- Experimental Biomedicine and Clinical Neurosciences, School of Medicine, Postgraduate Residency Program in Neurological Surgery, Neurosurgical Clinic, AOUP “Paolo Giaccone”, Palermo, Italy,
- Department of Neurosurgery, Highly Specialized Hospital and of National Importance “Garibaldi”, Catania, Italy,
- Department of Neurosurgery, Cannizzaro Hospital, Trauma Center, Gamma Knife Center, Catania, Italy.
Correspondence Address:
Gianluca Scalia, Department of Neurosurgery, Highly Specialized Hospital and of National Importance “Garibaldi,” Catania, Italy.
DOI:10.25259/SNI_784_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Salvatore Marrone1, Roberta Costanzo1, Gianluca Scalia2, Giuseppe Emmanuele Umana3, Carmelo Riolo2, Angelo Giuffrida2, Giuseppe Vasta2, Alessandro Calì2, Francesca Graziano1,2, Agatino Florio2, Giancarlo Ponzo2, Massimiliano Giuffrida2, Massimo Furnari2, Domenico Gerardo Iacopino1, Giovanni Federico Nicoletti2. Delayed brain reexpansion in schizophrenic patient affected by trabecular type chronic subdural hematoma. 06-Sep-2021;12:442
How to cite this URL: Salvatore Marrone1, Roberta Costanzo1, Gianluca Scalia2, Giuseppe Emmanuele Umana3, Carmelo Riolo2, Angelo Giuffrida2, Giuseppe Vasta2, Alessandro Calì2, Francesca Graziano1,2, Agatino Florio2, Giancarlo Ponzo2, Massimiliano Giuffrida2, Massimo Furnari2, Domenico Gerardo Iacopino1, Giovanni Federico Nicoletti2. Delayed brain reexpansion in schizophrenic patient affected by trabecular type chronic subdural hematoma. 06-Sep-2021;12:442. Available from: https://surgicalneurologyint.com/surgicalint-articles/11098/
Abstract
Background: Chronic subdural hematoma (cSDH) represents a complex and unpredictable disease, characterized by high morbidity and mortality, especially in elderly patients. Factors affecting the postoperative brain reexpansion along to cSDH recurrence have not been yet adequately investigated. The authors presented the case of a schizophrenic patient affected by trabecular type cSDH that presented a delayed brain reexpansion despite a craniotomy and membranotomy.
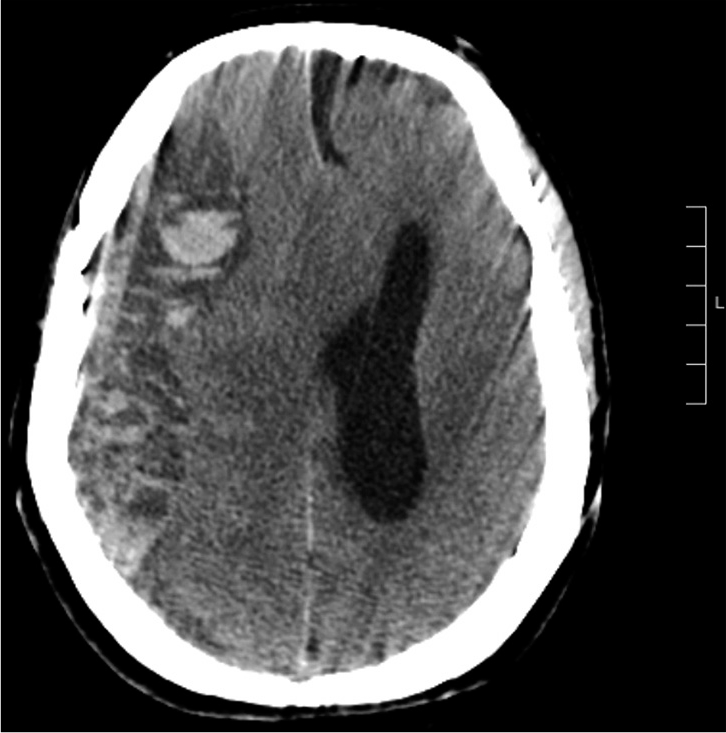
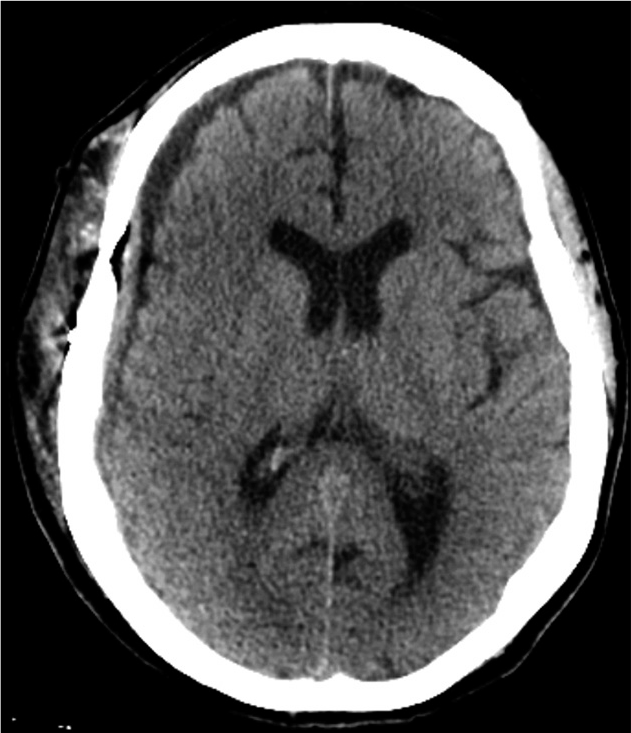
Case Description: A 51-year-old female patient with diagnosis of schizophrenia was admitted to the emergency department with GCS score of 5/15 and right anisocoria. An urgent brain CT revealed a trabecular right cSDH (35 mm in maximum diameter) with recent bleeding. After surgery, a brain CT scan showed a markedly reduced brain reexpansion and pneumocephalus. Nevertheless, postoperative 7-day brain CT documented a progressive brain reexpansion with reduced midline shift.
Conclusion: According to our opinion, anatomopathological alterations in schizophrenia reduce normal brain compliance and increasing elastance, thus modifying the normal timing of reexpansion after cSDH drainage, also after craniotomy and membranotomy. Although postoperative pneumocephalus is a well-known cause of hindered reexpansion, this could be due to anatomical alterations in schizophrenia. Such factors must be considered in the preoperative planning but mostly in the postoperative management.
Keywords: Chronic subdural hematoma, Craniotomy, Pneumocephalus, Schizophrenia, Trabecular
INTRODUCTION
Chronic subdural hematoma (cSDH) represents a complex and unpredictable disease, characterized by high morbidity and mortality, especially in elderly patients. There is no univocal indication of the cSDH treatment, and common surgical techniques include burr hole craniostomy, twist drill craniostomy, and craniotomy. Factors affecting the postoperative brain reexpansion along to cSDH recurrence have not been yet adequately investigated. In schizophrenia, micro- and macroscopic anatomopathological alterations were described, such as astrogliosis and widespread pial gliosis.[
CASE DESCRIPTION
A 51-year-old female patient with diagnosis of schizophrenia (positive symptoms) was admitted to the emergency department with GCS score of 5/15 and right anisocoria. Multiple minor self-inflicted head trauma was reported. An urgent brain CT revealed a trabecular (Nakaguchi type G) right cSDH (35 mm in maximum diameter) with recent bleeding [
DISCUSSION
A reduced compliance and an increased brain elastance are the main cause probably related to a delayed brain reexpansion. In patients with schizophrenia, anatomopathological alterations, as previously mentioned, can altered brain compliance, promoting elastance. It measures the stiffness of a system, and it is influenced by cerebrovascular volume, subpial brain tissues, and meningeal membranes.[
CONCLUSION
According to our opinion, anatomopathological alterations in schizophrenia reduce normal brain compliance and increasing elastance, thus modifying the normal timing of reexpansion after cSDH drainage, also after craniotomy and membranotomy. Although postoperative pneumocephalus is a well-known cause of hindered reexpansion, this could be due to anatomical alterations in schizophrenia. Such factors must be considered in the preoperative planning but mostly in the postoperative management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Andreasen NC, Nopoulos P, Magnotta V, Pierson R, Ziebell S, Ho BC. Progressive brain change in schizophrenia: A prospective longitudinal study of first-episode schizophrenia. Biol Psychiatry. 2011. 70: 672-9
2. Catts VS, Wong J, Fillman SG, Fung SJ, Weickert CS. Increased expression of astrocyte markers in schizophrenia: Association with neuroinflammation. Aust N Z J Psychiatry. 2014. 48: 722-34
3. Das JM, Bajaj J.editors. Pneumocephalus. Treasure Island, FL: StatPearls Publishing; 2021. p.
4. Dietz AG, Goldman SA, Nedergaard M. Glial cells in schizophrenia: A unified hypothesis. Lancet Psychiatry. 2020. 7: 272-81
5. Fischer B, Lehrl S, Weber E, Gundert-Remy U, Fischer U. Zerebrovaskuläre insuffizienzen und tabletten-compliance [Cerebrovascular insufficiency and compliance with drug therapy]. Z Gerontol. 1981. 14: 145-52
6. Freeman T, Karson CN. The neuropathology of schizophrenia. A focus on the subcortex. Psychiatr Clin North Am. 1993. 16: 281-93
7. Fukuhara T, Gotoh M, Asari S, Ohmoto T, Akioka T. The relationship between brain surface elastance and brain re-expansion after evacuation of chronic subdural hematoma. Surg Neurol. 1996. 45: 570-4
8. Huang BY, Castillo M. Hypoxic-ischemic brain injury: Imaging findings from birth to adulthood. Radiographics. 2008. 28: 417-39
9. Kayaci S, Kanat A, Koksal V, Ozdemir B. Effect of inner membrane tearing in the treatment of adult chronic subdural hematoma: A comparative study. Neurol Med Chir (Tokyo). 2014. 54: 363-73
10. Kazakova PB. Fibrosis of the pia mater in schizophrenia. Zh Nevropatol Psikhiatr Im S S Korsakova. 1961. 61: 1244-50
11. Montano N, Stifano V, Skrap B, Mazzucchi E. Management of residual subdural hematoma after burr-hole evacuation. The role of fluid therapy and review of the literature. J Clin Neurosci. 2017. 46: 26-9
12. Van Erp TG, Walton E, Hibar DP, Schmaal L, Jiang W, Glahn DC. Cortical brain abnormalities in 4474 individuals with schizophrenia and 5098 control subjects via the enhancing neuro imaging genetics through meta-analysis (ENIGMA) consortium. Biol Psychiatry. 2018. 84: 644-54
13. Walsh EK, Schettini A, Hoff JT, Betz AL.editors. Brain tissue elasticity and CSF elastance. Intracranial Pressure VII. Berlin, Heidelberg: Springer; 1989. p.
14. Yoshida R, Otomo E, Sugino M, Takenaka H. Cerebral atrophy of senile dementia. Rinsho Shinkeigaku. 1987. 27: 911-7







Dr. Miguel A. Faria
Posted September 6, 2021, 10:31 am
This is a good article that among many other concepts, reminds us that pathological problems in neurosurgery and the procedures required to correct them, can affect schizophrenic patients in unexpected ways, not only mentally but also anatomically, for reasons not yet completely elucidated.