawa S. The front door to Meckel’s cave: An anteromedial corridor via expanded endoscopic endonasal approach-technical considerations and clinical series. Neurosurgery. 2009. 64: ons71-82
14. Labib MA, Prevedello DM, Carrau R, Kerr EE, Naudy C, Al-Shaar HA. A road map to the internal carotid artery in expanded endoscopic endonasal approaches to the ventral cranial base. Neurosurgery. 2014. 10: 448-71
15. Labib MA, Prevedello DM, Fernandez-Miranda JC, Sivakanthan S, Benet A, Morera V. The medial opticocarotid recess: An anatomic study of an endoscopic “key landmark” for the ventral cranial base. Neurosurgery. 2013. 72: 66-76
16. Peris-Celda M, Kucukyuruk B, Monroy-Sosa A, Funaki T, Valentine R, Rhoton AL. The recesses of the sellar wall of the sphenoid sinus and their intracranial relationships. Neurosurgery. 2013. 73: ons117-31
17. Rhoton AL. The cavernous sinus, the cavernous venous plexus, and the carotid collar. Neurosurgery. 2002. 51: S375-410
18. Schmidt RF, Choudhry OJ, Raviv J, Baredes S, Casiano RR, Eloy JA. Surgical nuances for the endoscopic endonasal transpterygoid approach to lateral sphenoid sinus encephaloceles. Neurosurg Focus. 2012. 32: E5
19. Silveira-Bertazzo G, Martinez-Perez R, Carrau RL, Prevedello DM. Surgical anatomy and nuances of the expanded transpterygoid approach to the pterygopalatine fossa and upper parapharyngeal space: A stepwise cadaveric dissection. Acta Neurochir (Wien). 2021. 163: 415-21
20. Truong HQ, Sun X, Celtikci E, Borghei-Razavi H, Wang EW, Snyderman CH. Endoscopic anterior transmaxillary “transalisphenoid” approach to Meckel’s cave and the middle cranial fossa: An anatomical study and clinical application. J Neurosurg. 2018. 130: 227-37
21. Truong HQ, Lieber S, Najera E, Alves-Belo JT, Gardner PA, Fernandez-Miranda JC. The medial wall of the cavernous sinus. Part 1: Surgical anatomy, ligaments, and surgical technique for its mobilization and/or resection. J Neurosurg. 2018. 131: 122-30
22. Wang J, Bidari S, Inoue K, Yang H, Rhoton A. Extensions of the sphenoid sinus: A new classification. Neurosurgery. 2010. 66: 797-816
23. Yasuda A, Campero A, Martins C, Rhoton AL, Ribas GC. The medial wall of the cavernous sinus: Microsurgical anatomy. Neurosurgery. 2004. 55: 179-90
24. Zhang Q, Wang Z, Guo H, Yan B, Wang Z, Zhao H. Direct Transcavernous sinus approach for endoscopic endonasal resection of intracavernous sinus tumors. World Neurosurg. 2019. 128: e478-87