- Spinal Disorders Center, Fujieda Heisei Memorial Hospital, Mizukami, Fujieda, Japan.
Correspondence Address:
Shu Takeuchi, Spinal Disorders Center, Fujieda Heisei Memorial Hospital, Mizukami, Fujieda, Japan.
DOI:10.25259/SNI_626_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shu Takeuchi, Junya Hanakita, Toshiyuki Takahashi, Manabu Minami, Ryo Kanematsu, Izumi Suda, Sho Nakamura. Destructive spondylodiscitis associated with SAPHO syndrome: A case report and literature review. 05-Aug-2022;13:345
How to cite this URL: Shu Takeuchi, Junya Hanakita, Toshiyuki Takahashi, Manabu Minami, Ryo Kanematsu, Izumi Suda, Sho Nakamura. Destructive spondylodiscitis associated with SAPHO syndrome: A case report and literature review. 05-Aug-2022;13:345. Available from: https://surgicalneurologyint.com/surgicalint-articles/11761/
Abstract
Background: Synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome is a rare sterile inflammatory disease characterized by cutaneous and osteoarticular lesions. Associated spinal lesions chronically manifest slight or no neurological symptoms. Only rarely does destructive spondylodiscitis occur.
Case Description: A 62-year-old female with palmoplantar pustulosis presented with a rapidly progressive quadriparesis. When the cervical MR showed destructive spondylodiscitis at the C5–C7 level, the patient underwent anterior debridement followed by posterior reconstruction/fixation. The histopathology showed a nonspecific inflammatory process with vertebral sclerosis consistent with the diagnosis of SAPHO; cultures were negative. Postoperatively, the patient’s symptoms improved and SAPHO did not recur.
Conclusion: Destructive spondylodiscitis associated with SAPHO syndrome is uncommon. Early diagnosis and surgical treatment result in the best outcomes.
Keywords: Destructive spondylodiscitis, SAPHO syndrome, Spine surgery
INTRODUCTION
Synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome, a noninfectious inflammatory disease, can rarely cause destructive spondylodiscitis.[
CASE DESCRIPTION
History and examination
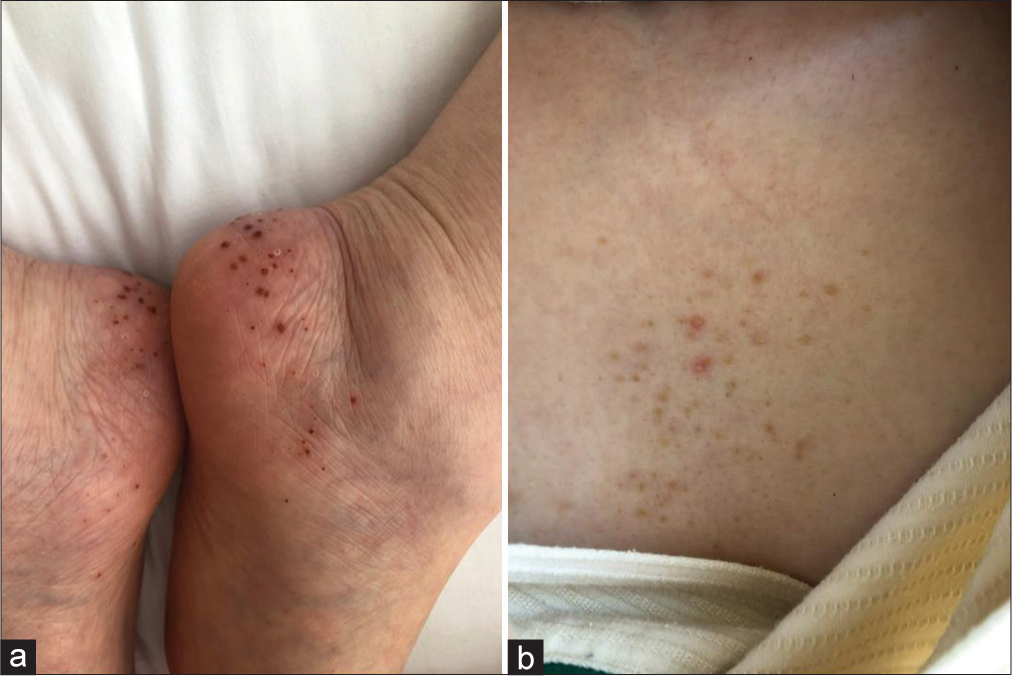
A 62-year-old female presented with progressive shoulder pain and quadriparesis that worsened over a 6 day course in the hospital. On physical examination, she had evidence of the SAPHO syndrome characterized by synovitis, acne, pustulosis, hyperostosis, osteitis, palmoplantar pustulosis, and acne on anterior chest wall [
Diagnostic work-up
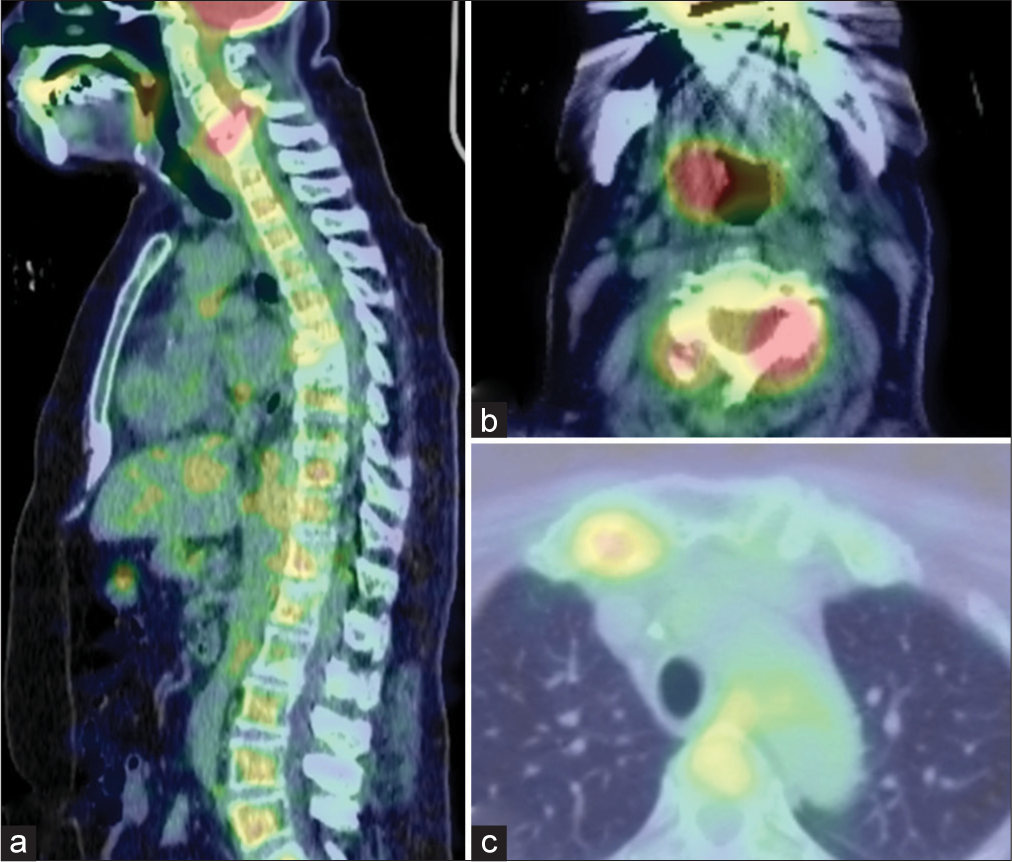
Plain cervical X-rays showed destruction of the C5–C7 vertebral bodies with kyphosis [
Figure 2:
Preoperative images. (a) Cervical plain radiography shows kyphotic deformity of C5–C7 vertebral bodies. (b) Sagittal CT scan demonstrates remarkable destructive change at C6 vertebra. (c and d) Midsagittal MRI of cervical spine shows highly tortuous spinal cord and compressed vertebrae of C5, 6 with T1 hypointense signal, T2 iso-hyperintense signal.
Circumferential C5–C7 Surgery
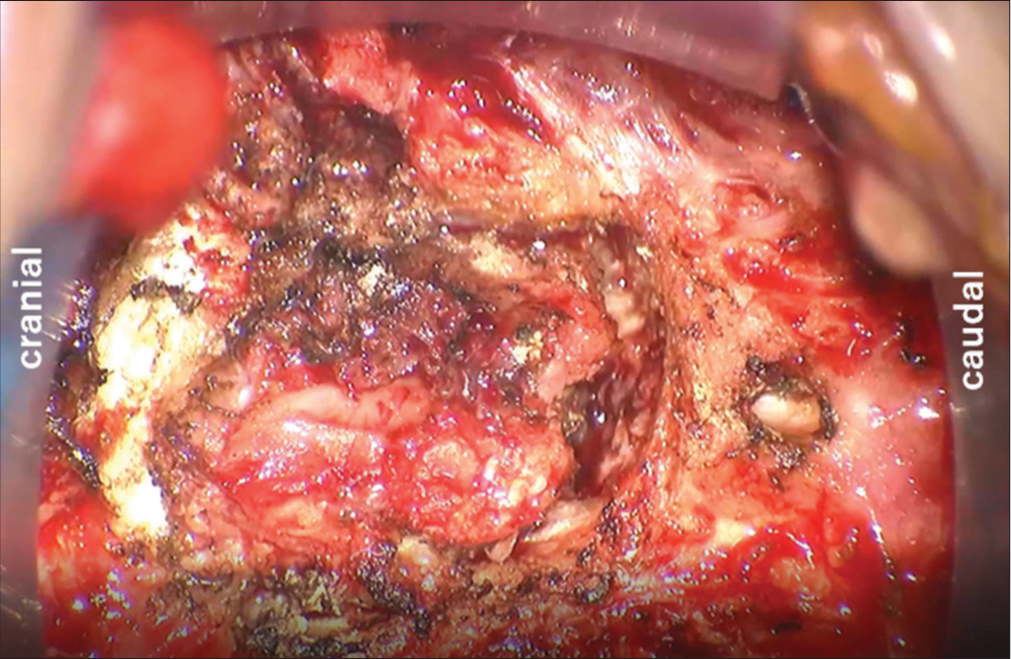
She underwent an anterior C5, C6 corpectomies with C4–C7 fusion (i.e., using iliac crest autograft and a plate) under microscopic visualization. Erosive granulomatous tissue was removed, but no abscess or solid tumor were encountered [
Histological diagnosis
The histopathological examination was consistent with SAPHO syndrome. The findings included a sterile inflammatory infiltrate composed of neutrophils and lymphocytes. Within the C5 and C6 vertebral bodies, bony trabeculae and sclerotic changes were observed.
Postoperative course
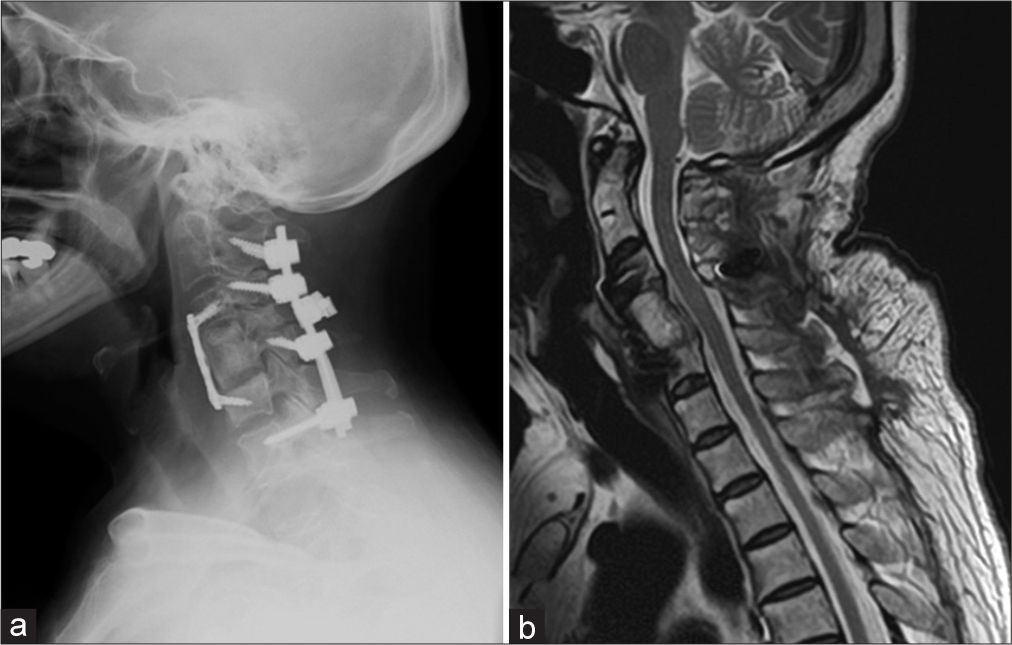
Postoperatively, her quadriparesis immediately resolved and imaging studies demonstrated decompression of spinal cord with correction of the kyphosis [
DISCUSSION
SAPHO syndrome is rare nonbacterial inflammatory disease, characterized by cutaneous and osteoarticular lesions, occurring in 1/10,000 in Europe but only in 0.000285/10,000 in Japan.[
Literature review
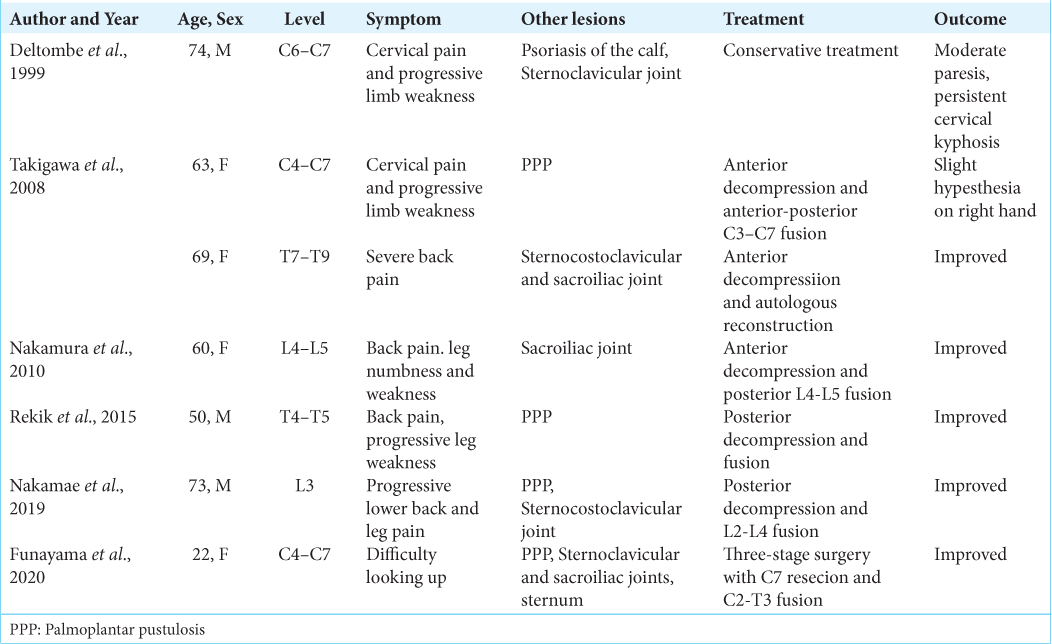
From the literature, we identified seven cases of SAPHO syndrome accompanied by destructive spondylodiscitis and neurological deficits [
CONCLUSION
Although SAPHO syndrome is usually chronic, those who rarely develop spinal spondylodiscitis may present with acute neurological deterioration warranting timely operative intervention.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Funayama T, Abe T, Noguchi H, Miura K, Mataki K, Takahashi H. Severe, rigid cervical kyphotic deformity associated with SAPHO syndrome successfully treated with three-stage correction surgery combined with C7 vertebral column resection: A technical case report. Spine Deform. 2021. 9: 285-92
2. Li C, Zuo Y, Wu N, Li L, Li F, Zhang W. Synovitis, acne, pustulosis, hyperostosis and osteitis syndrome: A single centre study of a cohort of 164 patients. Rheumatology (Oxford). 2016. 55: 1023-30
3. Liu S, Tang M, Cao Y, Li C. Synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome: Review and update. Ther Adv Musculoskelet Dis. 2020. 12: 1759720X20912865
4. Magrey M, Khan MA. New insights into synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome. Curr Rheumatol Rep. 2009. 11: 329-33
5. Nakamae T, Yamada K, Tsuchida Y, Adachi N, Fujimoto Y. Synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome with destructive spondylitis: A case report. Spine Surg Relat Res. 2019. 3: 267-9
6. Nakamura J, Yamada K, Mitsugi N, Saito T. A case of SAPHO syndrome with destructive spondylodiscitis suspicious of tuberculous spondylitis. Mod Rheumatol. 2010. 20: 93-7
7. Okuno H, Watanuki M, Kuwahara Y, Sekiguchi A, Mori Y, Hitachi S. Clinical features and radiological findings of 67 patients with SAPHO syndrome. Mod Rheumatol. 2018. 28: 703-8
8. Rekik S, Slouma M, Sahli H. Spinal cord compression: An infrequent complication of SAPHO syndrome. Turk J Rheumatol. 2015. 30: 247-52
9. Sallés M, Olivé A, Perez-Andres R, Holgado S, Mateo L, Riera E. The SAPHO syndrome: A clinical and imaging study. Clin Rheumatol. 2011. 30: 245-9
10. Takigawa T, Tanaka M, Nakahara S, Sugimoto Y, Ozaki T. SAPHO syndrome with rapidly progressing destructive spondylitis: Two cases treated surgically. Eur Spine J. 2008. 17: S331-7
11. Takigawa T, Tanaka M, Nakanishi K, Misawa H, Sugimoto Y, Takahata T. SAPHO syndrome associated spondylitis. Eur Spine J. 2008. 17: 1391-7