- Department of Neurological Surgery, College of Medicine, The Ohio State University,Columbus, United States.
- Department of Neurological Surgery, The Ohio State University Wexner Medical Center, Columbus, United States.
Correspondence Address:
David Gibbs, Department of Neurological Surgery, College of Medicine, The Ohio State University, Columbus, United States.
DOI:10.25259/SNI_375_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: David Gibbs1, Andrew James Grossbach2, Noah Mallory1, Nathaniel Toop2, Stephanus Viljoen2. Delayed stenosis associated with sublaminar band placement in the thoracic spine for proximal junctional kyphosis. 16-Jun-2023;14:211
How to cite this URL: David Gibbs1, Andrew James Grossbach2, Noah Mallory1, Nathaniel Toop2, Stephanus Viljoen2. Delayed stenosis associated with sublaminar band placement in the thoracic spine for proximal junctional kyphosis. 16-Jun-2023;14:211. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12361
Abstract
Background: Proximal junctional thoracic kyphosis (PJK) is common following adult spinal deformity (ASD) surgery and may require revision operations. In this case series, we present delayed complications associated with the use of sublaminar banding (SLBs) for PJK prophylaxis.
Case Description: Three patients underwent long-segment thoracolumbar decompression and fusions for ASD. All had undergone SLB placement for PJK prophylaxis. All three subsequently developed neurologic complications secondary to cephalad spinal cord compression/stenosis requiring urgent revision surgery.
Conclusion: The placement of SLBs placed to prevent PJK may lead to sublaminar inflammation contributing to severe cephalad spinal canal stenosis and myelopathy following ASD surgery. Surgeons should be aware of this potential complication and may consider alternatives to SLB placement to avoid this complication.
Keywords: Arthrodesis, Myelopathy, Proximal junctional failure, Proximal junctional kyphosis, Sublaminar bands
INTRODUCTION
PJK is a common complication following corrective surgery for adult spinal deformity (ASD). PJK, radiographically defined as an increase in the sagittal Cobb angle to ≥10° or at least a 10° increase in the segmental kyphosis, affects up to 45% of all patients with 60% becoming symptomatic within 3 postoperative months.[
To reduce/prevent PJK, sublaminar bands (SLBs) were introduced to expand the transition zone between the instrumented and noninstrumented proximal junctional levels following long-segment thoracolumbar constructs.[
CASE SERIES
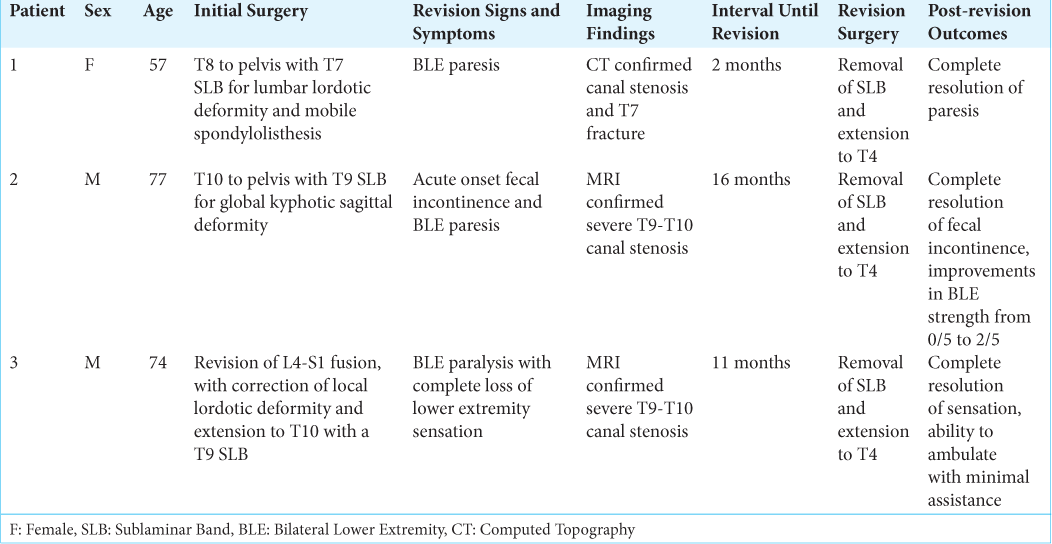
Three patients with ASD averaged 69.3 years of age and underwent long-segment thoracolumbar surgical decompressions and fusions utilizing in-line proximal SLB connectors.[
Patient #1
Our first patient, a 57-year-old female with a history of multiple spine surgeries and a spinal cord stimulator had preoperative imaging that demonstrated a local lumbar lordotic deformity with a pelvic incidence-lumbar lordosis (PI-LL) mismatch of −14° and a C7 sagittal vertical axis (SVA) of 92.3 mm. Further, there was pseudoarthrosis with a mobile spondylolisthesis at L4-5 with neural foraminal stenosis bilaterally at L2-L3 and L5-S1. She underwent T8 to pelvis fusion with a T7 SLB. Two months later, she acutely presented to the emergency department with sudden onset bilateral lower extremity paraparesis. CT showed thoracic canal stenosis and a fracture at T7, the level of the SLBs. Revision with removal of the SLB and extension of her construct to T4 was performed and she improved postoperatively.
Patient #2
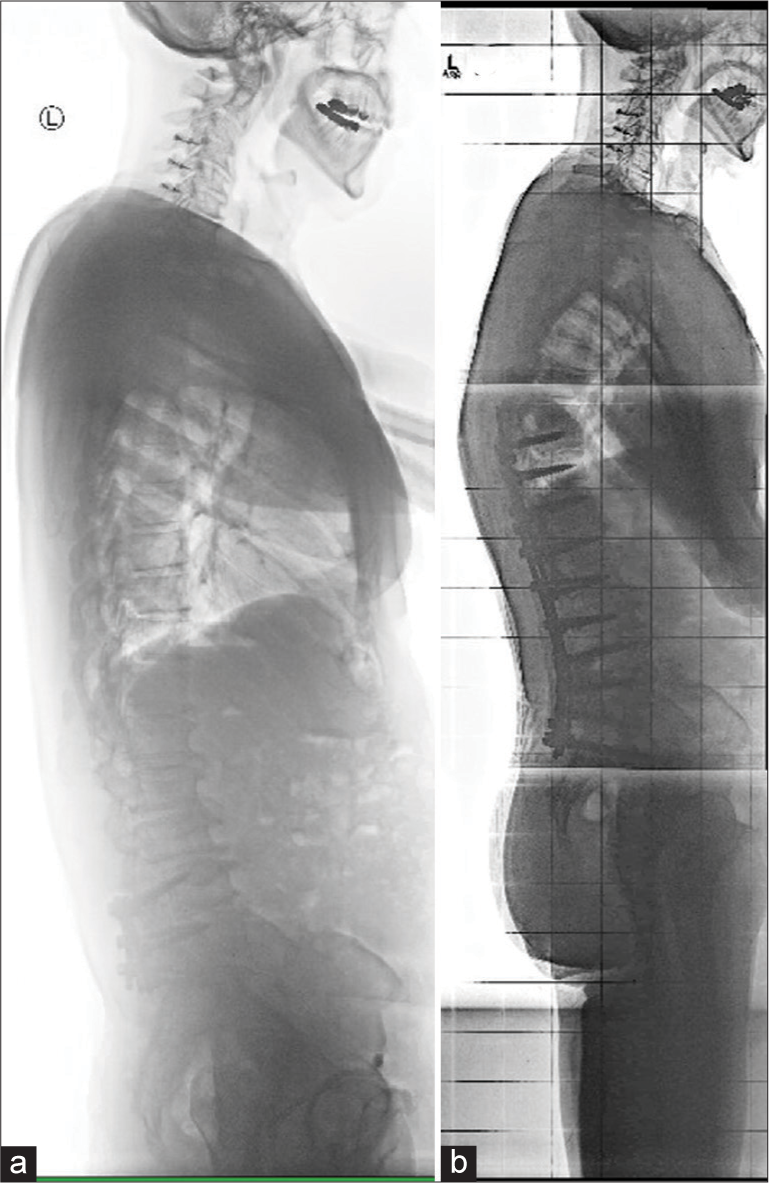
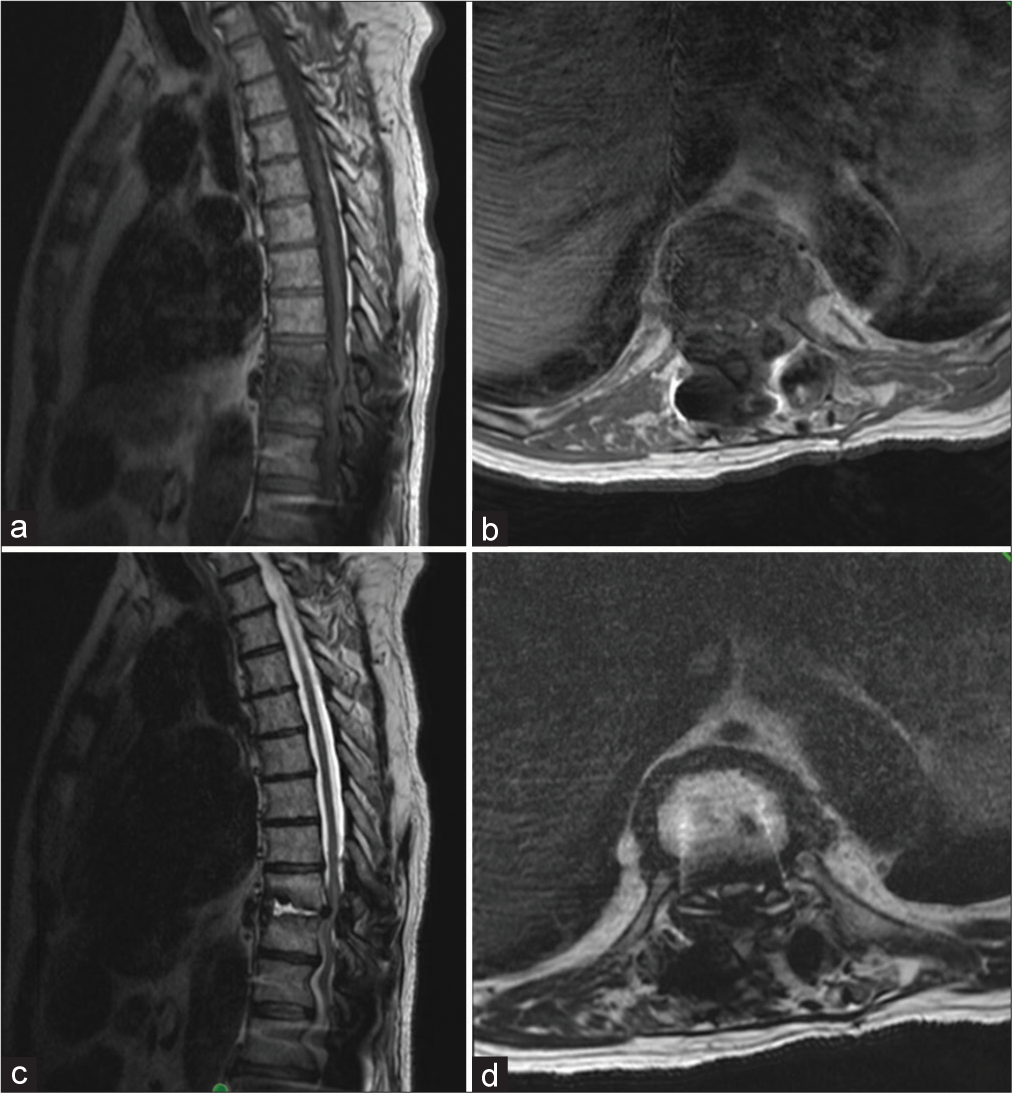
Our second patient, a 77-year-old male, initially presented with worsening low back and right leg pain. Imaging demonstrated global kyphotic sagittal deformity with a PI-LL mismatch of 18° and a C7 SVA of 10.2 mm [
Patient #3
Our third patient, a 74-year-old male presented with intractable back and leg pain requiring revision of his prior L4-S1 construction. X-ray imaging demonstrated a local lordotic sagittal deformity with a PI-LL mismatch of 13° and C7 SVA -27.6 mm. He underwent revision and extension to T10 with a T9 SLB. Eleven months later, he presented to the ED paralyzed and insensate in both of his lower extremities. The MRI revealed severe T9-T10 canal stenosis that prompted urgent revision and extension to T4 with removal of his T9 SLB. Postoperatively, he was able to ambulate with minimal assistance and had completely recovered sensation.
DISCUSSION
Here, we presented three patients who had SLBs placed one level above the proximal end of long-segment thoracolumbar constructs (decompressions/fusions) to mitigate the risk of PJK/PJF. All three developed acute postoperative myelopathies due to SLB-related significant inflammation and tissue hypertrophy resulting in severe spinal cord compression. At revision surgery, the vertebrae where the SLBs were placed formed what appeared to be “Charcot-Joint” like tissue hypertrophy. While the in vivo characteristics of SLBs remain unstudied, we hypothesize that micromotion against the band within the sublaminar joint space may lead to chronic inflammation and the subsequent development of the observed canal stenosis and myelopathy. Viswanathan et al. were the first to prospectively assess the potential role for SLBs in preventing PJK/PJF at 1 year among 40 ASD patients.[
CONCLUSION
SLBs may be effective in preventing PJK/PJF following extensive thoracolumbar fusions, but their long-term safety, as documented in the three patients presented above, remains questionable.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Echt M, Ranson W, Steinberger J, Yassari R, Cho SK. A systematic review of treatment strategies for the prevention of junctional complications after long-segment fusions in the osteoporotic spine. Glob Spine J. 2021. 11: 792-801
2. Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: Incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976). 2005. 30: 1643-9
3. Hyun SJ, Lee BH, Park JH, Kim KJ, Jahng TA, Kim HJ. Proximal junctional kyphosis and proximal junctional failure following adult spinal deformity surgery. Korean J Spine. 2017. 14: 126-32
4. Kim HJ, Iyer S. Proximal junctional kyphosis. J Am Acad Orthop Surg. 2016. 24: 318-26
5. Safaee MM, Dalle Ore CL, Zygourakis CC, Deviren V, Ames CP. The unreimbursed costs of preventing revision surgery in adult spinal deformity: Analysis of cost-effectiveness of proximal junctional failure prevention with ligament augmentation. Neurosurg Focus. 2018. 44: E13
6. Smith JS, Shaffrey CI, Ames CP, Lenke LG. Treatment of adult thoracolumbar spinal deformity: Past, present, and future. J Neurosurg Spine. 2019. 30: 551-67
7. Viswanathan VK, Kukreja S, Minnema AJ, Farhadi HF. Prospective assessment of the safety and early outcomes of sublaminar band placement for the prevention of proximal junctional kyphosis. J Neurosurg Spine. 2018. 28: 520-31
8. Viswanathan VK, Minnema AJ, Viljoen S, Farhadi HF. Sublaminar banding as an adjunct to pedicle screw-rod constructs: A review and technical note on novel hybrid constructs in spinal deformity surgery. J Neurosurg Spine. 2019. 30: 807-13