- Department of Neurosurgery, University Hospital of Patras, Patras, Greece.
- Department of Anesthesiology and ICU, University Hospital of Patras, Patras, Greece.
- Department of Otorhinolaryngology, Head and Neck Surgery, University Hospital of Patras, Patras, Greece.
Correspondence Address:
Dionysia Fermeli, Department of Neurosurgery, University Hospital of Patras, Patras, Greece.
DOI:10.25259/SNI_980_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Dimitrios Papadakos1, Dionysia Fermeli1, Panagiotis Tsipouriaris1, Theofanis Vrettos2, Nikolaos Mastronikolis3, Constantine Constantoyannis1. Delayed postoperative erosion of hypopharynx after anterior hardware extrusion: A case report. 16-Feb-2024;15:47
How to cite this URL: Dimitrios Papadakos1, Dionysia Fermeli1, Panagiotis Tsipouriaris1, Theofanis Vrettos2, Nikolaos Mastronikolis3, Constantine Constantoyannis1. Delayed postoperative erosion of hypopharynx after anterior hardware extrusion: A case report. 16-Feb-2024;15:47. Available from: https://surgicalneurologyint.com/surgicalint-articles/12755/
Abstract
Background: Esophageal breach or pharynx perforations are serious and potentially fatal complications of anterior cervical corpectomy/fusion (ACF). They are either recognized intraoperatively or are diagnosed within several postoperative days. Here, a 76-year-old male presented with the retropharyngeal extrusion of an anterior cervical expandable cage that occurred two years postoperatively.
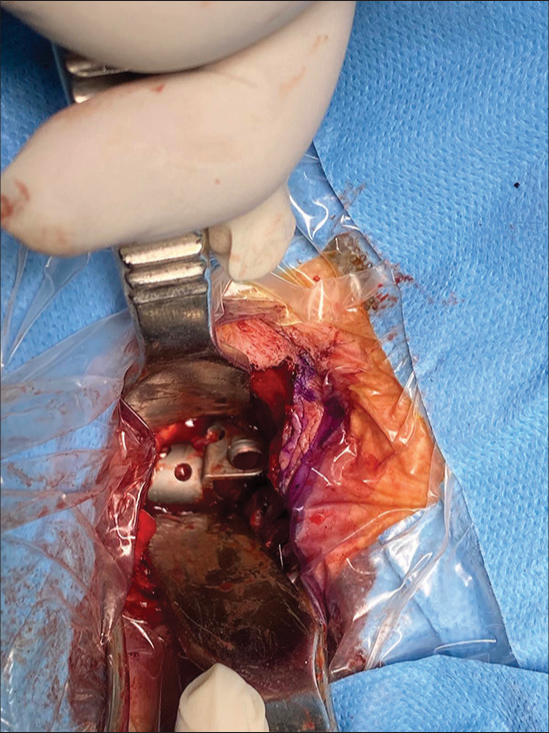
Case Description: A 76-year-old male with a history of an anterior corpectomy/fusion (C3–C6, corpectomy C4, C5) performed two years ago presented with persistent dysphagia for three months. Cervical X-rays showed anterior migration of the expandable cage and that was also confirmed by computed tomography (CT) scans. During intubation, the anesthesiologist observed that the cage had directly penetrated the hypopharynx. Following routine removal of the cage, ENT could not identify (using the operating microscope) any direct perforation of the esophagus or hypopharynx; presumably, the esophageal breach was small, and the esophageal wall spontaneously closed the gap following cage excision.
Conclusion: Pharyngeal perforation after ACF is typically associated with significant morbidity and mortality. Stringent preoperative assessment, utilizing X-rays, magnetic resonance/CT studies, and ENT specialists to perform indirect laryngoscopy, may optimize postoperative outcomes.
Keywords: anterior cervical corpectomy/fusion (ACF), Cage migration, Esophageal perforation, Pharynx erosion
INTRODUCTION
Anterior cervical corpectomy and fusion (ACF C3–C6 with C4, C5, corpectomy) may rarely result in esophageal breaches, hypopharynx perforations, trachea injuries, carotid ruptures, and/or recurrent laryngeal nerve damage.[
CASE DESCRIPTION
Preoperative evaluation
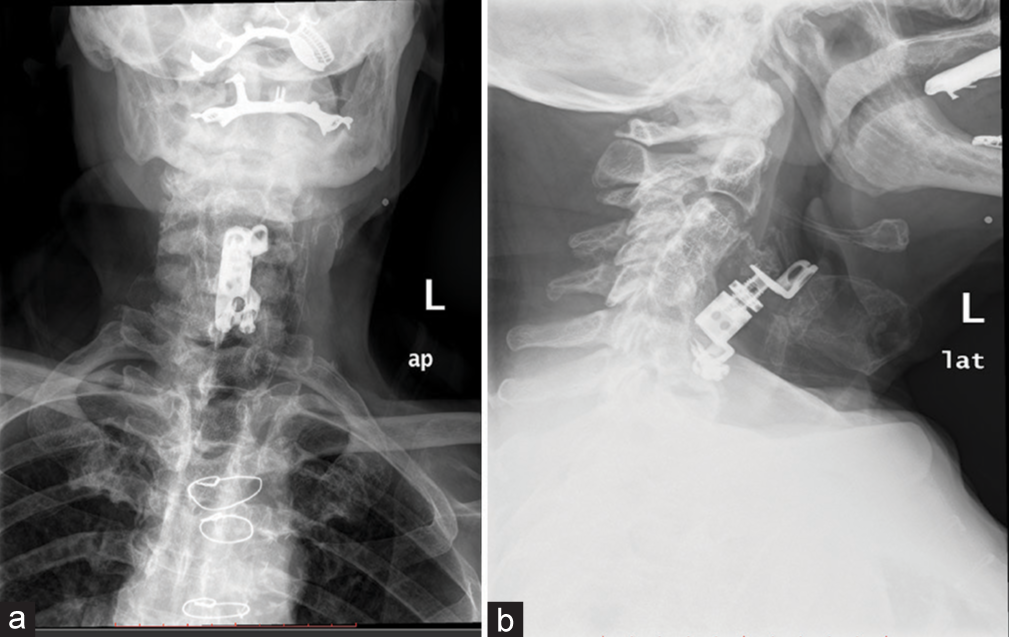
A 76-year-old male with a history of a C3–C6 ACF 2 years ago presented with dysphagia for three months. Cervical X-rays showed anterior migration of the expandable cage [
Surgery
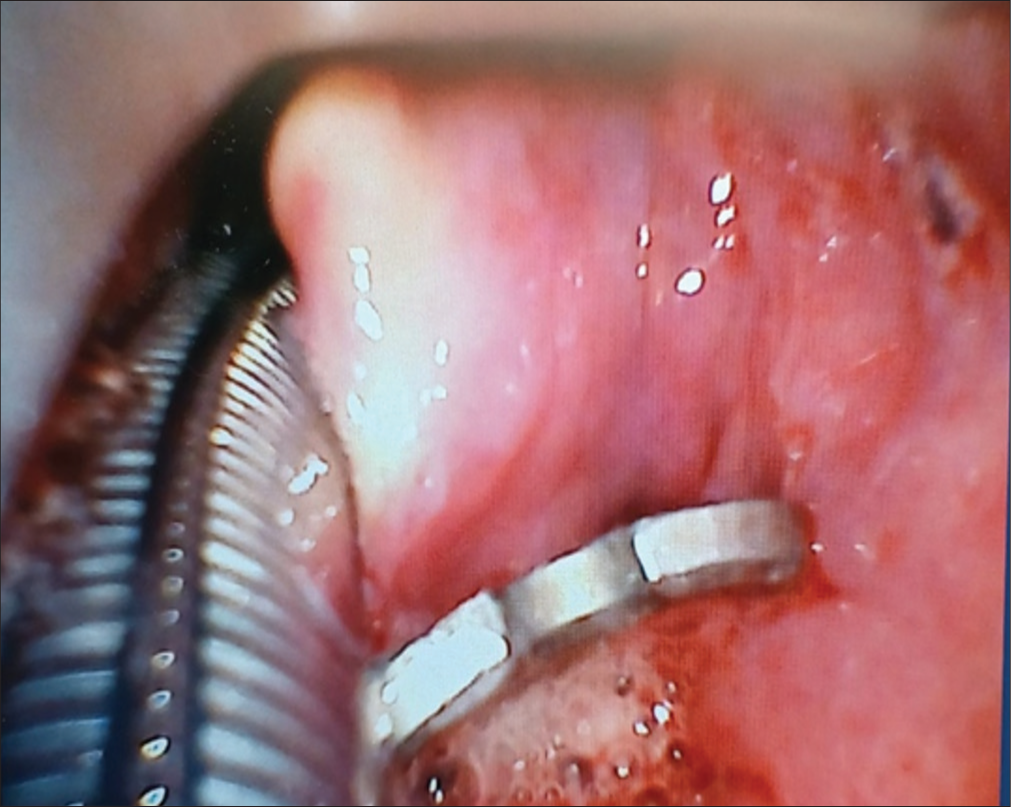
During the intubation, the anesthesiologist directly visualized the expandable cage within the esophaguahypopharynx [
Postoperative course
Postoperatively, a nasogastric tube was maintained just in case an esophageal perforation had been missed; this would reduce the potential for developing mediastinitis. On the third postoperative day, the patient developed chest pain, difficulty in breathing, and tachypnea. The emergency chest CT scan documented no mediastinitis, but the electrocardiogram/cardiac workup was diagnostic for myocardial infarction. After a three days stay in the cardiac intensive care unit, he returned to the neurosurgical floor.
Further ENT evaluation
On the 11th postoperative day, ENT performed another laryngoscopy; this was negative. The barium swallow that followed was also normal. The patient was maintained on antibiotics for 14 days in total and ultimately discharged on the 15th postoperative day, fully recovered and without dysphagia.
DISCUSSION
Incidence of pharyngoesophageal erosion/perforation
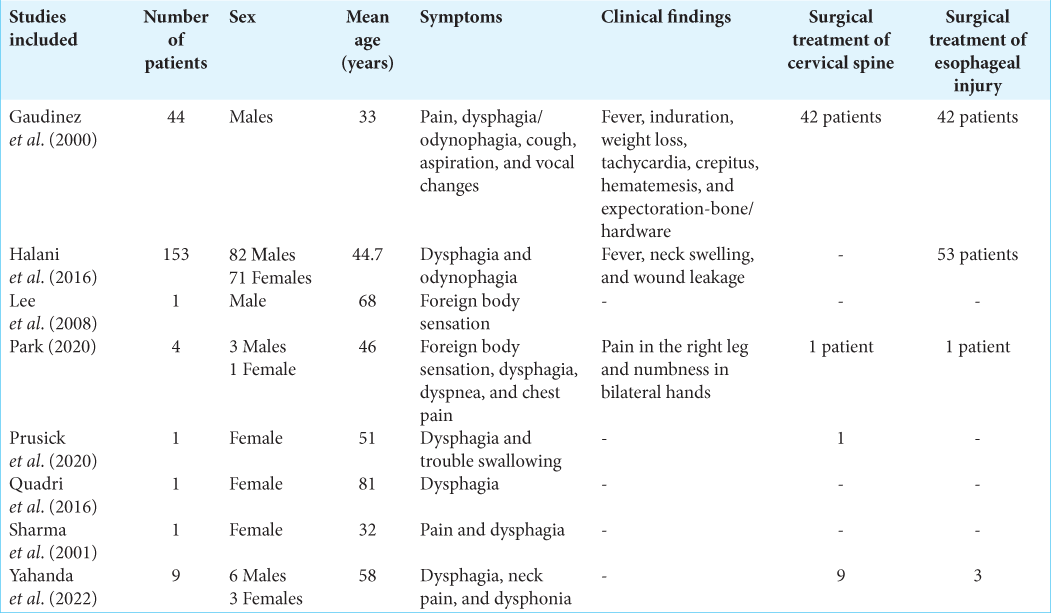
Pharyngoesophageal erosion is an uncommon complication of anterior cervical surgery. Retrospective study of 2946 patients (Gaudinez et al.)[
Mechanism of pharyngoesophageal erosion/perforation
Multiple mechanisms may lead to pharyngoesophageal perforations and include chronic compression by hardware, pressure sores caused by the titanium implant/cages, and microtrauma of the outer surface of the pharynx.[
Diagnosis of pharyngoesophageal erosion/perforation
The diagnosis of pharyngoesophageal erosion/perforation is readily achieved utilizing endoscopy or a Barium swallow-esophagogram. Furthermore, useful in documenting anterior migration/extrusion of instrumentation are X-rays and a contrast CT scan of the neck/chest (i.e., showing air in the mediastinum, a paravertebral collection, and/or mediastinitis).
Surgery pharyngoesophageal erosion/perforation
Although conservative treatment is described in the literature, surgery is the treatment of choice to address pharyngoesophageal erosion/perforation.[
CONCLUSION
Pharyngeal perforation after ACF carries significant morbidity and up to a 4% mortality. The preoperative assessment for a patient presenting with significant dysphagia following ACF should include X-rays, magnetic resonance, and CT studies, along with laryngoscopy by ENT to look for an esophageal/hypopharynx perforation directly.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Gaudinez RF, English GM, Gebhard JS, Brugman JL, Donaldson DH, Brown CW. Esophageal perforations after anterior cervical surgery. J Spinal Disord. 2000. 13: 77-84
2. Halani SH, Baum GR, Riley JP, Pradilla G, Refai D, Rodts GE. Esophageal perforation after anterior cervical spine surgery: A systematic review of the literature. J Neurosurg. 2016. 25: 285-91
3. Lee JS, Kang DH, Hwang SH, Han JW. Oral extrusion of screw after anterior cervical interbody fusion. J Korean Neurosurg Soc. 2008. 44: 259-61
4. Park JS. Esophageal perforation associated with anterior cervical discectomy and fusion. Case series and a review of the literature. Interdiscip Neurosurg. 2020. 22: 100867
5. Prusick PJ, Sabri SA, Kleck CJ. Expectoration of anterior cervical discectomy and fusion cage: A case report. J Spine Surg. 2021. 7: 218-24
6. Quadri SA, Capua J, Ramakrishnan V, Sweiss R, Cabanne M, Noel J. A rare case of pharyngeal perforation and expectoration of an entire anterior cervical fixation construct. J Neurosurg. 2017. 26: 560-6
7. Sharma RR, Sethu AU, Lad SD, Turel KE, Pawar SJ. Pharyngeal perforation and spontaneous extrusion of the cervical graft with its fixation device: A late complication of C2-C3 fusion via anterior approach. J Clin Neurosci. 2001. 8: 464-8
8. Yahanda AT, Pennicooke B, Ray WZ, Hacker CD, Kelly MP, Dorward IG. Pharyngoesophageal damage from hardware extrusion at an average of 7.5 years after anterior cervical diskectomy and fusion: A case series, discussion of risk factors, and guide for management. World Neurosurg. 2022. 160: e189-98
9. Yee TJ, Swong K, Park P. Complications of anterior cervical spine surgery: A systematic review of the literature. J Spine Surg. 2020. 6: 302-22