- Department of Neurosurgery, Desert Regional Medical Center, Palm Springs, California, United States.
- University of Texas Medical Branch at Galveston, Galveston, Texas, United States,
- School of Medicine, Anahuac Querétaro University, Santiago de Querétaro, México,
- College of Human Medicine, Michigan State University, East Lansing, Michigan, United States.
- William Beaumont School of Medicine, Oakland University, Rochester, Michigan, United States.
- School of Medicine, University of New Mexico, Albuquerque, New Mexico, United States.
Correspondence Address:
Brian Fiani
School of Medicine, University of New Mexico, Albuquerque, New Mexico, United States.
DOI:10.25259/SNI_165_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Brian Fiani1, Thao Doan2, Claudia Covarrubias3, Jennifer Shields4, Manraj Sekhon5, Alexander Rose6. Determination and optimization of ideal patient candidacy for anterior odontoid screw fixation. 19-Apr-2021;12:170
How to cite this URL: Brian Fiani1, Thao Doan2, Claudia Covarrubias3, Jennifer Shields4, Manraj Sekhon5, Alexander Rose6. Determination and optimization of ideal patient candidacy for anterior odontoid screw fixation. 19-Apr-2021;12:170. Available from: https://surgicalneurologyint.com/surgicalint-articles/10737/
Abstract
Background: Odontoid process fractures are one of the most common spine fractures, especially in patients over age 70. There is still much controversy over the ideal candidate for anterior odontoid screw fixation (AOSF), with outcomes affected by characteristics such as fracture morphology, nonideal body habitus, and osteoporosis. Therefore, this systematic review seeks to discuss the optimal criteria, indications, and adverse postoperative considerations when deciding to pursue AOSF.
Methods: This investigation was conducted from experiential recall and article selection performed using the PubMed electronic bibliographic databases. The search yielded 124 articles that were assessed and filtered for relevance. Following the screening of titles and abstracts, 48 articles were deemed significant for final selection.
Results: AOSF is often utilized to treat Type IIB odontoid fractures, which has been shown to preserve atlantoaxial motion, limit soft-tissue injuries/blood loss/vertebral artery injury/reduce operative time, provide adequate osteosynthesis, incur immediate spinal stabilization, and allow motion preservation of C1 and C2. However, this technique is limited by patient characteristics such as fracture morphology, transverse ligament rupture, remote injuries, short neck or inability to extend neck, barrel chested, and severe spinal kyphosis, in addition to adverse postoperative outcomes such as dysphagia and vocal cord paralysis.
Conclusion: Due to the fact that odontoid fractures have a significant morbidity in elderly population, treatment with AOSF is generally recommended for this population with higher risk for nonoperative fusion. Considerations should be made to achieve fracture stability and fusion, while lowering the risk for operative and postoperative complications.
Keywords: Cervical fusion, Odontoid fracture, Odontoid screw fixation, Spinal fixation, Traumatic spinal injury
INTRODUCTION
Anterior odontoid screw fixation (AOSF) is a cervical spine surgical procedure that usually utilizes an anteromedial approach to implement one or two screws for fusion of primarily Type II odontoid fractures.[
Approaches to intervention for odontoid fractures have varied from nonoperative management with cervical collar, Minerva, cervicothoracic orthoses, and halo orthosis to operative management such as AOSF or posterior atlantoaxial stabilization.[
However, different parameters must be considered for predicting success of fusion for Type 2 odontoid fractures utilizing the anterior screw fixation approach. For example, displacement <4 mm and those >6 mm have been associated with improved and lowered fusion rates, respectively.[
PATIENT SELECTION
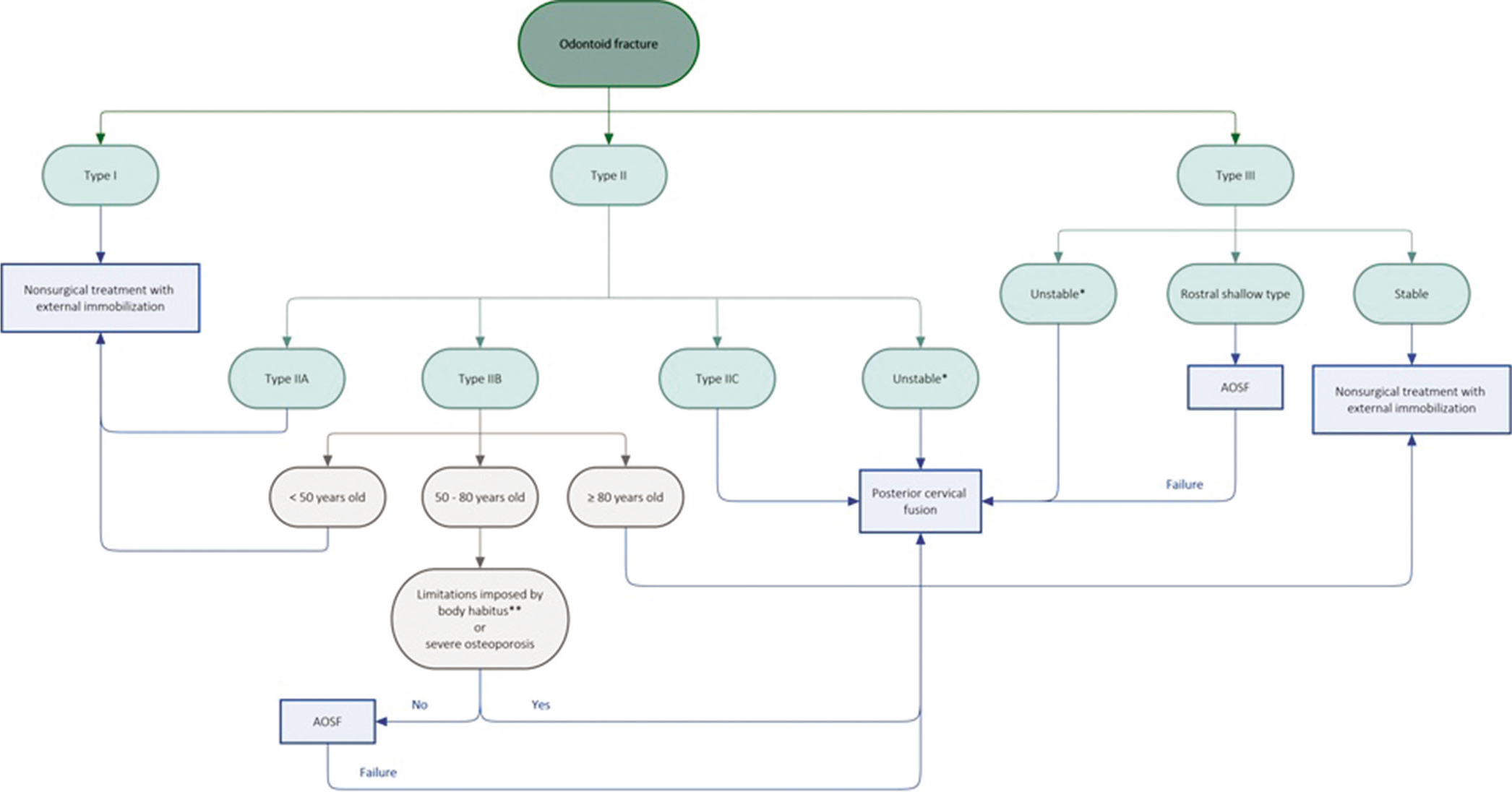
Determination of appropriate surgical candidates for AOSF must take into account many individual, clinical, and radiological features. Based on current literature, a proposed algorithm for the patient selection process [
Figure 1:
Proposed algorithm for the patient selection process to guide treatment of odontoid fractures for use in conjunction with clinical judgment. *Criteria of instability: fracture age greater than or equal to 6 months post-injury, fracture comminution, concomitant disruption of transverse ligament, nonreducible or malaligned fracture, dens displacement greater than or equal to 6 mm, angulation greater than or equal to 10 degrees, or fracture gap greater than or equal to 2 mm. **Criteria for body habitus limitations: fixed cervical or thoracic kyphosis, short neck, or barrel-shaped chest imposing restrictions for proper patient positioning and anterior neck access in AOSF. AOSF, Anterior odontoid screw fixation.
Beyond age, other patient factors, such as comorbidities and functional dependence, bone quality, and especially body habitus, may influence medical suitability for surgery and postoperative outcome and, thus, should be considered when performing a clinical assessment to determine the best treatment approach for odontoid fractures. In patients with significantly reduced bone mineral density, strength, and healing potential, as seen in patients with severe osteoporosis, attaining adequate fixation and fusion are challenging and considered a contraindication given the high possibility for nonunion.[
Postoperative complications may occur as a result of surgical technique that has the potential to affect quality of life. Primarily, these are dysphagia or inability to swallow, as well as damage to the recurrent laryngeal nerve, causing dysphonia or vocal cord paralysis.[
BRIEF OVERVIEW OF TECHNIQUES
Patients are placed under general anesthesia and positioned supine on the operating table. Anterior-posterior and lateral fluoroscopy are used to visualize the C2 vertebral body, odontoid process, and lateral masses of C1. Reduction is achieved using skull traction and flexion or extension maneuvers to position the head before stabilizing with a halter and assessing with fluoroscopy. The C5-6 level is identified and marked using the thyroid and cricoid cartilage preoperatively, then a transverse skin incision is made. The standard Smith-Robertson method is used to expose the prevertebral space by retracting the carotid sheath laterally and the trachea and esophagus medially. The anterior-inferior margin of C2 is exposed, and a Kirschner wire is drilled down the anterior-inferior edge of C2 to the midline of the dens on the opposite apical cortical bone using fluoroscopy. A guide wire is inserted centrally then a cannulated screw is inserted along the guide wire into the C2 body and posterior odontoid process. Fluoroscopy is used to confirm spinal stability.[
Careful selection of patients is necessary for surgery success. The integrity and grade of atlantal transverse ligament damage must be assessed, because atlantoaxial stability cannot be achieved with a single odontoid screw fixation if the ligament is damaged.[
TRIALS, OUTCOMES, AND EFFECTIVENESS
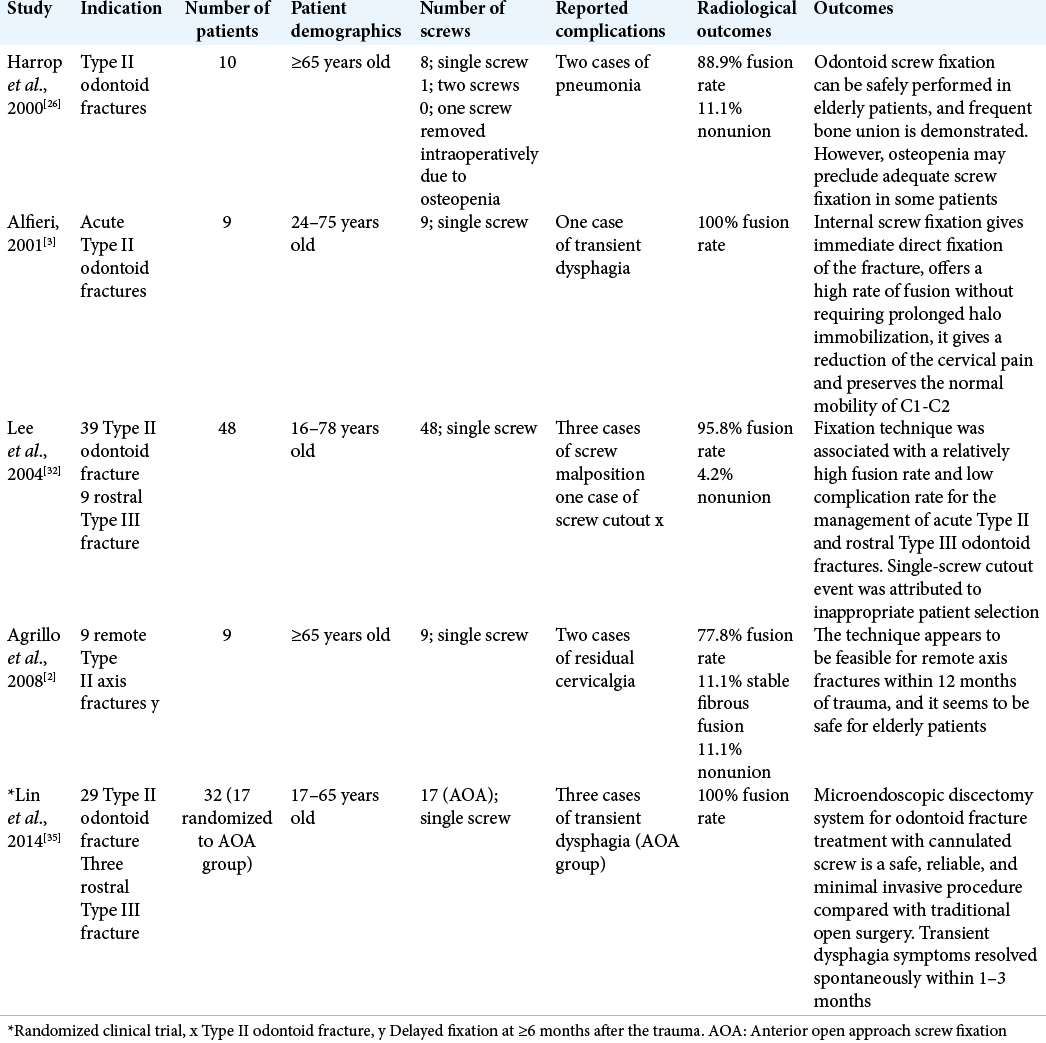
Current available data have demonstrated that AOSF is a feasible treatment for Type II and shallow Type III odontoid fractures, providing immediate stabilization with high fusion rates and preserved C1-2 rotation [
Higher incidence of nonunion is observed in both fractures that are displaced by more than 6 mm, particularly posteriorly, as well as in geriatric patients.[
CONCLUSION
AOSF requires appropriate patient selection to minimize morbidity, maximize fusion rates, and avoiding reduction of range of motion. Because odontoid fractures have a significant morbidity in elderly population, treatment with AOSF is generally recommended for this population with higher risk for nonoperative fusion. Contraindications of anterior screw fixation mentioned in the literature include short neck, concomitant thoracic kyphosis, severe osteopenia, barrel chest deformity, disrupted transverse atlantoaxial ligament, and significant cervical kyphosis. Other factors that can be considered as contraindications include an unfavorable fracture plane angulation from anterior caudal to posterior rostral and inability to obtain an anatomical fracture reduction. Considerations should be made to achieve fracture stability and fusion, while lowering the risk for operative and postoperative complications especially those in relation to functionality and quality of life. Future studies, in particular randomized controlled trials and observational studies with larger patient sample size, should be conducted to further clarify appropriate patient selection and operative technique.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aebi M, Etter C, Coscia M. Fractures of the odontoid process. Treatment with anterior screw fixation. Spine (Phila Pa 1976). 1989. 14: 1065-70
2. Agrillo A, Russo N, Marotta N, Delfini R. Treatment of remote Type II axis fractures in the elderly: Feasibility of anterior odontoid screw fixation. Neurosurgery. 2008. 63: 1145-50
3. Alfieri A. Single-screw fixation for acute Type II odontoid fracture. J Neurosurg Sci. 2001. 45: 15-8
4. Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974. 56: 1663-74
5. Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000. 93: 227-36
6. Böhler J. Anterior stabilization for acute fractures and non-unions of the dens. J Bone Joint Surg Am. 1982. 64: 18-27
7. Chi YL, Wang XY, Xu HZ, Lin Y, Huang QS, Mao FM. Management of odontoid fractures with percutaneous anterior odontoid screw fixation. Eur Spine J. 2007. 16: 1157-64
8. Chiba K, Fujimura Y, Toyama Y, Fujii E, Nakanishi T, Hirabayashi K. Treatment protocol for fractures of the odontoid process. J Spinal Disord. 1996. 9: 267-76
9. Cho DC, Sung JK. Analysis of risk factors associated with fusion failure after anterior odontoid screw fixation. Spine (Phila Pa 1976). 2012. 37: 30-4
10. Cho DC, Sung JK. Is all anterior oblique fracture orientation really a contraindication to anterior screw fixation of Type II and rostral shallow Type III odontoid fractures?. J Korean Neurosurg Soc. 2011. 49: 345-50
11. Cho SK, Lu Y, Lee DH. Dysphagia following anterior cervical spinal surgery: A systematic review. Bone Joint J. 2013. 95B: 868-73
12. Clark CR, White AA. Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985. 67: 1340-8
13. Dailey AT, Hart D, Finn MA, Schmidt MH, Apfelbaum RI. Anterior fixation of odontoid fractures in an elderly population. J Neurosurg Spine. 2010. 12: 1-8
14. Elgafy H, Dvorak MF, Vaccaro AR, Ebraheim N. Treatment of displaced Type II odontoid fractures in elderly patients. Am J Orthop (Belle Mead NJ). 2009. 38: 410-6
15. Fehlings MG, Arun R, Vaccaro AR, Arnold PM, Chapman JR, Kopjar B. Predictors of treatment outcomes in geriatric patients with odontoid fractures: AOSpine North America multi-centre prospective GOF study. Spine (Phila Pa 1976). 2013. 38: 881-6
16. Fountas KN, Kapsalaki EZ, Karampelas I, Feltes CH, Dimopoulos VG, Machinis TG. Results of long-term follow-up in patients undergoing anterior screw fixation for type II and rostral Type III odontoid fractures. Spine (Phila Pa 1976). 2005. 30: 661-9
17. Geisler FH, Cheng C, Poka A, Brumback RJ. Anterior screw fixation of posteriorly displaced Type II odontoid fractures. Neurosurgery. 1989. 25: 30-7
18. Gokaslan ZL, Bydon M, De la Garza-Ramos R, Smith ZA, Hsu WK, Qureshi SA. Recurrent laryngeal nerve palsy after cervical spine surgery: A multicenter AOSpine clinical research network study. Global Spine J. 2017. 7: 53S-7S
19. Gornet ME, Kelly MP. Fractures of the axis: A review of pediatric, adult, and geriatric injuries. Curr Rev Musculoskelet Med. 2016. 9: 505-12
20. Grauer JN, Shafi B, Hilibrand AS, Harrop JS, Kwon BK, Beiner JM. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005. 5: 123-9
21. Greene KA, Dickman CA, Marciano FF, Drabier J, Drayer BP, Sonntag VK. Transverse atlantal ligament disruption associated with odontoid fractures. Spine (Phila Pa 1976). 1994. 19: 2307-14
22. Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine (Phila Pa 1976). 1997. 22: 1843-52
23. Guzman JZ, Feldman ZM, McAnany S, Hecht AC, Qureshi SA, Cho SK. Osteoporosis in cervical spine surgery. Spine (Phila Pa 1976). 2016. 41: 662-8
24. Hadley MN, Browner C, Sonntag VK. Axis fractures: A comprehensive review of management and treatment in 107 cases. Neurosurgery. 1985. 17: 281-90
25. Hanigan WC, Powell FC, Elwood PW, Henderson JP. Odontoid fractures in elderly patients. J Neurosurg. 1993. 78: 32-5
26. Harrop JS, Przybylski GJ, Vaccaro AR, Yalamanchili K. Efficacy of anterior odontoid screw fixation in elderly patients with Type II odontoid fractures. Neurosurg Focus. 2000. 8: e6
27. Henry AD, Bohly J, Grosse A. Fixation of odontoid fractures by an anterior screw. J Bone Joint Surg Br. 1999. 81: 472-7
28. Joaquim AF, Patel AA. C1 and C2 Spine Trauma. Contemp Spine Surg. 2010. 11: 1-7
29. Joaquim AF, Patel AA. Surgical treatment of Type II odontoid fractures: Anterior odontoid screw fixation or posterior cervical instrumented fusion?. Neurosurg Focus. 2015. 38: E11
30. Khattab MF, Nageeb Mahmoud A, Saeed Younis A, ElHawary Y. A simple technique for easier anterior odontoid screw fixation. Br J Neurosurg. 2019. 33: 135-9
31. Konstantinou DLevi ADSonntag VKDickman CA. Odontoid Screw Fixation. Available from: https://www.barrowneuro.org/for-physicians-researchers/education/grand-rounds-publications-media/barrow-quarterly/volume-13-no-2-1997/odontoid-screw-fixation [Last accessed on 2021 Jan 31].
32. Lee SC, Chen JF, Lee ST. Management of acute odontoid fractures with single anterior screw fixation. J Clin Neurosci. 2004. 11: 890-5
33. Lee TK, Han MS, Lee SK, Moon BJ, Lee JK. Outcomes of patients undergoing anterior screw fixation for odontoid fracture and analysis of the predictive factors for surgical failure. Neurospine. 2020. 17: 603-9
34. Lennarson PJ, Mostafavi H, Traynelis VC, Walters BC. Management of Type II dens fractures: A case-control study. Spine (Phila Pa 1976). 2000. 25: 1234-7
35. Lin B, Lu C, Yu H, Zhang W, Yang W. Comparison of microendoscopic discectomy system and anterior open approach in treatment of unstable odontoid fracture with cannulated screw internal fixation. Acta Orthop Belg. 2014. 80: 529-36
36. Lipson SJ. Fractures of the atlas associated with fractures of the odontoid process and transverse ligament ruptures. J Bone Joint Surg Am. 1977. 59: 940-3
37. Lobo JP, Moutinho VV, Serdoura AF, Oliveira CF, Pinho AR. Anterior fixation of odontoid fractures: Results. Rev Bras Ortop. 2018. 53: 532-6
38. Lvov I, Grin A, Talypov A, Godkov I, Kordonskiy A, Khushnazarov U. The impact of odontoid screw fixation techniques on screw-related complications and fusion rates: A systematic review and meta-analysis. Eur Spine J. 2021. 30: 475-97
39. Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: A death sentence?. J Trauma. 2005. 59: 350-6
40. Munakomi S, Tamrakar K, Chaudhary PK, Bhattarai B. Anterior single odontoid screw placement for Type II odontoid fractures: Our modified surgical technique and initial results in a cohort study of 15 patients. F1000Res. 2016. 5: 1681
41. Nakanishi T. Internal fixation of the odontoid fracture. Cent Jpn J Orthop Trauma Surg. 1980. 23: 399-406
42. Platzer P, Thalhammer G, Krumboeck A, Schuster R, KutschaLissberg F, Zehetgruber I. Plate fixation of odontoid fractures without C1-C2 arthrodesis: Practice of a novel surgical technique for stabilization of odontoid fractures, including the opportunity to extend the fixation to C3. Neurosurgery. 2009. 64: 726-33
43. Scheyerer MJ, Zimmermann SM, Simmen HP, Wanner GA, Werner CM. Treatment modality in Type II odontoid fractures defines the outcome in elderly patients. BMC Surg. 2013. 13: 54
44. Smith HE, Kerr SM, Maltenfort M, Chaudhry S, Norton R, Albert TJ. Early complications of surgical versus conservative treatment of isolated Type II odontoid fractures in octogenarians: A retrospective cohort study. J Spinal Disord Tech. 2008. 21: 535-9
45. Song KJ, Lee KB, Kim KN. Treatment of odontoid fractures with single anterior screw fixation. J Clin Neurosci. 2007. 14: 824-30
46. Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006. 60: 199-203
47. Tian NF, Hu XQ, Wu LJ, Wu XL, Wu YS, Zhang XL. Pooled analysis of non-union, re-operation, infection, and approach related complications after anterior odontoid screw fixation. PLoS One. 2014. 9: e103065
48. Vasudevan K, Grossberg JA, Spader HS, Torabi R, Oyelese AA. Age increases the risk of immediate postoperative dysphagia and pneumonia after odontoid screw fixation. Clin Neurol Neurosurg. 2014. 126: 185-9