- Department of Neurology, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, United States.
- Department of Neurological Surgery, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, United States.
- Department of Orthopedic Surgery, Baylor University Medical Center, Houston, Texas, United States.
Correspondence Address:
Daniel Y. Chu, Department of Neurology, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, United States.
DOI:10.25259/SNI_1046_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Daniel Y. Chu1, Garret P. Greeneway2, Cody J. Falls3, Paul S. Page2, Azam S. Ahmed2. Delayed spinal epidural hematoma following T1 chance fracture: An illustrative case and review of the literature. 23-Dec-2022;13:593
How to cite this URL: Daniel Y. Chu1, Garret P. Greeneway2, Cody J. Falls3, Paul S. Page2, Azam S. Ahmed2. Delayed spinal epidural hematoma following T1 chance fracture: An illustrative case and review of the literature. 23-Dec-2022;13:593. Available from: https://surgicalneurologyint.com/surgicalint-articles/12070/
Abstract
Background: A Chance fracture is a traumatic fracture of the thoracic or lumbar spine that occurs secondary to a flexion-distraction injury. Although patients with chance fractures rarely present with neurologic deficits, a subset may become symptomatic from spinal epidural hematomas (SEH) warranting emergent decompressive surgery.
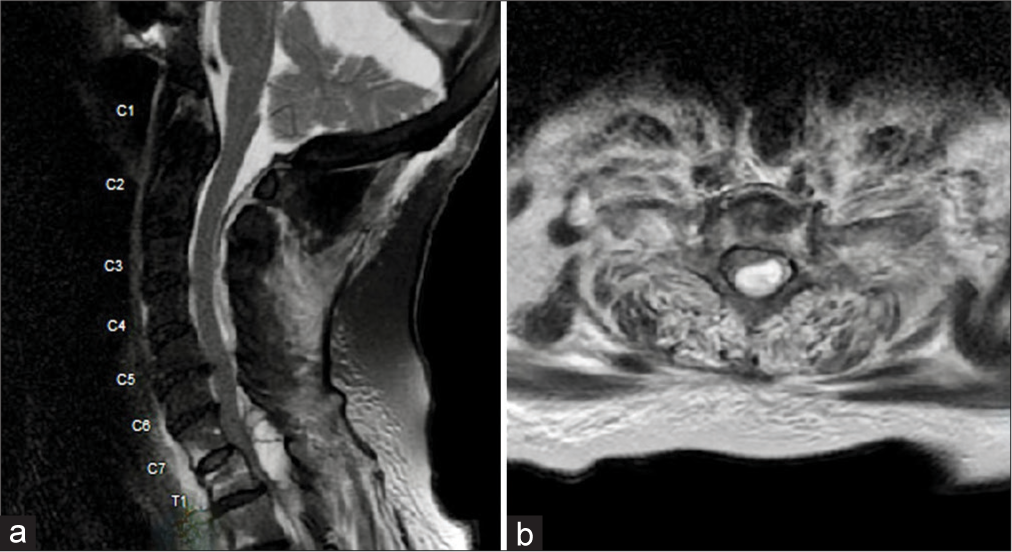
Case Description: An 87-year-old female on anticoagulation presented with a T1 Chance fracture after a fall. She was originally neurologically intact, but became paraplegic over the next 10 h. When the cervical/thoracic magnetic resonance revealed a SEH markedly compressing the cord between the C7-T1 levels, she underwent an emergent decompression; she also had a C5-T4 instrumented fusion. Postoperatively, she regained lower limb function, but expired on postoperative day 5 due to respiratory complications likely attributed to the prolonged surgery for the spinal instrumentation.
Conclusion: Delayed SEH rarely occur following spinal Chance fractures. Here, an 87-year-old female on anticoagulation developed the 10-h delayed onset of a SEH with paraplegia attributed to a T1 Chance fracture at the C7-T1 level. Although she regained neurological function following the emergent decompression, she expired 5 days later likely due to the extended operative time/blood loss from the C5-T4 fusion that could have been avoided.
Keywords: Anticoagulation, Chance fracture, Epidural hematoma, Spine fracture, Thoracic spine
INTRODUCTION
A Chance fracture is a traumatic horizontal fracture of the spine that occurs secondary to a flexion/distraction injury.[
ILLUSTRATIVE CASE
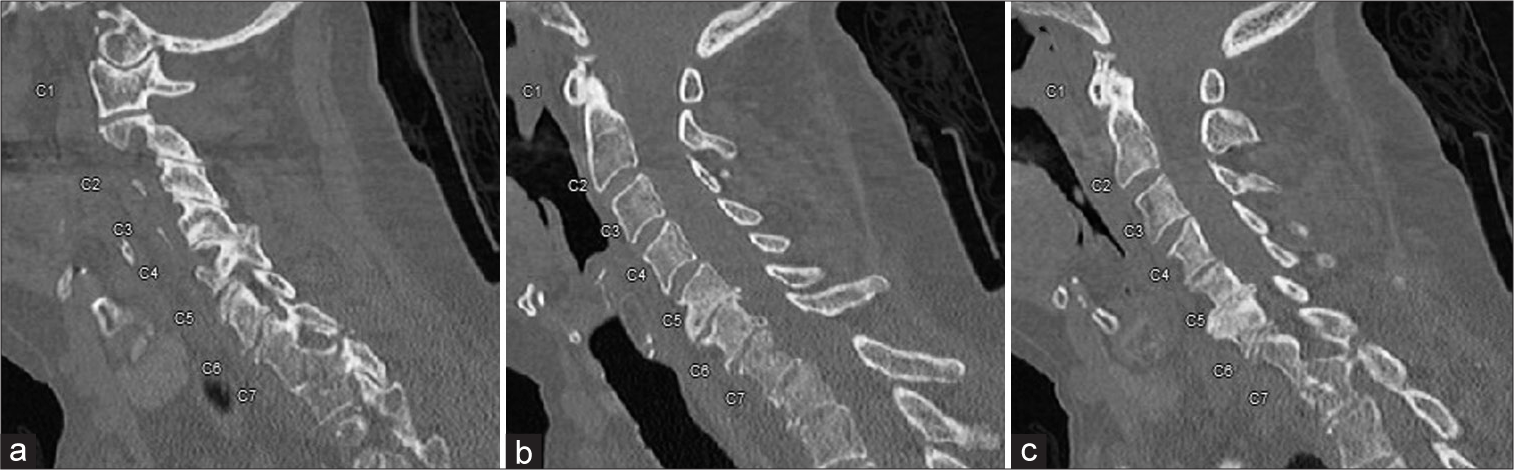
Following a fall at home, an 87-year-old female on Warfarin for coronary artery disease and atrial fibrillation, presented with neck pain but was neurologically intact. Lab studies showed international normalized ratio (INR) of 4.6 and a hemoglobin of 6.6 g/dL; she received one unit of packed red blood cells, 10 mg of vitamin K, and 6 mg of intravenous dexamethasone. The cervical computed tomography showed an acute flexion-distraction injury (Chance fracture) of T1 with kyphosis [
DISCUSSION
Observations
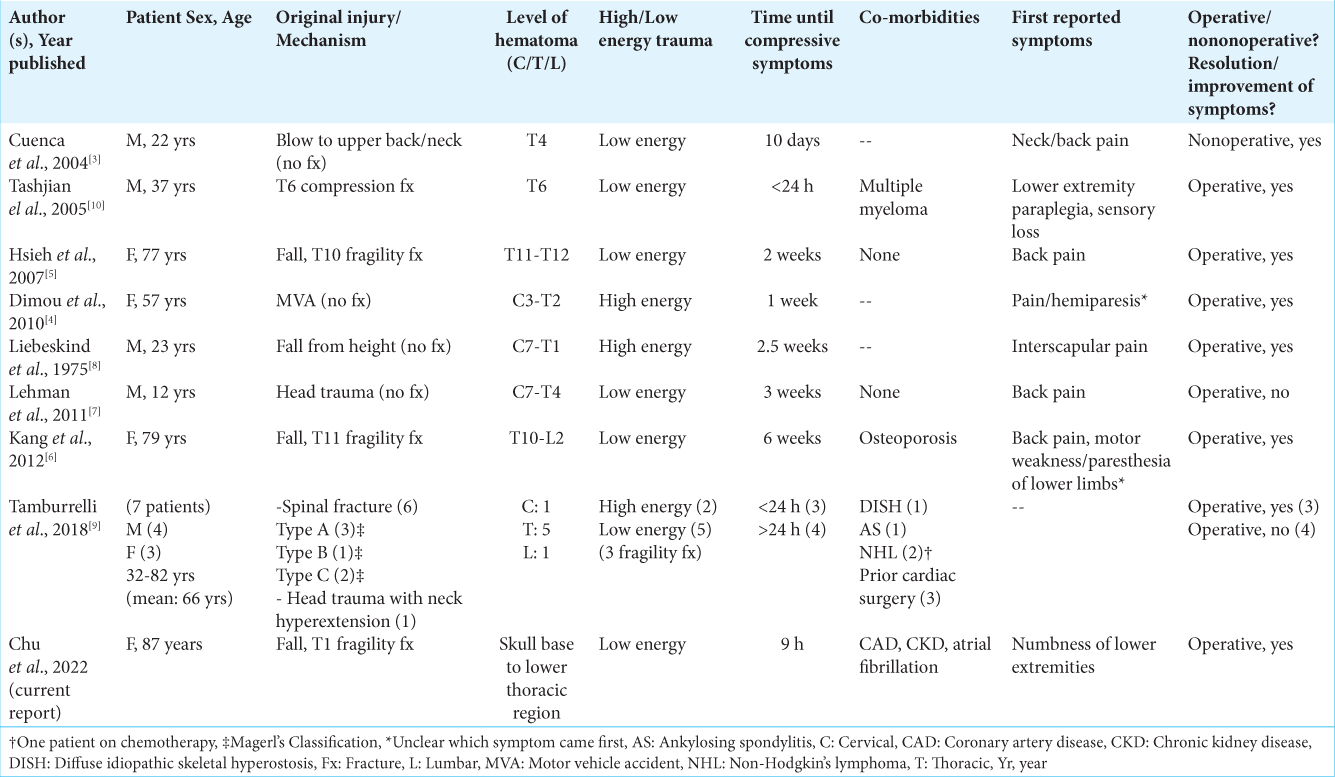
Chance fractures are traumatic fractures of the thoracic or lumbar spine that occur through flexion-distraction forces that are rarely associated with the delayed onset of SEH. A review of delayed (i.e., 8 h after injury) SEH following traumatic back injuries [
Etiology of SEH with chance fractures
SSEH with Chance spinal fractures most likely occur secondary to trauma to the thin-walled epidural venous plexus, and are less likely to be attributed to epidural plexus arteriovenous malformation, hemangiomas, and spinal tumors.[
Factors to reconsider in this case
Patients with SEH due to chance fractures may warrant decompressive laminectomies alone without fusions. Certainly, in this case, the dorsally located C7-T1 epidural hematoma could have been effectively removed/decompressed within a matter of 1–2 h. The patient should likely not have initially undergone the additional instrumented C5-T4 posterolateral fusion. In short, avoiding the emergent longer- duration posterolateral C5-T4 fusion would have markedly reduced the operative time, and likely avoided the patient’s subsequent respiratory decompensation, and death.
CONCLUSION
Delayed SEH following Chance spinal fractures are rare. Here, we presented an 87-year-old female who 10 h following a C7-T1 Chance Fracture developed a SEH warranting emergent laminectomy, but likely not the instrumented fusion that contributed to her demise.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
NIH T32 GM140935.
Conflicts of interest
There are no conflicts of interest
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Al-Mutair A, Bednar DA. Spinal epidural hematoma. J Am Acad Orthop Surg. 2010. 18: 494-502
2. Chance GQ. Note on a type of flexion fracture of the spine. Br J Radiol. 1948. 21: 452
3. Cuenca PJ, Tulley EB, Devita D, Stone A. Delayed traumatic spinal epidural hematoma with spontaneous resolution of symptoms. J Emerg Med. 2004. 27: 37-41
4. Dimou J, Jithoo R, Bush S. A patient with delayed traumatic cervical spinal epidural haematoma presenting with hemiparesis. J Clin Neurosci. 2010. 17: 404-5
5. Hsieh CT, Chiang YH, Tang CT, Sun JM, Ju DT. Delayed traumatic thoracic spinal epidural hematoma: A case report and literature review. Am J Emerg Med. 2007. 25: 69-71
6. Kang MS, Shin YH, Lee CD, Lee SH. Delayed neurological deficits induced by an epidural hematoma associated with a thoracic osteoporotic compression fracture. Neurol Med Chir (Tokyo). 2012. 52: 633-6
7. Lehman AA, McKenna ME, Wisneski R, Hess WF. Delayed presentation of a traumatic spinal epidural hematoma in a preadolescent: A case report. J Bone Joint Surg Am. 2011. 93: e28
8. Liebeskind A, Schwartz K, Coffey E, Beresford H. Spinal epidural hematoma with delayed appearance of neurological symptoms. Neuroradiology. 1975. 8: 191-3
9. Tamburrelli FC, Meluzio MC, Masci G, Perna A, Burrofato A, Proietti L. Etiopathogenesis of traumatic spinal epidural hematoma. Neurospine. 2018. 15: 101-7
10. Tashjian RZ, Bradley MP, Lucas PR. Spinal epidural hematoma after a pathologic compression fracture: An unusual presentation of multiple myeloma. Spine J. 2005. 5: 454-6